The Calmette–Guerin Bacillus (BCG), an attenuated live strain of Mycobacterium bovis was originally developed by Albert Leon Charles Calmette and Camile Guerin in 1925 as a vaccine for tuberculosis. At the present, BCG is widely used as a complementary therapy for superficial bladder neoplasms. This treatment is considered to be safe and well tolerated although local and distal complications may appear.1 In 2003, Diaz et al. reported in the Spanish language, for the first time, a case of unilateral infection of the parotid gland caused by BCG.2 We reviewed the English literature from 1975 to 2015 and found no other cases of such infection, as it is extremely rare. In this article we report a well-documented case of a bilateral infection of the parotid glands produced by BCG and discuss the treatment and patient follow-up.
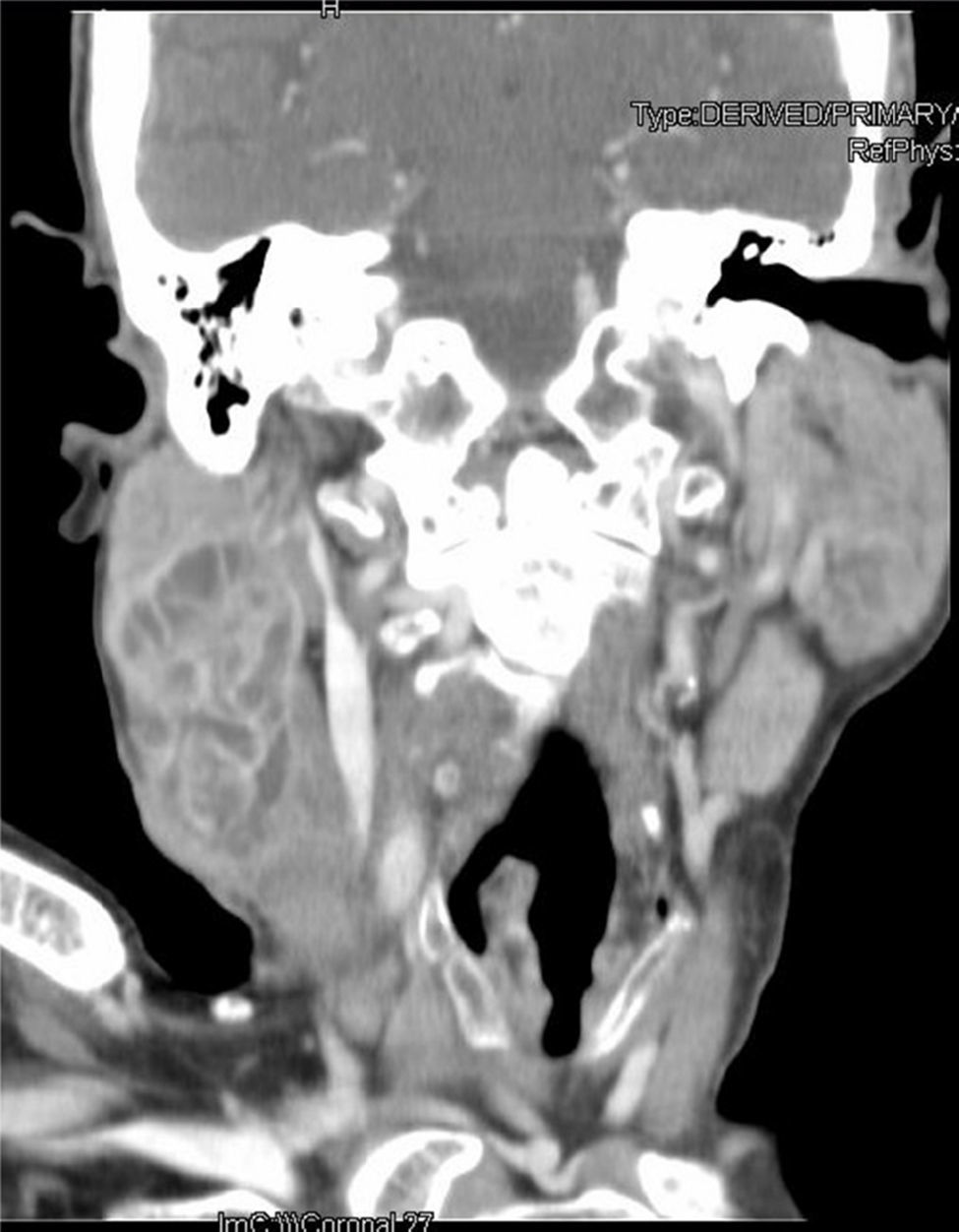
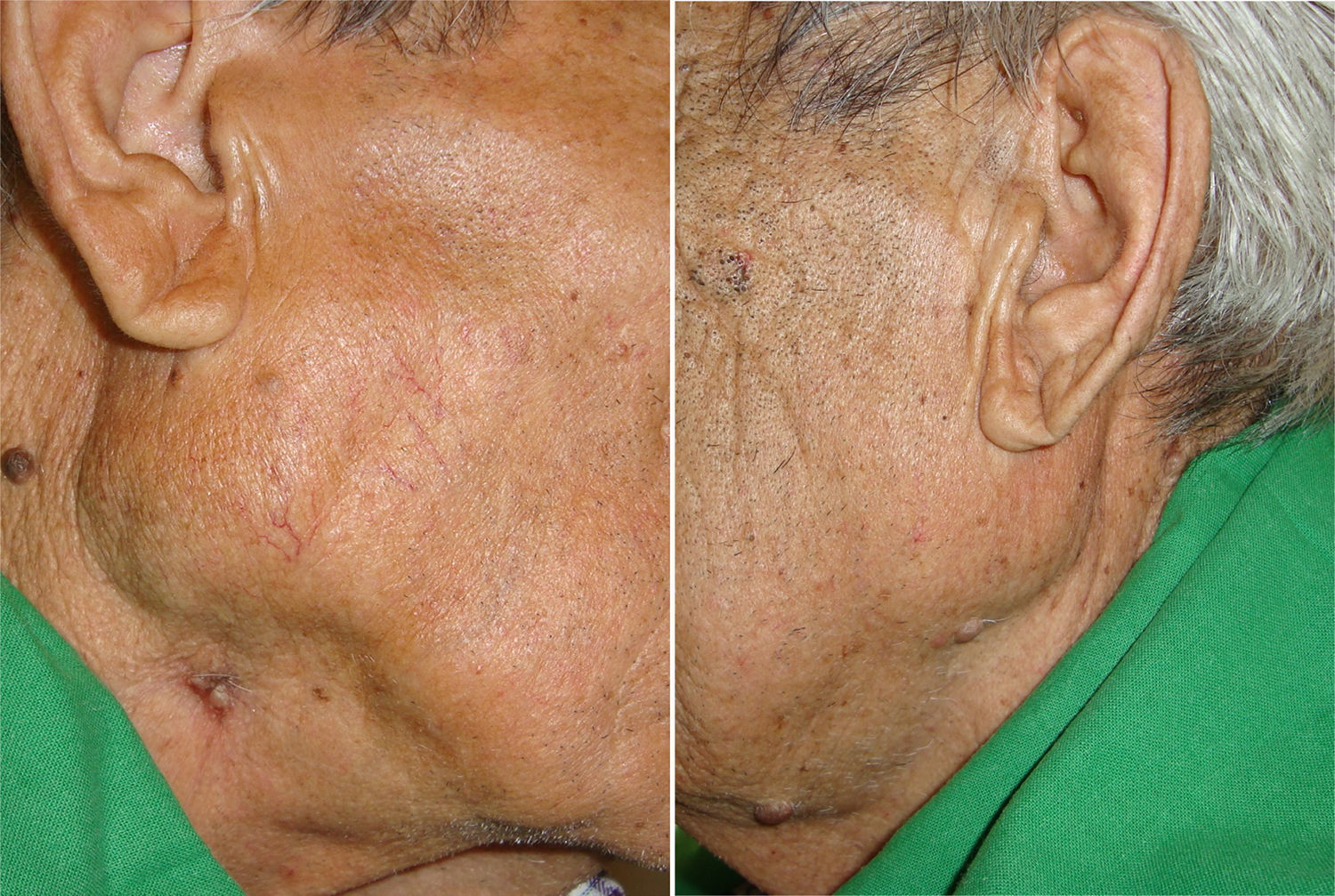
Case reportWe present the case of a 72-years old male with a history of recurrent bladder carcinoma in the last three years. The patient also had a long history of tobacco consumption in the past 30 years. He was referred to our ENT department due to bilateral parotid gland swelling with a small ulcerative lesion on the right gland that had been growing in the previous month. The patient underwent several treatments in the last few years for a recurrent bladder carcinoma. The last treatment consisted of a transurethral resection followed by intravesical instillation therapy with BCG. Treatment ended two month prior to the patient's consultation with our ENT department. The initial physical examination revealed enlargement of both