In patients with benign paroxysmal positional vertigo, BPPV; a torsional-vertical down beating positioning nystagmus can be elicited in the supine straight head-hanging position test or in the Dix-Hallpike test to either side. This type of nystagmus can be explained by either an anterior canal BPPV or by an apogeotropic variant of the contralateral posterior canal BPPV Until now all the therapeutic maneuvers that have been proposed address only one possibility, and without first performing a clear differential diagnosis between them.
ObjectiveTo propose a new maneuver for torsional-vertical down beating positioning nystagmus with a clear lateralization that takes into account both possible diagnoses (anterior canal-BPPV and posterior canal-BPPV).
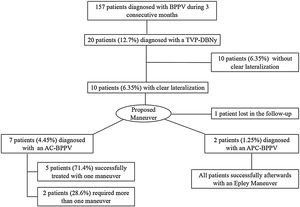
MethodsA prospective cohort study was conducted on 157 consecutive patients with BPPV. The new maneuver was performed only in those with torsional-vertical down beating positioning nystagmus with clear lateralization.
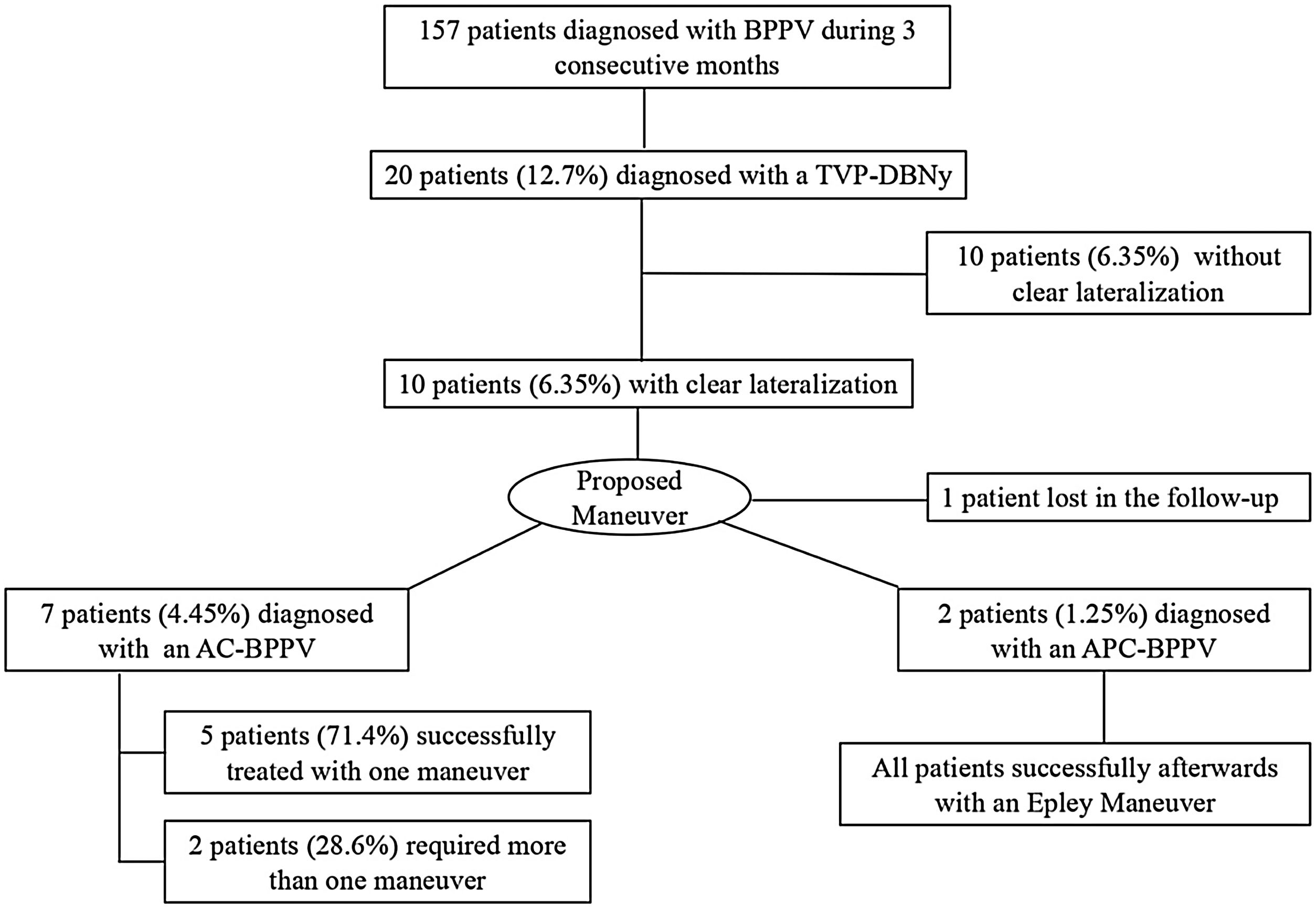
ResultsTwenty patients (12.7%) were diagnosed with a torsional-vertical down beating positioning nystagmus. The maneuver was performed in 10 (6.35%) patients, in whom the affected side was clearly determined. Seven (4.45%) patients were diagnosed with an anterior canal-BPPV and successfully treated. Two (1.25%) patients were diagnosed with a posterior canal-BPPV and successfully treated with an Epley maneuver after its conversion into a geotropic posterior BPPV.
