To compare functional outcome of microscopic and endoscopic approach regarding type of ossiculoplasty.
MethodsIn this retrospective study, cases who had undergone type-II and type-III tympanoplasty between February 2007 to September 2019 were divided into two groups according to the type of approach as microscopic and endoscopic. In cases with type-II reconstruction; Partial Ossicular chain Replacement Prosthesis (PORP), incus interposition and bone cement were used in order of frequency. Whereas in cases with type-III reconstruction, only Total Ossicular chain Replacement Prosthesis (TORP) was used. The average Air Bone Gap (ABG) was determined pre- and post-operatively for the calculation of Air Conductance Gain (ACG). The ACG, pre- and post-operative ABG values of each group were compared with regard to the type of ossiculoplasty.
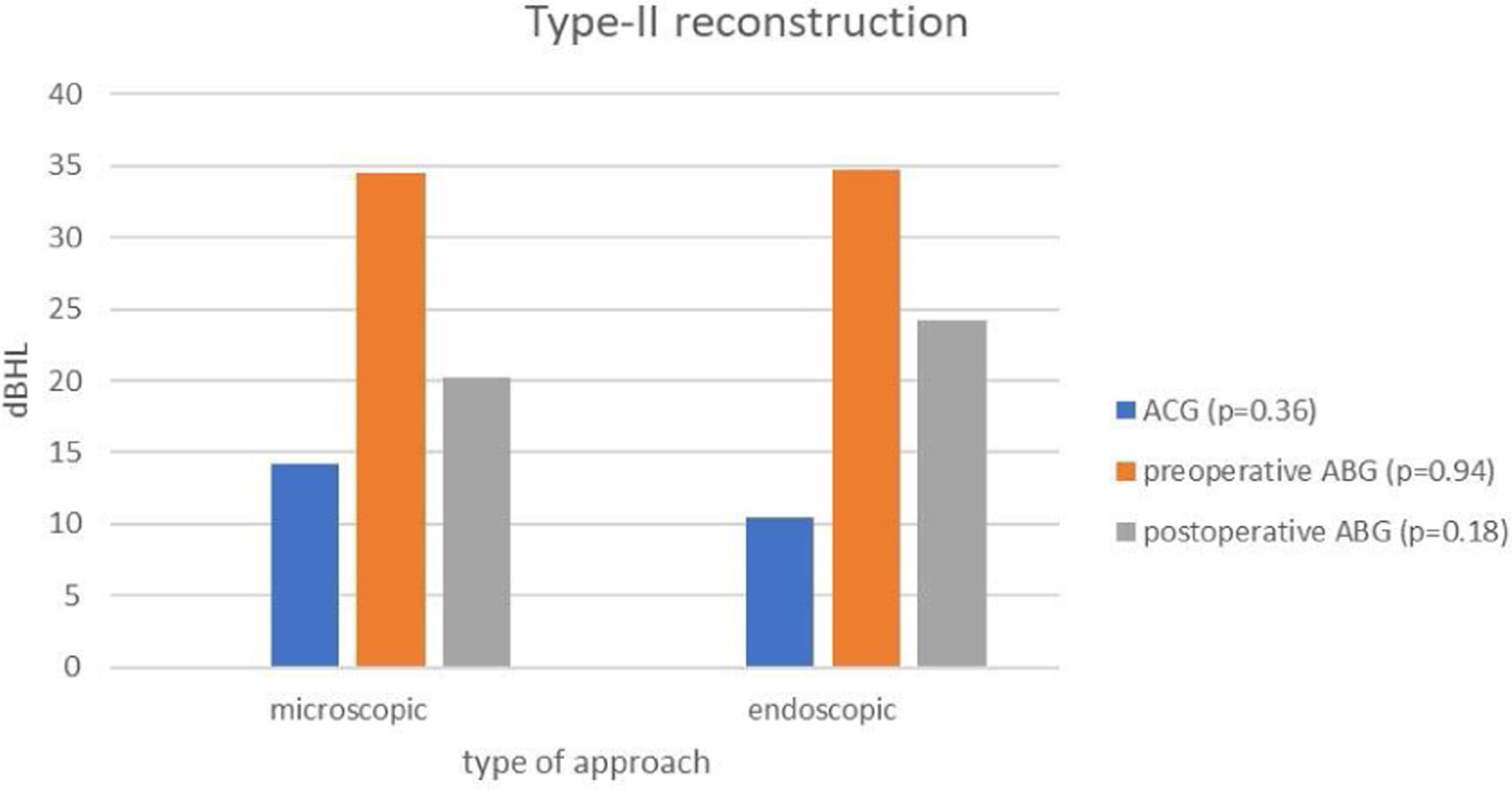
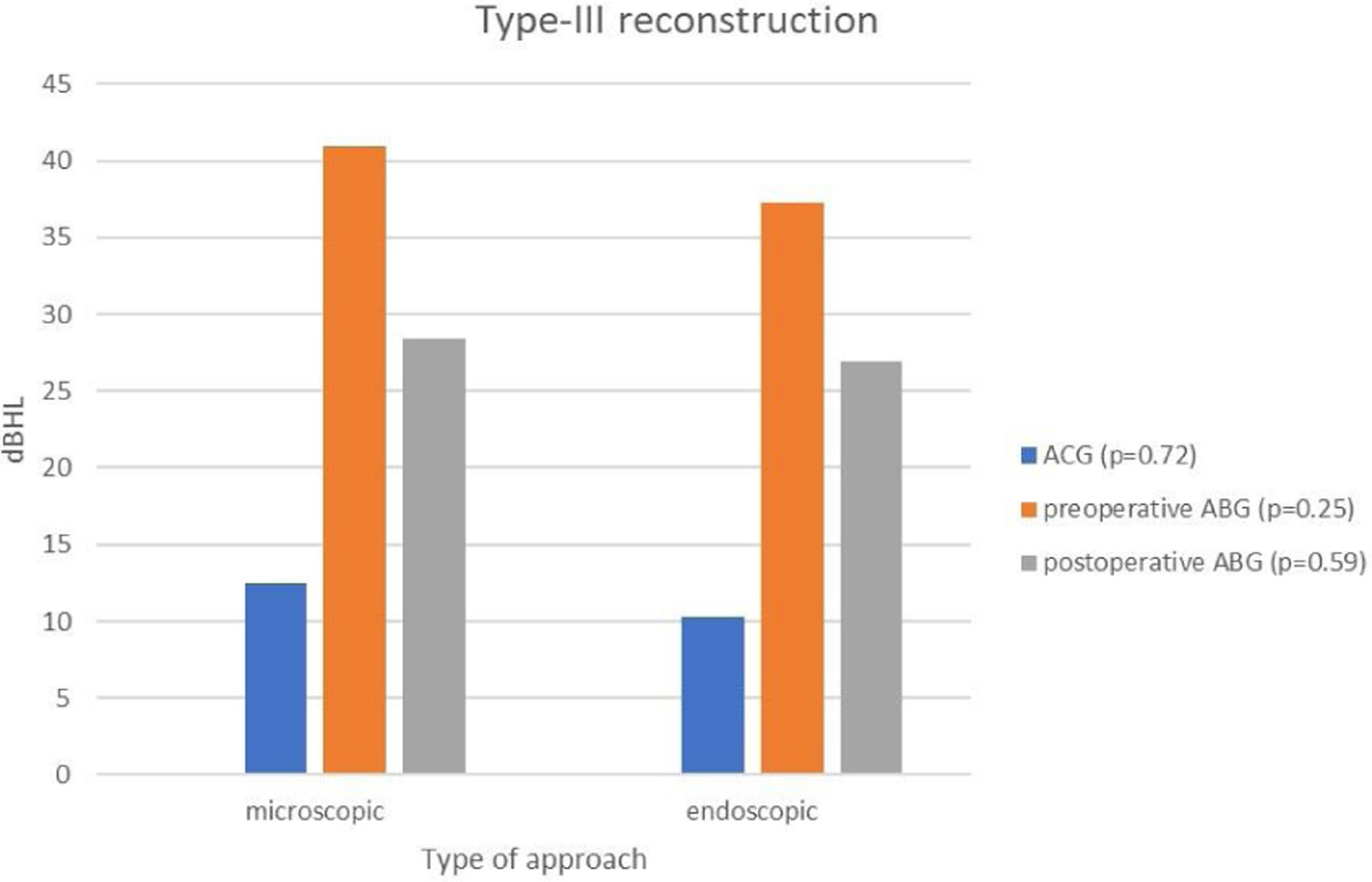
ResultsA total of 79 cases consisting of 32 females and 47 males who had undergone type-II and type-III tympanoplasty were enrolled. No statistically significant difference between microscopic and endoscopic approach was found in terms of ACG (p = 0.42), pre-(p = 0.23) and postoperative ABG (p = 0.99). We did not find any significant difference in terms of ACG, pre- and postoperative ABG between two approaches for type-II and type-III reconstructions (p > 0.05).
