Endolymphatic hydrops, the histopathological substrate of Ménière's disease, is an almost universal finding in postmortem studies of patients with this disease. The cause of hydrops is still unknown, as is the mechanism by which it causes progressive dysfunction of the sensory organs of inner ear. The fluctuating course of the disease complicates the interpretation of certain tests, such as electrocochleography; thus, for some authors its diagnostic value is questionable.
ObjectiveThe aim of this study was to analyze the clinical applicability of electrocochleography in the diagnosis of hydrops. It is a valuable tool, but still generates conflicting opinions among otolaryngologists.
MethodsSystematic review of the literature on electrocochleography in patients diagnosed with endolymphatic hydrops.
ResultsA total of 34 articles regarding the use of electrocochleography in patients with hydrops, from the year 2000 onwards, were selected. Of these, 15 were excluded from the review as they were not observational studies. Only one cross-sectional study addressing the clinical use of electrocochleography by otolaryngologists was included.
ConclusionElectrocochleography is a valuable tool in the diagnosis of hydrops, as it is a non-invasive, easy to handle procedure, which offers new techniques to increase the sensitivity of the test, and thereby assists otolaryngologists in the management of Ménière's disease.
A hidropisia endolinfática é o substrato histopatológico e achado quase universal nos estudos post-mortem de pacientes com doença de Ménière. A causa da hidropisia ainda é desconhecida, assim como o mecanismo pelo qual causa disfunção progressiva dos órgãos sensitivos da orelha interna. O curso flutuante da doença dificulta a interpretação de exames como a eletrococleografia, que apresenta, para alguns autores, valor diagnóstico controverso.
ObjetivosO objetivo deste estudo é analisar a aplicabilidade clínica da eletrococleografia no diagnóstico da hidropisia endolinfática, sendo uma ferramenta de uso comum e que ainda gera opiniões conflitantes entre os otorrinolaringologistas.
MétodoRevisão sistemática da literatura sobre eletrococleografia em pacientes com diagnóstico de hidropisia endolinfática.
ResultadosForam selecionados 34 artigos sobre o uso da eletrococleografia em pacientes portadores de hidropisia endolinfática a partir do ano 2000; 15 artigos foram excluídos da revisão por não se tratarem de estudos observacionais, com inclusão de somente um estudo transversal que trata sobre o uso clínico da eletrococleografia entre os otorrinolaringologistas.
ConclusãoA eletrococleografia é uma importante ferramenta no diagnóstico da hidropisia endolinfática, por ser não invasiva, de fácil mensuração, e por oferecer novas técnicas capazes de aumentar a sensibilidade do exame e auxiliar o otorrinolaringologista no tratamento da Doença de Ménière.
Endolymphatic hydrops is the histopathological substrate and an almost universal finding in postmortem studies of patients with Ménière's disease. The cause of hydrops is still unknown, as is the mechanism by which it causes progressive dysfunction of the sensory organs of the inner ear. Various theories have been proposed, and most of them are based on a change in the production or resorption of endolymph.1,2
A family history is present in over 10% of patients, with genetic predisposition, viral infections, autoimmune disease suggesting deposition of circulating immune complexes in the endolymphatic sac and disorders of water homeostasis wherein the aquaporins and vasopressin play an important role.1,2
One hypothesis, widely accepted, is that of Schuknecht: hydrops causes rupture of Reissner's membrane, allowing the potassium-rich endolymphatic fluid to make contact with perilymph, reaching the surface of the hair cells and of the vestibulocochlear nerve, causing hearing loss and vertigo attacks.2 In the advanced stages of endolymphatic hydrops, it is common to find patients with hearing thresholds greater than 50dB. Other theories suggest that even the distension of the basilar membrane by endolymphatic hydrops may already lead to degeneration of hair cells and consequently to their malfunction, causing a decrease in AP.1,2