ConclusionThis new maneuver was found to be effective in resolving all the cases of torsional-vertical down beating positioning nystagmus-BPPV caused by an anterior canal-BPPV, and in shifting in a controlled way the posterior canal-BPPV cases of the contralateral side into a geotropic-posterior-BPPV successfully treated during the followup visit. Moreover, this new maneuver helped in the differential diagnosis between anterior canal-BPPV and a contralateral posterior canal-BPPV.
Benign paroxysmal positional vertigo (BPPV) is one of the most common and treatable causes of peripheral vertigo, in which one or more semicircular canals are abnormally stimulated by loose otoconia displaced from the otolith organs.1 Through head movements with respect to gravity, free otoconia activate the semicircular canal afferents, producing a false perception of head rotation and eliciting the corresponding nystagmus.2
During clinical examination of some patients with a history of BPPV, a nystagmus beating predominantly downward but with a small torsional component in which the upper pole of the eye beats toward the affected ear, called torsional-vertical down beating positioning nystagmus (TVP-DBNy), can be elicited in the supine straight head-hanging (HH) position test or in the Dix-Hallpike (DH) test to either side. In the context of BPPV, that type of nystagmus can be explained by either an anterior canal BPPV (AC-BPPV) or by an apogeotropic variant of the posterior canal BPPV (APC-BPPV).1,3–5
AC-BPPV accounts approximately 3%–12% of all BPPV variants.6,7 Although vertigo and nystagmus can be provoked by a DH or a HH test, the latter seems to be the most suitable as the head reaches a more dependent position and the canal is closest to the mid-sagittal plane though extremely curved.7–9 In the HH position free otoconia in the anterior canal (AC) drift away from the cupula, producing an excitatory response and consequently the clinical examination will reveal a TVP-DBNy. The torsional component is usually less intense than the vertical, probably due to the proximity of the AC to the sagittal plane (41°) when compared to the posterior canal (56°),9,10 and its presence provides a localizing clue.11 In AC-BPPV, latency is typically absent and the nystagmus is fatigable,3 however a short latency and a long duration nystagmus have also been described.4 When returning to the sitting position some authors have described a lack inversion of the down-beating vertical nystagmus,3,4 while others described an inversion in the 42% of cases.7
APC-BPPV accounts approximately 2.5% of BPPV forms.3 In this variant of BPPV, loose otoconia are localized in the distal part of the non-ampullary arm of the posterior canal (PC), near the common crus. When HH or DH tests are performed, otoconia move towards the cupula producing an ampullopetal endolymphatic flow and therefore an inhibitory discharge of the posterior ampullary nerve.4 The APC-BPPV is characterized by a paroxysmal positioning nystagmus in the opposite direction to the one evoked in typical (geotropic) posterior canal BPPV: a TVP-DBNy. The linear component is down-beating, and the torsional component is towards the unaffected ear (upper pole of the eye beating to the left for the right canal, and to the right for the left canal), similar to contra-lateral AC-BPPV.5 In APC-BPPV the nystagmus is mainly vertical, has no latency, when raising up to the upright position does not always reverse its direction, and the a torsional component is not always clear.3–5
As previously mentioned TVP-DBNy can be caused by either an AC-BPPV or an APC-BPPV, but in a patient it is very difficult to differentiate the AC from the PC variant and accordingly the side. Until now all the therapeutic maneuvers that have been proposed address only one possibility, and without first performing a clear differential diagnosis between them.4,9,12–15
Different maneuvers have been proposed for the treatment of AC-BPPV when the pathologic side is identified such as the Rahko maneuver,12 the reverse Epley,14 or the maneuver described by Kim et al.13 In 2009, Yacovino and Hain proposed a maneuver that works symmetrically for both anterior canals, regardless of which side is affected.9 On the other hand, the literature is scarce regarding the treatment of APC-BPPV. Califano et al. in 2014 described the use of a maneuver named “quick liberatory rotation maneuver”, which is similar to the Epley maneuver with the difference that the rotation of the head in the horizontal plane is followed by the trunk, and also movements are carried out very quickly.15 Also, Vannucchi proposed a maneuver in 2015 based on the Semont maneuver named as “Demi-Semont”.4
We propose here a new maneuver for TVP-DBNy when it is possible to determine the affected side. This maneuver is designed to remove the debris through the common crus in AC-BPPV; but in case of contralateral APC-BPPV, the same maneuver will shift in a controlled way the debris from the non-ampullary arm into the ampullary arm of the contralateral posterior canal, turning it into a geotropic posterior anal BPPV (PC-BPPV).