ConclusionsAccording to the current study, endoscopic approach in type-II and type-III reconstruction is at least reliable as microscopic approach regarding functional outcome. Since both techniques have similar functional results, other factors (anatomic characteristics, habitude of the surgeon and duration of the surgery) should be considered when choosing the technique.
Level of evidenceIn the current paper we present a retrospective comparative study of two different approaches of a particular type of otologic surgery. Level of evidence corresponds to level III.
The classical approach to middle ear surgery is microscopic technique.1,2 Operating microscopes have been used dated from mid-20thcentury.3,4 At the beginning, microscopes were utilized in limited number of middle ear surgery like tympanoplasty and ossiculoplasty.1–3 Over time, with the reciprocal evolvement of microscopes and surgical techniques, the use of microscopes in every type of otologic surgery becomes indispensable. On the other side utilization of endoscopes as the main approach for middle ear surgery is relatively novice.5–7 At the beginning, the endoscopes had been used only for diagnostic purposes or assistance in microscopic middle ear surgery.8,9 But nowadays even the whole surgical process could be carried out solely by endoscopic approach. Endoscopes have been used in various types of ear surgeries also including the ossiculoplasty. With the ever-increasingly use of endoscopes in almost every type of otologic surgery, as a matter of cause some questions emerged concerning the feasibility and reliability of endoscopes.
Many classifications have been proposed for tympanoplasty and ossiculoplasty. Wullstein published the 1st classification of tympanoplasty including details of middle ear surgery and ossiculoplasty in 1956.10 Next, the original classification was modified on several occasions by Lierle,11 Farrior,12 Belluci,13 Pratt,14 Nadol and McKenna,15 respectively. On the other hand, McGee and Hough16 have defined a novel classification focusing mainly on ossiculoplasty which was then generally accepted. The classification of McGee and Hough also was preferred in this study.
There is an ongoing dispute concerning the need and feasibility of endoscopic approach in ear surgery. But two obstacles seem to leap out in comparing the microscopic and endoscopic approach. At first, there are numerous types of different surgical techniques of ossiculoplasty complicating the comparison of two approaches. The latter one is the existence of different ossiculoplasty classifications which also hampers the comparison of both approaches throughout different studies.
There are limited number of studies comparing the both approaches particularly in terms of ossiculoplasty.17–19 In this study, we aimed to reveal the effect of the surgical approach (microscopic and endoscopic) on the functional results of ossiculoplasty while considering two subtypes.
MethodsDesign and study populationThis retrospective study was approved by the institutional ethical committee (protocol number: 21/05/2021/20478486-800). Required sample size was determined by a power of 95% based on an effect size of α2 = 0.05. (G*power 3.1.9.7). Total sample size was predetermined as 45 for paired samples t-test and 47 for Wilcoxon signed-rank test. Total sample size of the current study was actualized as 79 cases which was within the limit.
The medical documents of all cases who had undergone type-II and type-III tympanoplasty between February 2007 to September 2019 were analyzed. The exclusion criteria were as follows: (i) Presence of retraction pocket, (ii) Presence of cholesteatoma (iv) History of previous surgery in the relevant ear, (v) Utilization of both microscopy and endoscopy. According to these criteria, 79 eligible cases were enrolled into the study, which were then divided into two groups according to the type of approach as: (i) Microscopic (36 cases) and (ii) Endoscopic (43 cases).
Endoscopic otological surgery was started in our clinic in 2015. The microscopic group mainly includes the cases operated between 2007–2015 while the endoscopic group includes cases after 2015. There were not any clinical selection criteria for the type of approach. Therefore, homogeneity of potential confounding variables like preoperatif audiological data, site and size of tympanic membrane perforation were also compared on group basis. Besides, cases with postoperative graft failure were not enrolled into the study to forestall the potential confounding effect of tympanic membrane perforation on functional outcome of ossiculoplasty.