parotid glands, with an elastic consistency. On the inferior pole of the right gland there was a small painless ulcer with continuous pus discharge (Fig. 1). Blood work showed mild anemia with no other findings. An echography-guided puncture of the right lesion was realized and samples were sent for microbiologic testing. An urgent CT scan was then preformed showing a large mass of 6.4cm×3cm×3.6cm, on the right side. The lesion showed multiple trabecular zones with cystic and necrotic areas. The left side showed a 3cm×2cm×2cm lesion with the same characteristics (Fig. 2). Considering age, sex and the smoking history the preliminary suspicion was a bilateral Warthin's tumor. Based on the analysis made by the microbiology department using GeneXpert® (Cepheid), the initial report came back positive for Mycobacterium tuberculosis complex. Given the result and the history of oncologic bladder treatments with BCG, molecular biology procedures (GenoType Mycobacterium CM/AS®, Hain) were performed confirming the presence of the attenuated strain of M. bovis, thus BCG. A scintigraphy was performed to rule out other locations of dissemination of the BCG. Vertebral, renal and pulmonary dissemination areas were found. Patient underwent treatment with Isoniazid 300mg with vitamin B6, ethambutol 800mg and levofloxacin 500mg once daily for 10 month presenting excellent response to the treatment. After 20 month of follow-up patient still had no evidence of disease, confirmed by CT scans and fiscal examination and blood tests. The swelling of the parotid glands completely disappeared as well as the ulcerative lesion on the right side (Fig. 3).