AAO-HNS diagnostic criteria from 1995 only include clinical and audiometric parameters in the diagnosis of Ménière's disease. According to these criteria, patients with two or more spontaneous episodes of vertigo, with duration equal or greater than 20min, with documented hearing loss on at least one occasion and presence of tinnitus or aural fullness are clinically classified as having Ménière's disease. This diagnosis is considered likely when a defined episode of vertigo occurs in the presence of documented sensorineural hearing loss on at least one occasion, aural fullness, or tinnitus. It is considered as possible in the presence of episodic vertigo of Ménière's type without documented hearing loss or when there is sensorineural, fixed, or fluctuating hearing loss associated to imbalance, without a definite vertigo episode.3
The fluctuating course of the disease complicates the interpretation of tests such electrocochleography; some authors consider it to provide a controversial diagnostic value. Studies show disappointing results for its sensitivity and specificity; however, several instruments can be used to increase the sensitivity of this test. Electrocochleography remains as the only objective tool to measure endolymphatic hydrops in the cochlea.4–8
Electrocochleography registers all three mechanoelectrical potentials of the cochlea; cochlear microphonics is considered as the first step toward neural impulse, reflecting the sum of intracellular potentials generated into the hair cells in the most basal portion of cochlea during its depolarization.4,6,9
Cochlear microphonics is produced by varying the potassium flow in the tectorial plate of hair cells, as a result of rapid ion changes associated with the ciliary movement. At high intensities, the basilar membrane vibrates asymmetrically around its midpoint, and the excessive displacement toward the scala tympani produces a constant direct current (DC) component, the summation potential (SP).4,5,7,9
The generation of the summation potential is controversial. Several authors, such as Hall in 2007 and Durrant et al. in 1998, believe that the inner hair cells perform a key role in generating of SP; some authors, such as Burkand et al., believe that SP is generated by both internal and external hair cells. The action potential is the sum of the synchrony of cochlear nerve's individual neural PAs.4–6
The aim of this study was to analyze the clinical applicability of electrocochleography in the diagnosis of endolymphatic hydrops, since it represents an usual tool that still generates conflicting opinions among otolaryngologists.
MethodsThis was a systematic review of the literature on electrocochleography in patients with endolymphatic hydrops. The PubMed/MEDLINE and BIREME databases were consulted.
The search strategy employed in the literature review was guided by the combination of four descriptors indexed in Descriptors in Health Sciences (DecS) in Brazilian Portuguese: “hidropisia endolinfática,” “doença de Ménière,” “audiometria de resposta evocada,” and “eletrococleografia”; and in Medical Subject Headings (MeSH) in English: “endolymphatic hydrops;” “Ménière's disease;” “audiometry,” and “evoked response.”
The inclusion criteria were: retrospective and prospective studies on humans from the year 2000 on electrocochleography in patients with a diagnosis of endolymphatic hydrops according to Hearing and Balance Committee of the American Academy of Otolaryngology (1995) criteria, published in indexed journals. The inclusion criteria were defined by one of the authors, while the other authors were responsible for the analysis of the articles.