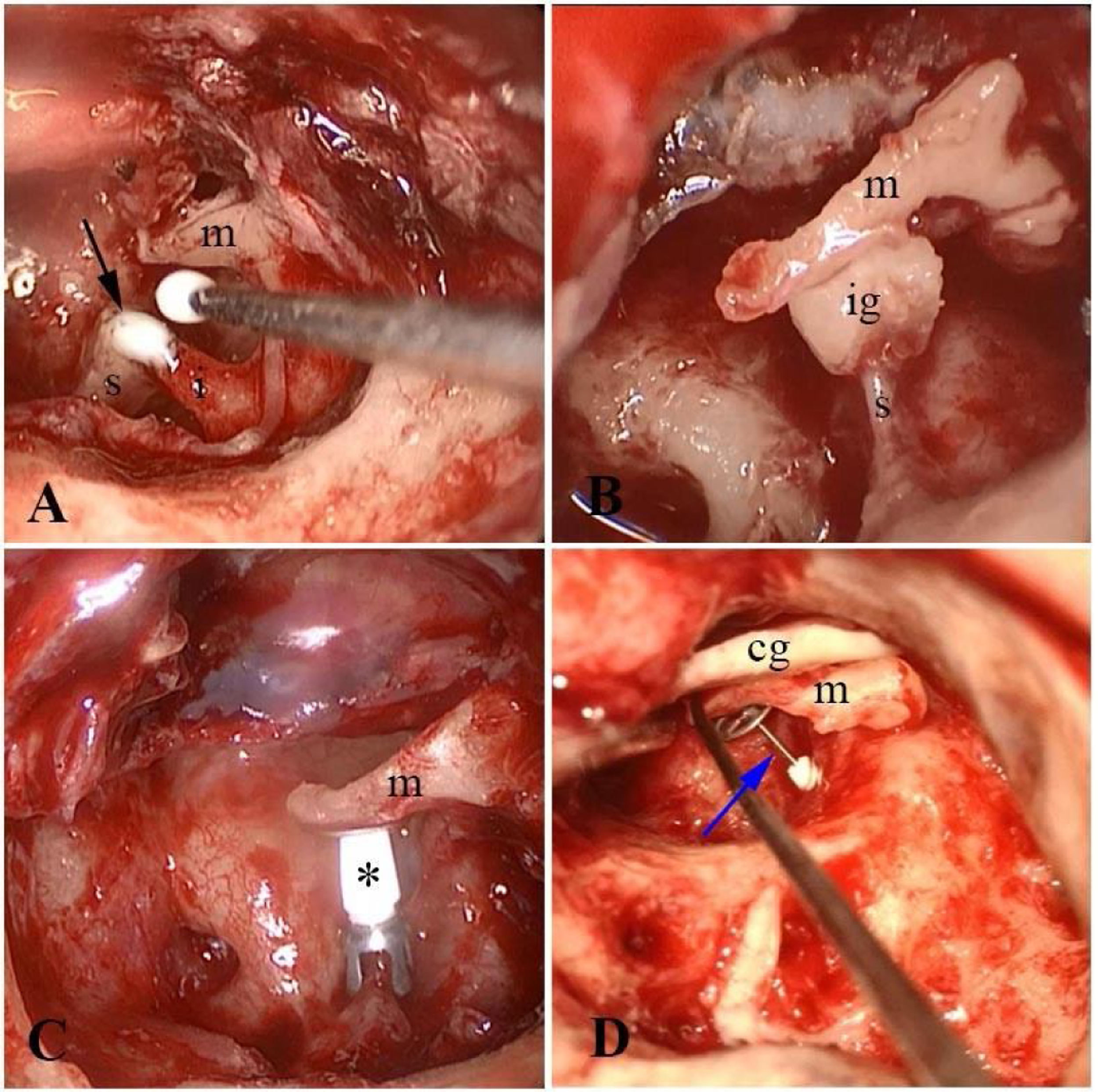
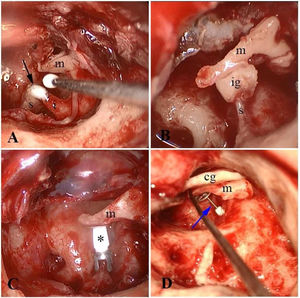
Surgical procedureType-II and type-III tympanoplasty was performed by the same attending surgeon, individually and with assistance from otolaryngology residents. Patients in both groups were operated on under general anesthesia. We used the endoscopic ear classification system designed by Gulsen and Baltacı.20 According to this, all endoscopic approaches of the current study were class IV which means that the whole surgery was carried out solely by endoscopes through the ear canal. On the other hand, transcanal, postauricular and endaural approaches were used for the microscopic group according to the pre-operative microscopic ear examination, in which the pattern of the ear canal, and the site and size of perforation were taken into account. The type of graft was determined according to the type of ossiculoplasty along with the condition of the relevant and the opposite ear. In cases with type-II reconstruction; Partial Ossicular chain Replacement Prosthesis (PORP), incus interposition and bone cement were used in order of frequency. Whereas in cases with type-III reconstruction, only Total Ossicular chain Replacement Prosthesis (TORP) was used (Fig. 1).