Tuberculosis affecting salivary glands is a rare type of extrapulmonar tuberculosis, being the parotid gland the most frequent location in these cases. This entity may be misdiagnosed as a neoplasm, as the clinical course is usually the same: a localized and progressive, chronic swelling of the gland. Sometimes it can even cause facial palsy, mimicking a malignant tumor. In our case the bilateral affection in an elder smoker man should include Warthin's tumor as a frequent possible diagnosis, as it appears as a painless, cystic, slow-growing mass which mainly affects the parotid gland. In 15% of cases it can involve both glands, and it does not usually become malignant.
Due to the similar clinical characteristics of parotid tuberculosis and parotid neoplasms, it is of the outmost importance to make a good clinical history asking about any previous cancers or contact with tuberculosis. After the clinical examination, a fine needle aspiration cytology guided by echography is needed, as it is the gold standard technique to differentiate both types of pathologies. Histological and microbiological tests must be run on the tissue sample. Histology testing often shows granulomatous inflammation, while the microbiological diagnosis could be achieved by acid-fast bacilli staining, mycobacterial culture or PCR-based assays. Unfortunately, cultures result negative in 40.9%3 of cases, due to the control of bacillary replication by an immunocompetent host against an attenuated mycobacteria strain. A CT scan may be a helpful tool in achieving the complete diagnosis as it helps determine the extension of the disease and it is used in the follow-up to evaluate the response to the treatment.2
In cases in which the ecography-guided puncture comes up with no clear result, parotidectomy with intraoperative biopsy could be done to rule out malignancy.2
The parotid tuberculosis is thought to be caused by hematogenous or lymphatic dissemination of the bacilli from the lungs or secondary to an oral cavity infection with involvement of the Stenon's duct and the afferent lymphatic vessels.
In our case the patient did not have any contact with M. tuberculosis, but with an attenuated strain of M. bovis, the BCG. Despite its rare incidence, the hematogenous dissemination of the bacilli is possible, and some conditions like immunosuppression, disruption of the urothelial barrier due to traumatic catheterization, concurrent urinary tract infection or early instillation after transurethral resection may promote it.3 The disseminated BCG infection is a different condition from the flu-like symptoms post-instillation and the local complications in the genitourinary tract that can appear during treatment. It is defined as a positive blood or bone marrow culture or evidence of infection at two or more anatomic sites beyond the urinary tract.3 The sites most commonly affected are the lungs and the osteoarticular system,3 being the salivary glands an extremely odd location for the BCG to migrate.
From a therapeutic point of view, this disease can be treated as any other tuberculosis infection with antituberculosis drugs. The BCG is intrinsically resistant to pyrazinamide and cycloserine2,3 so the preferred treatment is a combination of isoniazid, rifampicin or ethambutol. In some cases the BCG strain is susceptible to quinolones so an agent from this group may be added as well.
ConclusionsThe dissemination of BCG to the parotid gland is an extremely rare condition. In cases of bilateral swelling of the parotid glands in elderly patients with a long history of smoking, bilateral Warthin's tumor may be the initial suspicion. A detailed history of the patient must be obtained to achieve differential diagnosis and rule out all possibilities. The use of echography-guided punctures and molecular biology procedures was fundamental in achieving the diagnosis in this case. An interdisciplinary approach and a good collaboration specialist are essential in the management of complexes cases such as this one.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Friedlander E, Pascual PM, de Mora PM, Yurrita BS. Bilateral parotid glands infection caused by Calmette-Guerin Bacillus after intravesical therapy for recurrent bladder cancer: a case report. Braz J Otorhinolaryngol. 2017;83:726–9.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.