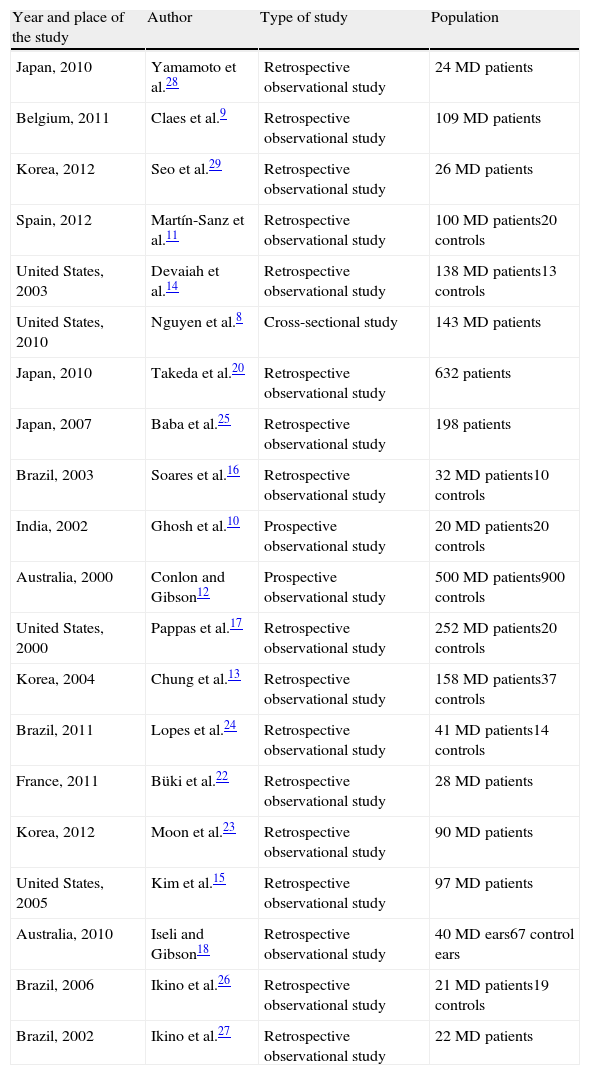
ResultsThirty-four articles on the use of electrocochleography in patients with endolymphatic hydrops were selected from the year 2000 onwards; 15 were excluded from the review because they were not observational studies, and only one cross-sectional study addressing the clinical use of electrocochleography among otolaryngologists was included (Table 1).
Twenty selected studies on the use of electrocochleography.
| Year and place of the study | Author | Type of study | Population |
| Japan, 2010 | Yamamoto et al.28 | Retrospective observational study | 24 MD patients |
| Belgium, 2011 | Claes et al.9 | Retrospective observational study | 109 MD patients |
| Korea, 2012 | Seo et al.29 | Retrospective observational study | 26 MD patients |
| Spain, 2012 | Martín-Sanz et al.11 | Retrospective observational study | 100 MD patients20 controls |
| United States, 2003 | Devaiah et al.14 | Retrospective observational study | 138 MD patients13 controls |
| United States, 2010 | Nguyen et al.8 | Cross-sectional study | 143 MD patients |
| Japan, 2010 | Takeda et al.20 | Retrospective observational study | 632 patients |
| Japan, 2007 | Baba et al.25 | Retrospective observational study | 198 patients |
| Brazil, 2003 | Soares et al.16 | Retrospective observational study | 32 MD patients10 controls |
| India, 2002 | Ghosh et al.10 | Prospective observational study | 20 MD patients20 controls |
| Australia, 2000 | Conlon and Gibson12 | Prospective observational study | 500 MD patients900 controls |
| United States, 2000 | Pappas et al.17 | Retrospective observational study | 252 MD patients20 controls |
| Korea, 2004 | Chung et al.13 | Retrospective observational study | 158 MD patients37 controls |
| Brazil, 2011 | Lopes et al.24 | Retrospective observational study | 41 MD patients14 controls |
| France, 2011 | Büki et al.22 | Retrospective observational study | 28 MD patients |
| Korea, 2012 | Moon et al.23 | Retrospective observational study | 90 MD patients |
| United States, 2005 | Kim et al.15 | Retrospective observational study | 97 MD patients |
| Australia, 2010 | Iseli and Gibson18 | Retrospective observational study | 40 MD ears67 control ears |
| Brazil, 2006 | Ikino et al.26 | Retrospective observational study | 21 MD patients19 controls |
| Brazil, 2002 | Ikino et al.27 | Retrospective observational study | 22 MD patients |
MD, Ménière's disease.