MethodsPatients and methodsA prospective cohort study was conducted on 157 consecutive patients diagnosed with BPPV during three consecutive months (December 2019–February 2020) in the neurotology clinic of our department. Only patients with TVP-DBNy and diagnosed with an AC-BPPV using the diagnostic criteria established by the Bárány Society in 2015 were included in the analysis.16
All patients underwent a routine neurotologic examination that included eye position, ocular motility, spontaneous and gaze-evoked nystagmus with and without visual fixation, headshaking-induced nystagmus or vibration-induced nystagmus and the clinical visual suppression and visual-vestibular interaction tests. The VOR was tested both clinically and with the video head-impulse test (the 6 semicircular canals). Dynamic position tests were orderly performed first the HH position test, then the supine, left and right lateral and finally the DH test. All tests were assessed and recorded using a videonystagmograph (VNG) system (VideoFrenzel Interacoustics VF505m) except the DH test, for which common Frenzel goggles were used. Audiometry was performed when indicated and all subjects were evaluated with a brain MRI.
The exclusion criteria were multicanal BPPV and central vestibular pathology according to findings in the clinical exam or MRI.17 This was a high resolution thin-slice temporal bone MRI with special focus on brainstem and cerebellum. Institutional review board approval and informed consent from all patients were obtained.
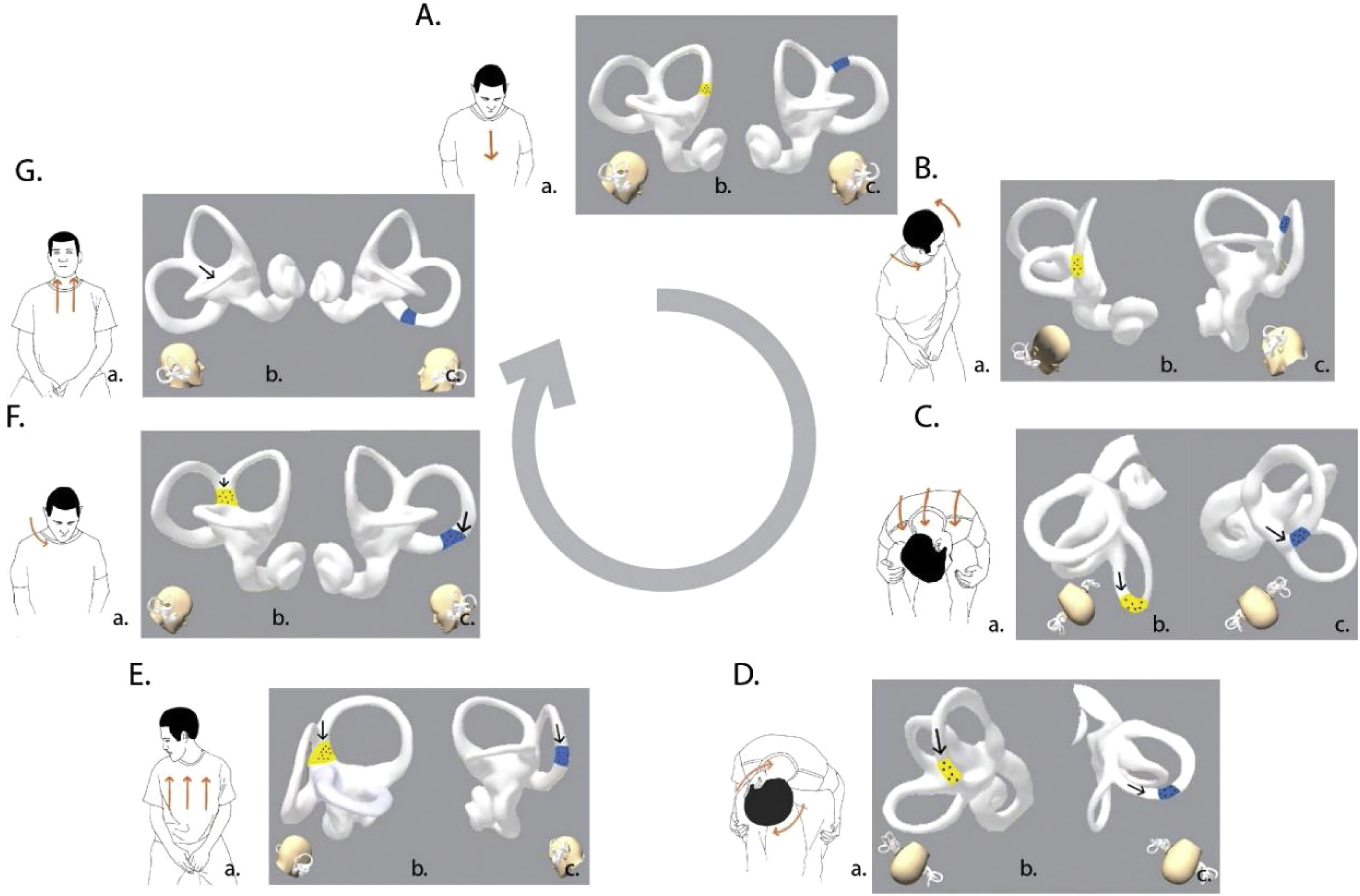
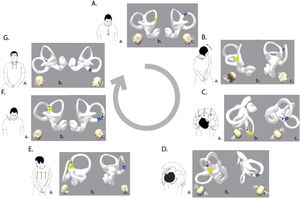
Particle repositioning maneuverOur repositioning maneuver is illustrated in Fig. 1. In order to perform this maneuver, and decide the “affected side”, we assumed in all cases that TVP-DBNy was triggered by an AC-BPPV. This maneuver is designed to use both inertial and gravitational force to move debris though the canal. The following steps were systematically followed:
Novel maneuver for the torsional-vertical down beating positioning nystagmus (TVP-DBNy) in patients with BPPV. In this example during the clinical examination, the patient revealed a DBN (Down Beating nystagmus) with a RBT (torsional component the upper pole of the eye beating towards the right or counterclockwise from examiner’s perspective). TVP-DBNy is assumed to be triggered by an AC-BPPV on the right side (Otoconia position and movement are highlight in yellow) or an APC-BPPV on the left side (Otoconia position and movement are highlight in blue). During all the steps of the maneuver, the nystagmus remains the same, because the otoconia and the endolymphatic flow follows the same direction and therefore the same response (ampullofugal/excitatory in AC-BPPV or ampullopetal/inhibitory in APC-BPPV). A and B (Step I), C (Step II), D (Step III), E (Step IV), F and G (Step V), DBN.
Step I: The maneuver starts with the patient in the sitting position with the back vertical at 0° and the head bowed approximately a 45° angle (Fig. 1Aa), Next, the patient’s head is rotated towards the unaffected side (Fig. 1Ba). This position places the AC of the affected side, and the PC of the unaffected in the sagittal plane. (Fig. 1Bb–Bc).
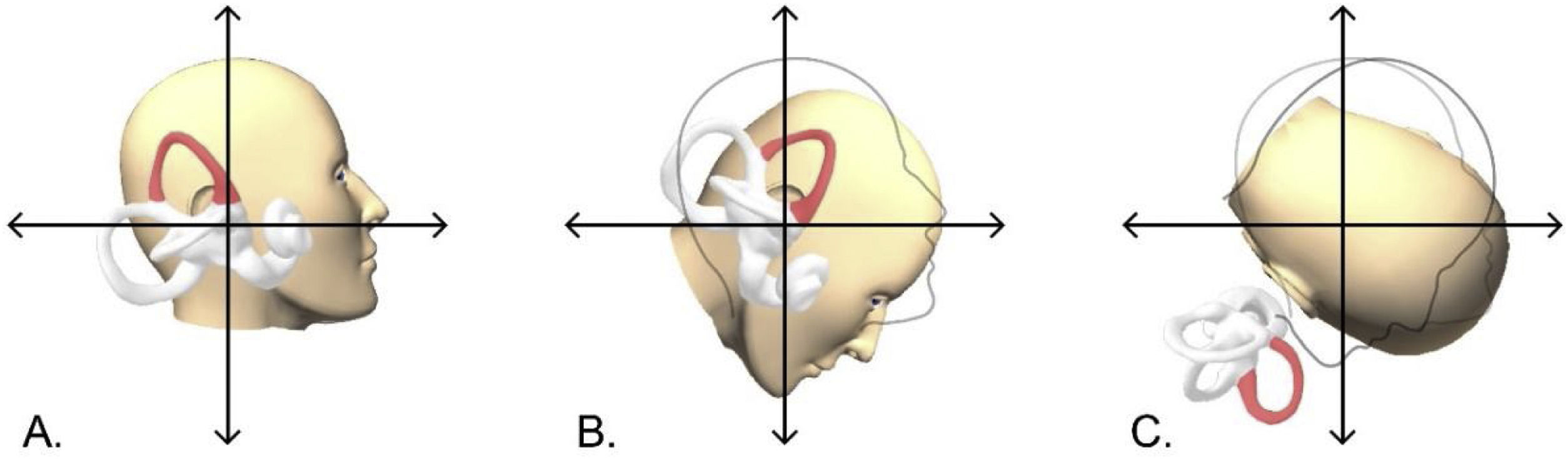
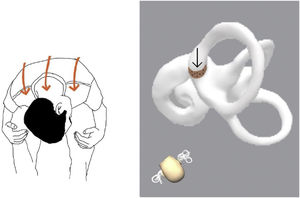
Step II: The patient is quickly bent forward 90° through a flexion of the lumbar spine and hips until the head reaches the height of the knees (Fig. 1Ca). With this movement, the inner ear labyrinth will be at a 90° forward bending;18 if we add the 45° of head forward flexion Step I, the cupula of the AC will now be at 135° forward bending.18–20 (Fig. 2) In this position, loose otoconia in the AC will be displaced towards the lowest gravitational point of the canal, first using the inertia generated by the deceleration of the movement and then by gravity (Fig. 1Cb). In the case of a contralateral APC-BPPV, loose otoconia will be displaced towards the lower gravitational point of the non-ampullary arm of the PC by the same mechanisms (Fig. 1Cc). This position is maintained for 1 min.
Right anterior canal spatial positioning during Stage I and II. A, Patient’s head in sitting position (0°). B, Patient’s head after forward flexion (45°). C, Patients head after rotation towards the left side and flexion of the lumbar spine and hips (90°). The right anterior canal cupula reaches approximately a 135° forward rotation.