Endoscopic view of bone cement utilization (A), incus interposition (B) and PORP placement (C) in type-II reconstruction. Endoscopic view of TORP placement is seen in (D). Black arrow, bone cement; s, stapes; I, Incus; m, malleus; ig, incus-graft; * PORP; cg, cartilage graft; blue arrow, TORP.
Cases with disconnection between long process of incus and head of the stapes were categorized as type-II while cases with missing head and crural arch of the stapes were categorized as type-III.
Before the surgery, diluted epinephrine (5 µg/mL [5‒8cc]) in one-to-one ratio was injected into canal skin in four quadrants and the retro-auricular region in the case of the retro-auricular approach. The graft was harvested from the tragus. For harvesting the cartilage graft, the skin incision was made on the medial side of the tragus, with a 2–3 mm rim of cartilage left on the lateral margin of the tragus for cosmetic purposes.
Medial circumferential and radial canal incisions were made for the elevation of the tympan meatal flap in both approaches. After elevation of the annulus, the continuity and mobility of the ossicular chain were checked in all cases. In both groups, the grafts for tympanic membrane reconstruction were placed in an over-underlay fashion. Gelfoam pieces in different sizes and numbers were placed into the middle ear and over the graft. The operation was ended with the placement of polyvinyl alcohol sponge (Merocel) in the ear canal.
Duration of surgery was obtained for each case from past surgery reports and compared on group basis.
Documentation of outcome measuresFor the evaluation of the functional outcome, pure tone audiometry (air and bone conduction thresholds at frequencies of 250 Hz, 500 Hz, 1000 Hz, 3000 Hz and 4000 Hz) were reviewed pre- (just before admission) and post-operatively (1 year after surgery). The average Air Bone Gap (ABG) was determined pre- and post-operatively for the calculation of Air Conductance Gain (ACG) for each case.
Documentation of tympanic membrane perforationTympanic membrane perforations were classified in 2 ways according to size and localization as previously reported.21 In terms of size, we categorized them according to involved percentage as small (<25%) moderate (25%–75%) and large (>75%). On the other hand, we categorized them as anterior, posterior, central, and marginal, in terms of localization.
Statistical analysisThe functional outcome was evaluated by comparing the ACG and the post-operative ABG. The distribution was evaluated by the Shapiro–Wilk test. Variables with normal distribution were presented as mean (Standard Deviation [SD]), while non-normal variables were reported as median (Interquartile Range [IQR]). The ACG, pre- and post-operative ABG values of each group were compared by paired samples t-test or Wilcoxon signed-rank test according to the results of Shapiro-Wilk test. Size and site of perforation were compared by independent samples t-test between groups. A Confidence Interval of 95% and p < 0.05 were considered to be statistically significant (IBM SPSS Statistics for Windows, Version 21.0; Armonk, NY, IBM Corp.).
