In its normal anatomy, the common carotid artery (CCA) originates in the brachiocephalic trunk on the right and directly from the aortic arch on the left.1 The CCA then ascends in the neck, up to the upper border of the thyroid cartilage, where it bifurcates. In the cervical region, the common carotid arteries are located one on each side, anterolaterally in the neck, being subsequently related to the cervical sympathetic chain, with the transverse apophyses of the cervical vertebrae and are covered by the pre-vertebral muscles and deep cervical aponeurosis.2
The internal carotid artery (ICA) originates at the CCA bifurcation, which shows an ascending path towards the base of the skull, without originating any branches. However, several anatomical variations are reported in its path. Post-mortem statistics indicate that the incidence of such variations is between 10% and 40% of the population, being usually bilateral. The origin of the different variations is controversial. Some are believed to represent congenital vascular anomalies and others are related to arteriosclerotic diseases or fibromuscular dysplasias.3,4
The ICA alterations, although frequent, can be silent and have a close association with the pharyngeal space.5 When symptomatic, these alterations usually manifest in the posterior pharyngeal wall and, therefore, are clinically relevant in the context of otorhinolaryngological surgeries such as tonsillectomy, drainage of peritonsillar abscesses, as well as adenoidectomies and pharyngeal lesion biopsies.3 Alterations in the CCA are rarer, but no less important, since the height of its bifurcation, the diameter of thickness and the degree of tortuosity are of the utmost importance for interventions and surgeries in the cervical topography.1
In elderly patients, dysphagia, dysphonia, cervical foreign body sensation and glossopharyngeal neuralgia may occur and can be associated with arteriosclerotic and thrombotic events, causing blood flow impairment to the brain.4
The investigation and exclusion of vascular anomalies is extremely important in the preoperative period of surgical procedures, aiming to avoid very severe iatrogenic events. This study, therefore, aims to demonstrate a rare case of multiple anomalies in the path of the CCA and ICA on the right, which enter regions that are frequently accessed in otorhinolaryngological and head and neck surgeries.
Case reportOAS, a 75-year-old male patient, ex-smoker, with hypertension and emphysema, came in July 2019 to the Otorhinolaryngology Outpatient Clinic of a referral hospital in the midwest of Brazil, complaining of dysphonia for 4 years, associated with heartburn and dysphagia for fluids, with no improvement after conventional anti-reflux treatments carried out in another service. No alterations were identified at the otorhinolaryngological physical examination. According to the medical history, the patient had undergone two microsurgery procedures for a laryngeal lesion biopsy in 2017.
His reports of previously performed exams included: videolaryngoscopy (VL) in 2015, with evidence of injury to the right vocal fold, ultrasonography (USG) in 2015 showing no alterations, videolaryngealstroboscopy (VLS) in 2016, showing right vocal fold apparently infiltrated with diminished mucosal wave and a lesion with leukoplastic aspect in the middle third, with signs of laryngopharyngeal reflux (LPR); the VL in 2017 (post-biopsy) showed decreased left vocal fold mobility. At the time of the first consultation, it was decided to request the results of the biopsies performed in previous surgical approaches to the vocal folds, as well as a new VL and computed tomography (CT) of the neck with contrast, due to the alteration in vocal fold mobility associated with the observation of slight asymmetry in the supraglottic region, to rule out the possibility of an infiltrative tumor in that region or the presence of storage disease. Treatment for LPR was prescribed as adjunctive therapy and speech therapy was recommended.