Step III: The patient’s head is slowly rotated towards the affected side (Fig. 1Da). This rotation induces the displacement of otoconia by gravity towards the common crus (Fig. 1Db). In the case of a contralateral APC-BPPV, the otoconia will reach the lowest gravitational point of the canal (Fig. 1Dc). This position is maintained for 1 min.
Step IV: With the head rotated towards the affected side, the patient is now brought to the sitting position with vertebral column at 0° in a single rapid movement (Fig. 1. Ea). Now the otoconia will be displaced into the common crus (Fig. 1 Eb). In the case of a contralateral APC-BPPV, they will reach the ampullary arm of the posterior canal (Fig. 1Ec).
Step V: The patient’s head is slowly rotated towards the midline (Fig. 1Fa) and is then elevated into a neutral position (Fig. 1Ga). Loose otoconia will be moved out into the utricle (Fig. 1Gb), and in the case of a contralateral APC-BPPV, will get closer to the ampulla of the PC (Fig. 1Gc).
ResultsIn the study period 20 patients (12.7%) were diagnosed TVP-DBNy. The maneuver was performed in 10 (50%) patients, in whom the affected side was clearly determined (Fig. 3). Nine were females (90%) and one was male (10%), the mean age was 59 years, and 7 (70%) had a previous history of BPPV. Among the patients with previous history of BPPV, 5 (71.4%) remained asymptomatic since the last episode/maneuver (mean of 21.25 months). Two patients (28.6%) remained partially symptomatic since the last episode/maneuver. Patient nº 2 had a right Epley maneuver performed 7 days before and patient nº 9 had also a right Epley maneuver performed 15 days before the assessment.
In the HH position down beating nystagmus was seen in 9 patients with different direction in the torsional component except for 1 (patient nº 4). In 4/9 patients the same nystagmus was seen in the HH test and both right and left DH tests (patients nº 1, nº 7, nº 8, and nº 9); in 3/9 patients the HH test finding was similar when the DH test was performed on just one side (2 were the affected and 1 in the non-affected side) (patients nº 2, nº 5, and nº 10); In 2/9 patients nystagmus was seen only the HH or DH test respectively (patients nº 3 and nº 4). In 1/10 patient (patient nº 4) the HH test was negative and the finding was obtained while performing the left sided DH test. Reversal of nystagmus upon siting was observed in 3 patients (30%) during DH and/or HH tests (Table 1).