Nguyen et al. evaluated the use of electrocochleography among members of the American Society of Otology and Neurotology American Society and found that, to approximately 50% of participants, electrocochleography has no role in their clinical practice, due to the variability of results and lack of correlation with patients’ symptoms.8
Between 25% and 54% of patients with Ménière's disease produce an electrocochleography with normal results.7,8 In most selected studies on electrocochleography in patients with Ménière's disease, the transtympanic electrode is the most used, with sensitivity rates ranging from 67% to 85%.9–12
Hall reported a sensitivity of 57% and specificity of 94%,5 while Chung et al. reported a sensitivity of 71% and a specificity of 96%.13 Conversely, Devaiah et al. observed a sensitivity of 60%, which reached 92% when the electrocochleography was performed during a symptomatic period.14
Kim et al. examined 60 patients with definite and 37 with probable or possible Ménière's disease. Overall, 59.8% had abnormally high SP/AP ratios. Among patients with definite Ménière's disease, 66.7% had abnormally high SP/AP ratios, while those with probable or possible MD, 52.7% produced an abnormal electrocochleography (p=0.069). These authors concluded that no statistically significant difference was observed in the results of electrocochleography between the definite and probable/possible MD groups. In addition, approximately 30% of people with definite Ménière's disease would not be diagnosed based on electrocochleography results. Due to the low sensitivity, according to Kim et al., electrocochleography should not play a decisive role in determining the diagnosis of Ménière's disease.15
Soares et al. conducted a retrospective study based on 60 electrocochleography studies. SP/AP ratio, the amplitude between the first positive peak of the second component of AP and the baseline, and the amplitude between the second positive peak of the second component of AP and the baseline were analyzed. These authors found that SP/AP ratio was the most sensitive and specific parameter for the identification of patients with endolymphatic hydrops.16
Comparing results from transtympanic versus extratympanic electrocochleography in 20 patients with Ménière's disease and 20 control patients, Ghosh et al. reported a significant difference in SP/AP ratio between cases and controls. For a value of SP/AP=0.29, these authors found a sensitivity of 100% and specificity of 90% for transtympanic and 90% and 80% for extratympanic electrocochleography, respectively, concluding that extratympanic electrocochleography is an effective, easily implemented in clinical practice, and non-invasive method, when compared to the transtympanic method.10
Pappas et al., in a retrospective study, evaluated extratympanic electrocochleography in a group of 252 patients diagnosed with MD and a control group of 20 healthy patients. The group with defined MD showed an increased SP/AP in 74% of cases, the group of possible MD in 64%, and the bilateral MD group in 66%. Contralateral ears showed high ratios in 42% of cases; in 40% of these ears, at least one contralateral symptom was found. These authors concluded that extratympanic electrocochleography plays an important role in cases of possible MD, for which audiological data are scarce.17 This conclusion is corroborated by Chung et al., who, in a retrospective analysis of 158 patients (97 women and 61 men) undergoing extratympanic electrocochleography, obtained a sensitivity of 71% and a specificity of 96% for a SP/AP=0.34, reasserting the role of extratympanic electrocochleography in patients with less-defined symptoms.13
The thresholds of SP/AP ratio vary in the literature. Pappas et al. believed that any result above 0.5 with extratympanic electrocochleography with use of clicks with alternating polarity is suggestive of endolymphatic hydrops,17 while Iseli and Gibson set a value of 0.33 with transtympanic electrocochleography.18
Martín-Sanz et al. observed a sensitivity of 85% and a specificity of 80% for a SP/AP threshold greater than 0.5 with transtympanic electrocochleography, using clicks with alternating polarity. These authors also reported that the sensitivity and specificity of any diagnostic test in Ménière's disease will always be subject to change, depending on the study population.11
Gibson et al. compared results of electrocochleography in ears of patients with Ménière's disease versus healthy ears with similar hearing loss and concluded that the use of clicks to assess SP/AP does not lend itself to such differentiation, but that the use of tonebursts to evaluate SP amplitude is significantly different in these populations.19
Colon and Gibson demonstrated that the sensitivity of transtympanic electrocochleography increases by 85% when 1kHz of toneburst was used to measure SP. These authors reported that most of the experts (58.6%) prefer click stimuli versus 17.2% using tonebursts and 24.3% using both stimuli.12