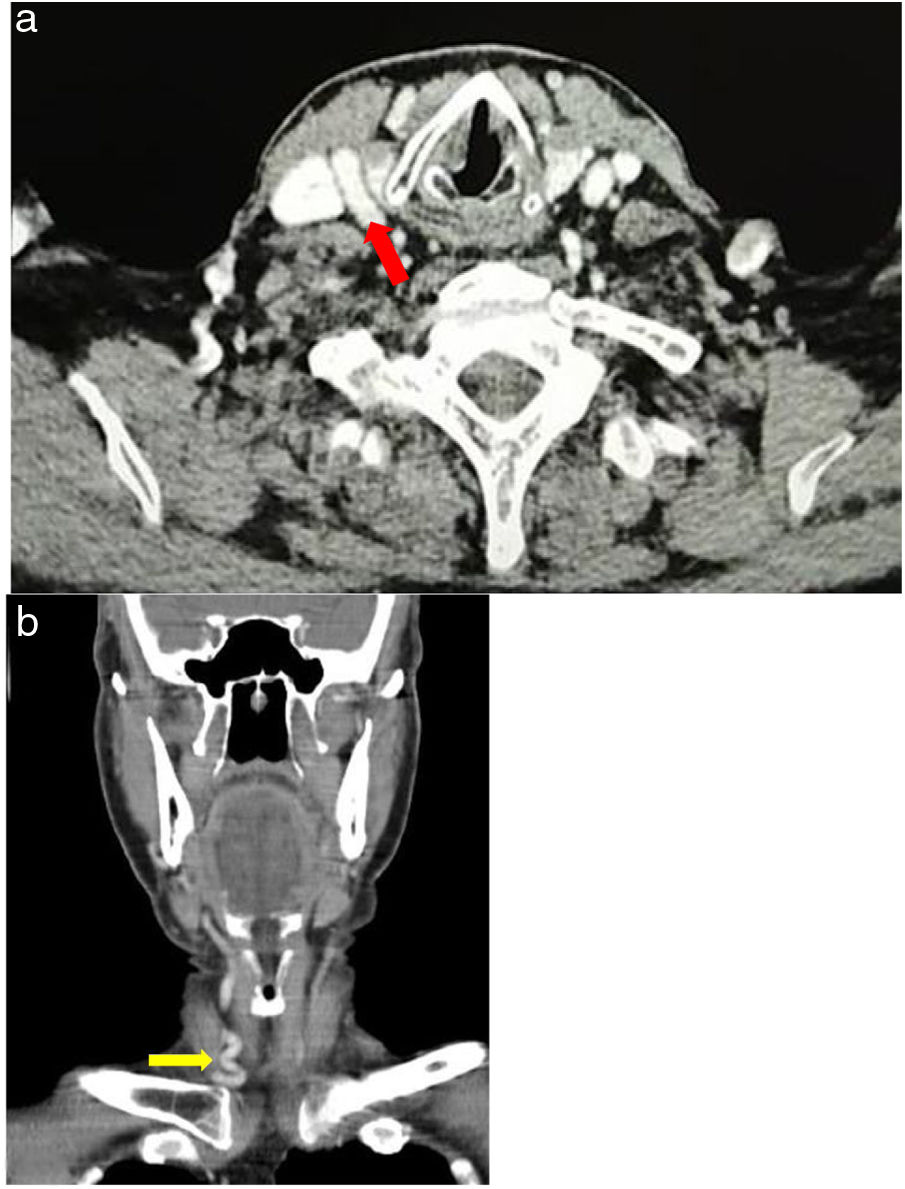
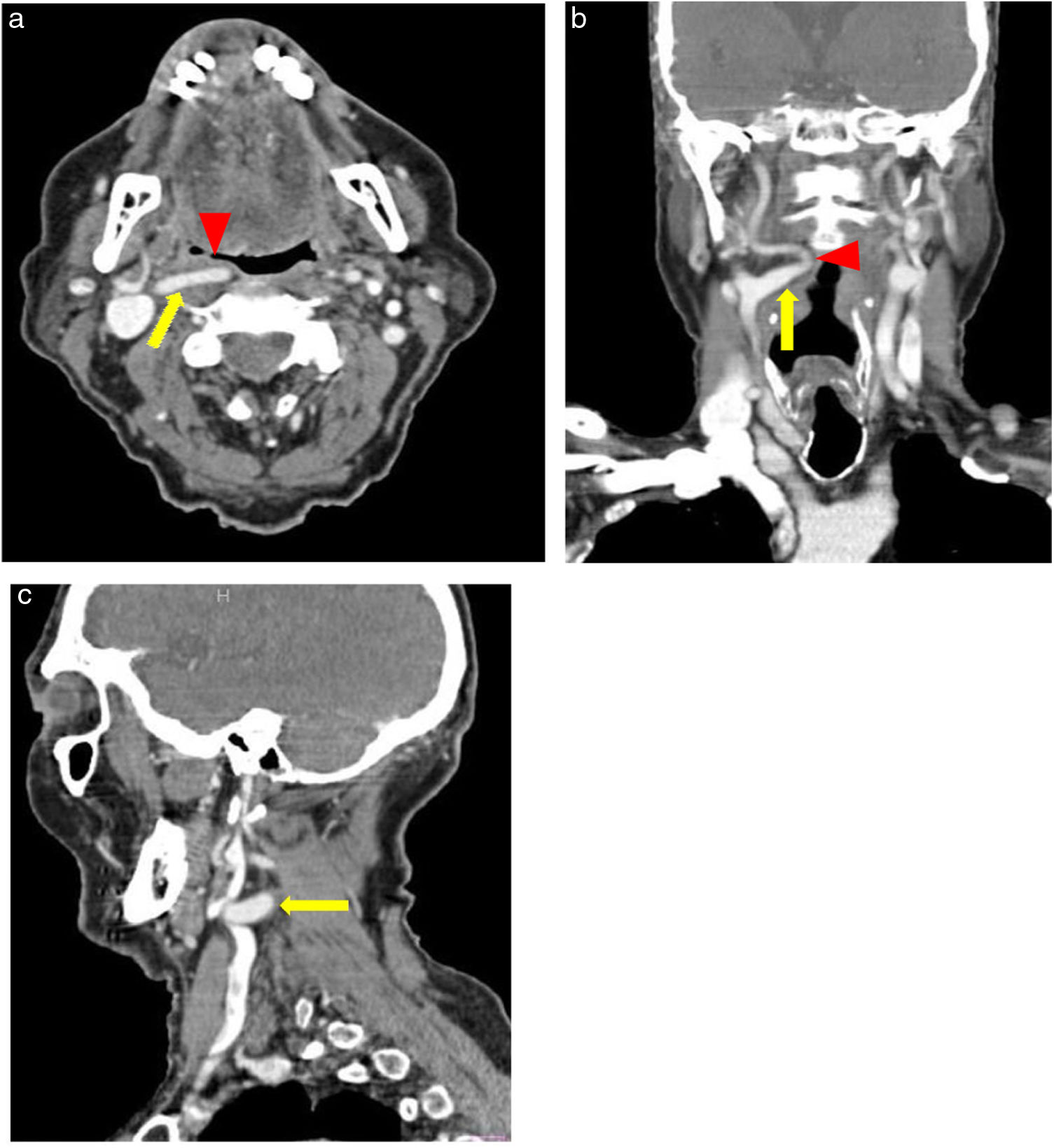
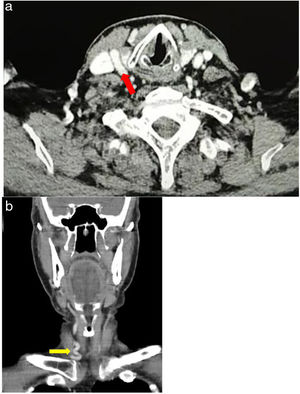
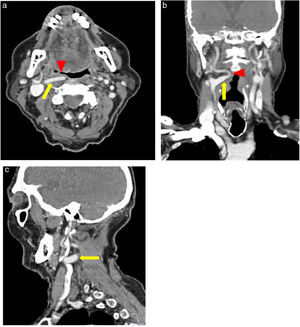
The patient returned with the requested exams for an outpatient consultation, during which the anatomopathological examination of 2017 showed a diagnosis of vocal cord cyst. The VL performed in 2020 showed persistent signs of LPR, chronic laryngitis and presence of vocal cleft. The contrast CT of the neck disclosed several anatomical variations in the carotid artery, from its common part with marked tortuosity on the right (Fig. 1) and aberrant path of the internal carotid artery also on the right, showing medial “kinking” at approximately 2.0cm from the carotid bifurcation, causing an impact on the right posterior lateral wall of the oropharynx, without reducing the air column (Fig. 2). In the laryngeal region, soft tissue content was identified, partially occupying the pyriform sinus and right piriform sinus distention. The patient was referred to the vascular surgeon and informed of the risks of inadvertent interventionist measures on the head and neck.