Clinical characteristics of patients with torsional vertical down beating positioning nystagmus BPPV.
| Nº | Sex | Age | Previous history of BPPV | HH | R-DH | L-DH | SU | Diagnosis strategy | Follow-up time (days) | Symptoms | Nystagmus | Final diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 79 | Yes | LBT + DBN | LBT + DBN | LBT + DBN | – | Left AC- BPPV | 3 | No | No | Left AC- BPPV |
| 2 | F | 36 | Yes | LBT + DBN | – | LBT + DBN | – | Left AC- BPPV | 8 | No | No | Left AC- BPPV |
| 3 | M | 66 | Yes | RBT + DBN | – | – | – | Right AC- BPPV | 11 | No | No | Right AC- BPPV |
| 4 | F | 66 | Yes | – | – | RBT + DBN | LBT + UBN | Right AC- BPPV | 2 | Yes | PC–BPPV | Left APC -BPPV |
| 5 | F | 81 | No | LBT + DBN | – | LBT + DBN | – | Left AC- BPPV | 7 | No | No | Left AC- BPPV |
| 6 | F | 46 | No | DBN | – | LBT + DBN | RBT + UBN | Left AC- BPPV | 3 | Yes | PC–BPPV | Right APC - BPPV |
| 7 | F | 44 | No | LBT + DBN | LBT + DBN | LBT + DBN | – | Left AC- BPPV | 2 | Yes | TVP–DBNy | Left AC- BPPV |
| 8 | F | 72 | Yes | RBT + DBN | RBT + DBN | RBT + DBN | UBN + LBT | Right AC- BPPV | 12 | Yes | TVP–DBNy | Right AC- BPPV |
| 9 | F | 41 | Yes | RBT + DBN | RBT + DBN | RBT + DBN | – | Right AC- BPPV | 6 | No | No | Right AC- BPPV |
| 10 | F | 59 | Yes | LBT + DBN | LBT + DBN | – | – | Left AC- BPPV | – | – | – | – |
BPPV: Benign paroxysmal positional vertigo; F: Female; M: Male; HH: Head Hanging test; R-DH: Right Dix-Hallpike; L-DH: Left Dix-Hallpike; SU: Sitting up position; LBT: torsional component the upper pole of the eye beating towards the left or clockwise from examiner’s perspective; RBT: torsional component the upper pole of the eye beating towards the right or counterclockwise from examiner’s perspective; DBN: Down Beating nystagmus; UBN: Upper beating nystagmus; AC: Anterior canal BPPV; APC: apogeotropic variant of posterior canal BPPV; PC: geotropic-posterior canal; TVP-DBNy: torsional-vertical down beating positional nystagmus.
Of the 10 patients here included, 1 was lost to followup. Five (55.56%) patients improved their symptoms and the nystagmus disappeared in the first medical followup (mean time to followup: 5.4 days). In 2 (22.22%) patients, symptoms and the same nystagmus (TVP-DBNy) persisted in the followup visit. A new maneuver was performed: patient nº 7 required a second maneuver and patient nº 8 a third maneuver until their symptoms and the nystagmus disappeared. In two patients (22.22%) at followup symptoms persisted but nystagmus was seen only in the DH test now when performed on the contralateral side, and accordingly were diagnosed of an APC-BPPV (patients nº 7 and nº 8). As in followup nystagmus was now consistent with a canalolithiasis in the ampullar arm, an Epley maneuver was successfully performed in both cases.
DiscussionIn our work, we have described a novel method to treat AC-BPPV, which also may be useful to carry out the differential diagnosis between AC-BPPV and the APC-BPPV variant. Both possible diagnoses were taken into account when designing the maneuver.
This study has some limitations. The main limitation is that the variants here considered are unusual and, in the case of the AC-BPPV, even controversial. Down-beat nystagmus is not an infrequent finding when complete vestibular examination is performed in patients with vertigo. Previous authors have noted that this type of nystagmus is linked to BPPV in approximately 50% of the patients,17 and that it needs a high index of suspicion to achieve a final diagnosis. In our study down-beat nystagmus was the only finding in 12.7% of patients seen for a confirmed BPPV. This is probably related to the sequence of the examination, which we always began with the HH test. A second limitation was that in order to be able to perform this maneuver, the affected side must be identified; that has been shown to occur in 33%–78% of patients.21,22 In the present study, among 20 patients with TVP-DBNy the affected side was identified in only 10 (50%) of them.
With regard to our study population, the results of the clinical examination similar to the ones described by Yang et al.7 in 40 patients with AC-BPPV. Yang described that nystagmus was obtained in all patients in the HH test (down-beat nystagmus with/without torsional component) and in 42.5% during bilateral DH tests, and that nystagmus reversed direction upon sitting up in 42.5% of patients. In our study those values were 90%, 40% and 30% respectively.