Claes et al. conducted a retrospective study of 131 results of transtympanic electrocochleography using clicks and tonebursts. These authors found that 91% of patients in the definite Ménière's disease group tested positive for electrocochleography with toneburst stimulation, and that 71% of controls (without Ménière's disease) were negative. Claes et al. combined audiometric and electrocochleographic thresholds and identified 98% of cases of absence of Ménière's disease and 94% of cases of definite Ménière's disease.9
Takeda et al. performed a retrospective study with the use of electrocochleography in 632 patients with symptoms extending over ten years. Among them, 334 patients were diagnosed with Ménière's disease, including 95 cases of bilateral involvement. These authors found an increased SP/AP ratio in 56.3% of patients with MD. They also observed that ears with longer symptomatology and/or with more severe symptoms presented greater abnormalities in the SP/AP ratio. The incidence of SP increase was significantly higher in patients with more than two years of duration of disease, or with several crises by year.20 Ge et al. also agree that patients with a longer disease duration present SP/AP ratio with higher values. They also concluded that the hearing gain after glycerol test resulted in no decrease in SP/AP ratio.21 These authors observed that once PS rises, it persists for long periods, even in cases of vertigo and of hearing loss remission – data corroborated by Kim et al. and Pappas et al.15,17
Büki et al., in a retrospective study, analyzed results of electrocochleography after vertigo control by intratympanic injection of gentamicin and observed that the SP/AP ratio measured by electrocochleography did not exhibit statistically increases in the absence of symptoms. The elevation of SP amplitude in ears with endolymphatic hydrops appears to depend mainly on the mechanoelectrical transduction process into the cochlea, due to the loss of hair cells or to potassium poisoning of the perilymph, instead of the mechanical factor of the displacement of the basilar membrane.22
Moon et al. noted that patients with abnormal SP/AP exhibited significant elevation in their hearing thresholds compared with those who had SP/AP within the normal range, suggesting that MD patients with severe endolymphatic hydrops suffer more severe hearing deterioration over time23 – data corroborated by Ge et al.23
Lopes assessed the sensitivity and specificity of SP/AP ratio and the graphic angular measure in electrocochleography studies of 71 ears (41 MD patients and 14 healthy controls). This author concluded that the graphic angular measure is not sensitive and specific enough for the diagnosis of MD. The association of SP/AP and graphic angular measure resulted in improved sensitivity, at the expense of the specificity of the test.24
Devaiah et al. conducted a retrospective study of 138 patients with MD who underwent transtympanic electrocochleography in order to identify patients with possible Ménière's disease. A control group for patients with normal SP/AP ratio was created. The SP/AP ratio and the area under the curve (AUC) for both groups were measured. These authors identified an increase in sensitivity for transtympanic electrocochleography with clicks with alternating polarity, by analyzing SP/AP AUC in the diagnosis of Ménière's disease. They found that seven of eight patients with possible Ménière's disease show an increase in SP/AP AUC.14
Baba et al. conducted a retrospective study of 198 patients undergoing transtympanic electrocochleography and compared SP/AP ratio and SP/AP AUC. Regarding SP/AP ratio, they found 57.1% of sensitivity in patients with definite MD, 39.6% in patients with probable MD, and 50% in those cases that turned from probable to definite MD. With respect to SP/AP AUC, they found 43.9%, 27.7%, and 30% respectively, concluding that the analysis of SP/AP AUC with transtympanic electrocochleography does not necessarily increase the sensitivity in the diagnosis of endolymphatic hydrops compared with SP/AP amplitude.25
Ikino et al. used transtympanic electrocochleography to examine 21 patients with definite Ménière's disease and 19 normal hearing patients with other cochleovestibular disorders. They compared SP/AP, AP latency difference, and area under curve of SP/AP ratio and calculated the diagnostic sensitivity of these parameters. The mean SP/AP AUC was 1.89ms in the study group and 1.58ms in the control group. The mean SP/AP was 0.37 in the study group and 0.22 in the control group. The mean product of SP/AP AUC by SP/AP ratio was 75.26ms in the study group and 34.60ms in the control group. The mean AP latency difference was 0.13ms in the study group and 0.07ms in the control group. The differences between groups were statistically significant for all parameters evaluated. The sensitivities for SP/AP AUC, SP/AP ratio, and AP latency difference in the study group were 33.3%, 52.4%, and 23.8%, respectively. These authors concluded that the use of the parameters studied did not increase the sensitivity of electrocochleography, regardless of whether they were used alone or in conjunction with SP/AP. The calculation of SP/AP showed the highest sensitivity.26