Common carotid artery (CCA) showing a tortuous path in the cervical Computed Tomography, with contrast. (a) Axial section at the larynx glottic level, showing the infrahyoid carotid space, which contains the CCA (red arrow), the internal jugular vein and the vagus nerve (not visible). (b) Coronal section showing the CCA tortuous path (yellow arrow), above its origin in the right brachiocephalic trunk.
Internal carotid artery showing an aberrant path on the cervical CT scan, with contrast. (a) Axial section showing a variation in the trajectory of the internal carotid artery (ICA) in the parapharyngeal space (yellow arrow), which is medialized and bulging the right posterolateral wall of the oropharynx (red arrowhead). (b) Coronal section showing the right ICA with an aberrant path, with medial “kinking” and serpiginous aspect (yellow arrow) associated with pharyngeal bulging (red arrowhead). (c) Sagittal section showing ICA kinking (yellow arrow).
Vascular anomalies of the common carotid artery or its internal branch should always be included in the differential diagnosis of pharyngeal wall bulging, with the most common being tortuosity, “kinking” and “coiling”.3,5 Injuries to these arteries can have catastrophic consequences and, therefore, it is sensible to carry out a careful preoperative assessment in patients who are candidates for otorhinolaryngological surgical procedures.5
In the present case, the patient had previously undergone two laryngeal biopsies on another service when he came for evaluation at our service. The inadvertent performance of biopsies or punctures in cases like the one described herein could lead to fatal outcomes, especially since the parapharyngeal space is a difficult region to be evaluated only clinically, due to its deep location in the cervical region.6,7
In the presence of lesions causing atypical bulges on the larynx or pharynx wall, it is essential to request imaging tests, such as CT, MRI and angiography, as they allow a more accurate assessment.5 Considering the costs and availability, the contrasted CT can be of great value in the investigation. In this context, the arteriography should be indicated for masses that need further clarification.6
Usually the described alterations are asymptomatic. However, there may be reductions in blood supply to the brain, depending on the movement of the head and neck and possible compression of other important structures. Patients may experience pharyngeal bulging and pulsation, in addition to pharyngeal foreign body sensation and odynophagia.8 The actual incidence of hemorrhage due to carotid aberration is unknown.9 However, given that the CCA bifurcates at the upper level of the thyroid cartilage and at the cervical C4 and C5 vertebral level, path abnormalities considerably increase the chances of arterial injury, highlighting the need for caution also in surgical approaches to the thyroid.10
The parapharyngeal space contains important structures, such as the internal carotid arteries, maxillary and inferior alveolar arteries, the internal jugular vein, the lingual nerves, the temporal auricle, the cranial nerve pairs numbers IX, X, XI and XI, the cervical sympathetic trunk and several lymph nodes. It is worth mentioning that, given the anatomical proximity of important cervical structures in the parapharyngeal space, complaints of dysphagia and dysphonia may occur due to the presence of tumors that lead to compression of the vagus nerve (X pair).6 In the reported case, the patient complained of dysphagia, which is not suspected by the chronic condition of mucosal alterations in the vocal folds, and the hypothesis of vagus nerve compression may be suspected.
The differential diagnoses include the possibility of carotid aneurysms, lymph node enlargement, pharyngeal tumors, carotid paragangliomas and deep lobe parotid tumors. Although “kinking” may have incapacitating or even fatal cerebral blood flow effects, this is not their typical presentation and the management regarding vascular surgery assessment is usually an expectant one.8
In the case described herein, we chose to perform the imaging investigation with contrasted cervical CT, and after the diagnosis, the patient was referred to vascular surgery, and an expectant management was decided upon with a six month followup.
ConclusionThe knowledge of the anatomy of cervical vessels and their possible variations is of utmost importance for surgeons when planning interventions, guiding a comprehensive preoperative assessment and a safer transoperative period. The importance of requesting imaging tests, such as contrasted cervical CT, is highlighted, helping in the differential diagnosis of tumors, storage diseases and aberrant paths of large cervical vessels, although it is not possible to observe pulsation, as in the case reported herein. Therefore, these exams should be performed in cases of patients with submucosal bulging in the rhino, oro- or hypopharynx regions, as well as with the observation of asymmetries and/or anatomical distortions. Thus, the present study contributes to the improvement in knowledge of the scientific community by reporting a rare manifestation caused by the association of the anomalous path of the carotid artery in its common and internal portions.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.