Regarding the frequency of the nystagmus and differential diagnosis some comments are needed. During a clinical evaluation, elucidating whether the presence of TVP-DBNy in patients with a typical history of BPPV is caused either by an AC-BPPV or an APC-BPPV on the contralateral side is very difficult and unlikely to happen in practice. Califano proposed a differential diagnosis between both etiologies based on the clinical examination.3 Besides the torsional component to differentiate a right from left AC-BPPV, and a right from left APC-BPPV, he defined the diagnosis of AC-BPPV as certain when the nystagmus was evoked through the HH test and sometimes through the DH test, and the diagnosis of APC-BPPV as certain when the nystagmus was evoked through the DH test and sometimes through the HH test. This approach might be somewhat inaccurate because previous studies have described that both etiologies can be triggered through both tests,5,7,9,23 and this is consistent with our results. But what is most important, and the key element in order to differentiate both etiologies, is how to distinguish a right AC-BBPV from a left APC-BPPV and vice versa, and that was not accurately defined by Califano. We propose that the best way to approach a TVP-DBNy is to consider both variants as possible triggers, and this strategy can be achieved with our proposed maneuver.
In our study confirmed AC-BPPV (after the maneuver) was found to be 4.45%, similar to the incidence describe by other authors which is approximately between 3% and 5%.6,24 However, if we include the cases in which the etiology of the TVP-DBNy could not be determined (1 of them lost followup and 10 with unclear lateralization), the incidence increases to 11.45%. If we assume those cases as AC-BPPV, the incidence could also be similar to higher incidences described, such as 12.1%.7 On the other, the incidence of confirmed APC-BPPV (after the maneuver) was found to be 1.27%. It is important to highlight that the diagnosis was made after the maneuver, which converted in a controlled way the APC-BPPV cases into PC-BPPV. Vannucchi described an incidence of 6.25% of APC-BPPV, and also emphasized the misdiagnosis of this variant as an AC-BPPV, when he noted that patients diagnosed witch AC-BPPV would come back to the next checkup with a typical PC-BPPV of the opposite side.5 Our APC-BPPV incidence could be 8.27% if we include the rest of the cases with unclear lateralization. Therefore, one question that results from this study is whether we are presently making an accurate diagnosis of AC-BPPV, or we are just assuming that all TVP-DBNy are caused by an AC-BPPV. It is interesting to highlight that two patients underwent replacement maneuvers prior to proposed maneuver (patients nº 2 and nº 9). The partial persistence of symptoms and the short time since the last maneuver could suggest that these atypical forms of BPPV could be considered as a complication of a previous maneuver.
Several manual reduction methods have been described for treating AC-BPPV when the affected side is identified, such as Rahko,12 the reverse Epley14 or Kim13 maneuver. All of these have been designed without taking into account a possible APC-BPPV in the contralateral ear, and except for Kim´s maneuver, there are no published data concerning their efficacy. Also, these maneuvers are performed in a supine position, and in some parts of the procedure, the head is in a hanging position, and it is turned in a manner similar to the way PC-BPPV is treated.12–14 The AC follows a different trajectory from the PC, therefore maneuvers to treat AC-BPPV must necessarily differ geometrically from those described for the PC.9 Since the PC is the most stimulated and assessed in the DH test, it is relevant to assume that the AC is better stimulated and assessed during a bending forward movement.18 The Yacovino-Hain maneuver works symmetrically for unilateral AC-BPPV, regardless of which side is affected.9 If we do not take into account the affected ear, TVP-DBNy can be triggered by loose otoconia in four semicircular canals: both ACs (AC-BPPV) and both PCs (APC-BPPV). By performing this maneuver we are assuming that the problem is in only one AC, and even if both ACs were affected, we are blindly hoping to liberate loose otoconia without knowing exactly where they are, since they could be in any of the four canals. Like the previous ones, the Yacovino-Hain maneuvers do not take into account the possibility of APC-BPPV involvement, and uncontrolled conversions into a PC-BPPV after performing the maneuver have been described.3,7 Its success rate is between 44.4% and 84.6%,7,25 and some patients will need an additional maneuver to achieve a clinical resolution.3,7,9 We also recommend to repeat our maneuver until either symptoms and nystagmus disappear, or until a PC-BPPV in the contralateral side is diagnosed. The proposed maneuver might be difficult to carry out in obese patients, nevertheless it can be a good option for elderly patients and those with limitation of neck mobility.