Ikino et al. also analyzed 22 patients (16 females and eight males) with transtympanic electrocochleography, aiming to examine the latency of condensed and rarefied clicks and the differences between these latencies in patients with Ménière's disease. Those eight cases (36.4%) with SP/AP ratio ≥0.33 were defined as group 1, whereas the 14 cases (63.6%) with SP/AP ratio <0.33 were defined as group 2. In 36.4% of patients, the relationship between the summation potential and the action potential was greater than 0.33; for these patients, the latency of condensed clicks, the latency for rarefied clicks, and the differences between their latencies were 1.94ms, 1.84ms, and 0.25ms, respectively. In the other patients, these values were 1.71ms, 1.71ms, and 0.09ms. Ikino et al. concluded that the latency for condensed clicks and the difference between latencies for condensed and rarefied clicks were not significantly higher in patients with endolymphatic hydrops.27
Yamamoto et al. performed an magnetic resonance imaging (MRI) study after intratympanic gadolinium injection and observed that the SP/AP ratio obtained with extratympanic electrocochleography with the use of rarefied and condensed clicks was significantly increased in patients with endolymphatic hydrops, except in patients with early-stage disease, within three months of the onset of symptoms.28
Seo et al. also demonstrated endolymphatic hydrops in the cochlea (81%) and saccule (69%) using MRI 3T after intratympanic gadolinium in correlation with abnormal electrocochleographic thresholds. They considered as an altered SP/AP threshold for click stimuli greater than 0.33, and 1000Hz tonebursts were considered abnormal if the absolute magnitude of PS were ≤3μV.29
Studies examined the difference in specificity and sensitivity of transtympanic and extratympanic collection methods. The present review demonstrated that the transtympanic method would be more effective; however, according to Pappas, Ghosh, and Chung, the extratympanic method can also be considered as an effective, easy to perform in clinical practice, and non-invasive method.10,13,17 It was observed that electrocochleography plays a role, especially in cases of scarce audiological data and with less defined symptoms.
Regarding the variation of stimuli to obtain the results, it was observed that the click is not useful for differentiating between healthy ears and ears with Ménière's disease. In the studies by Gibson, Colon, and Claes, it was demonstrated that the toneburst increases the sensitivity of the test.9,12,19 As to the stimuli polarity, no statistically significant differences were observed in relation to differences in latency for condensate and rarefied stimuli.
It can be concluded that the SP/AP ratio was the most sensitive and specific diagnostic parameter – data corroborated by Soares, Baba, and Ikino.16,25,26 Lopes and Devaiah reported an increase in sensitivity of the test for diagnosis with the association of SP/AP ratio with the area under of the curve of SP/AP.14,24 The SP/AP thresholds are variable in the literature, with diagnosis for values greater than 0.5, according to most authors searched.
Several authors also analyzed the relationship of SP amplitude with disease duration. It was observed that ears with symptoms of longer duration show greater abnormalities in the SP/AP ratio; and that once SP rises, this situation will persist for long periods.
ConclusionElectrocochleography is an important tool in the diagnosis of endolymphatic hydrops. The literature review identified that the extratympanic method is effective, non-invasive, and easy to perform in clinical practice. New techniques can increase the sensitivity of the test, such as the use of the toneburst and the analysis of the area under the curve of SP/AP ratio, in association with SP/AP ratio measurement.
Electrocochleography still remains the only test that can objectively measure endolymphatic hydrops in the cochlea and that fulfills its role, aiding the otolaryngologist in the treatment of Ménière's disease, especially when the audiological data are scarce and the symptoms are less defined.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Lamounier P, Gobbo DA, de Souza TS, de Oliveira CA, Bahmad Jr F. Electrocochleography for Ménière's disease: is it reliable? Braz J Otorhinolaryngol. 2014;80:527–32.
Institution: Universidade de Brasília, Brasília, DF, Brazil.