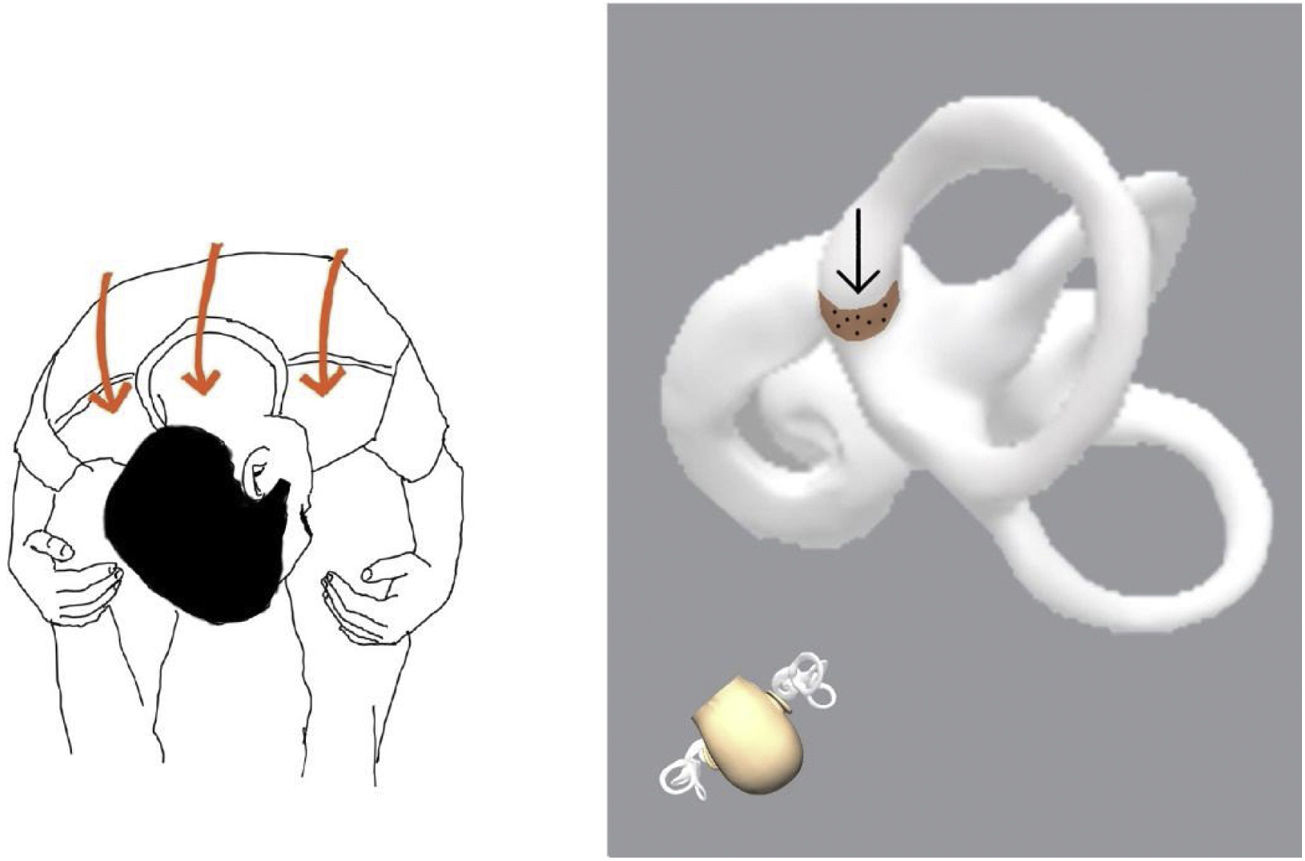
When it comes to the posterior canal BPPV, we have to take into account very unusual variants, such as the “short arm” canalithiasis.26 In this hypothetical variant, during the DH test, there is either no movement of the otoconia debris or one in an ampullofugal direction. While in the HH test, otoconia movement generates an ampullopetal endolymphatic flow with reversal upon sitting (even this could be the only registered effect) similar to an APC-BPPV.27,28 In this (otherwise hypothetical) situation, the second step of our maneuver (Fig. 4) would transfer the otoconia from the short arm towards the utricle, following the same principle of the Ostrich maneuver described by Fath et al. for the PC “short arm” canalithiasis.28
The bend forward test has been recently described as a diagnostic tool in the assessment of AC-BPPV by Iglebekk et al.18 The same group described a maneuver called “forward somersault” maneuver,20 in which the patient is turned 360° forwardly. Similarly, to the Yacovino-Hain maneuver it works for both sides, but it does not take into account a possible APC-BPPV Additionally it requires a specialized movable chair and is therefore unlikely to be very clinically practical.
Although this is a small and uncontrolled cohort study, this new maneuver was effective in resolving all the cases of TVP-DBNy caused by an AC-BPPV, and in shifting in a controlled way the APC-BPPV cases of the contralateral side into a geotropic-posterior-BPPV successfully treated during the followup visit. This maneuver could be useful in patients with a TVP-DBNy with a clear lateralization, as an alternative to the Yacovino-Hain maneuver.
Conflicts of interestThe authors declare no conflicts of interest.
To Esteban Župan for the help provided in the design of the illustrations.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.