ResultsDescriptive statisticsIn this study, a total of 79 cases consisting of 32 females (mean age ± SD: 40.25 ± 3.08) and 47 males (mean age ± SD: 30.26 ± 2.22) who had undergone type-II and type-III tympanoplasty were enrolled. The study population was then classified into two groups as microscopic and endoscopic. No significant difference was found between both groups in terms of age (p = 0.94). The distribution of cases according to approach and type of ossiculoplasty is presented in Table 1. Duration of operation for microscopic and endoscopic group was 107.75 ± 23.81 (mean ± SD) and 67.51 ± 14.70 (mean ± SD), respectively.
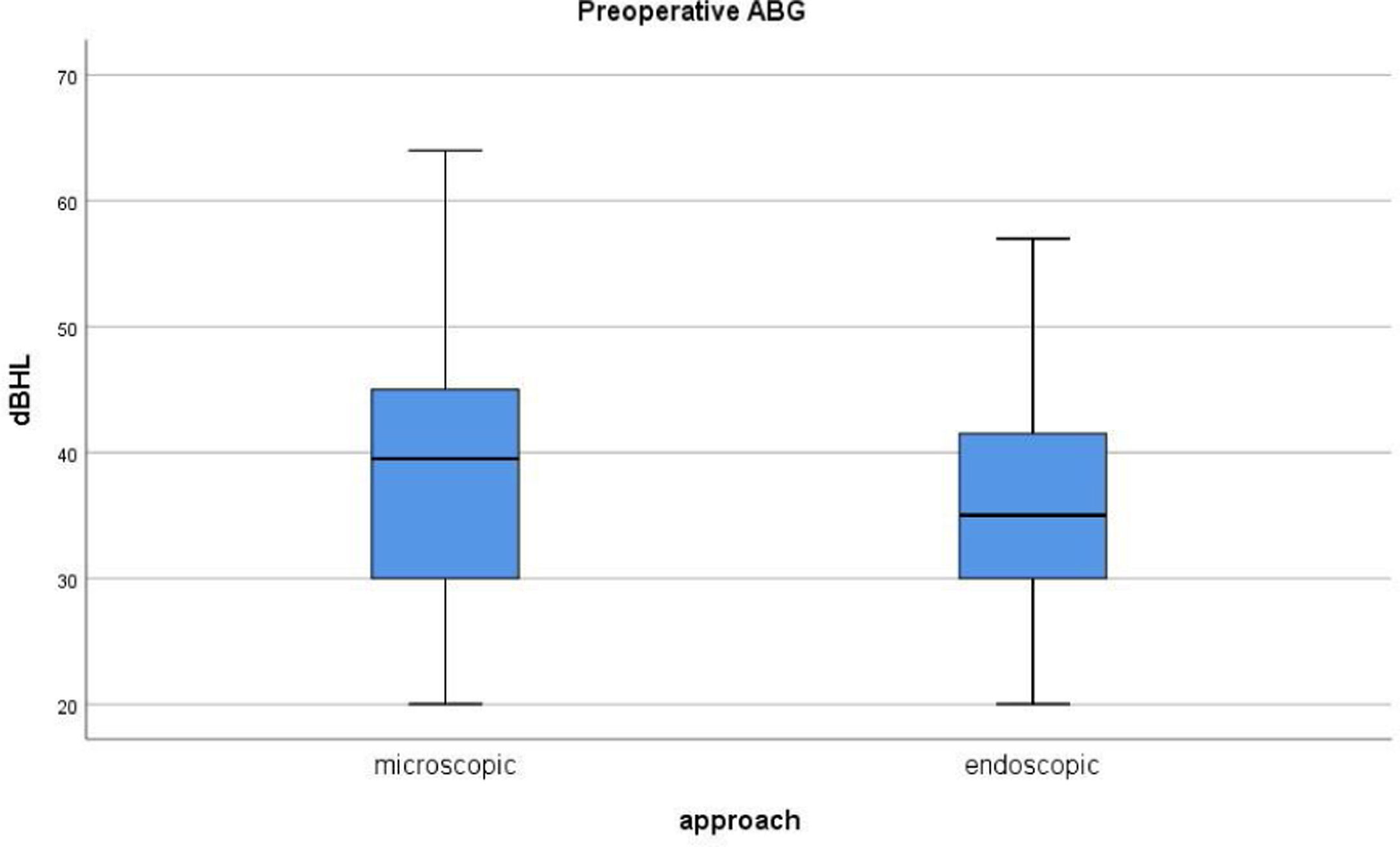
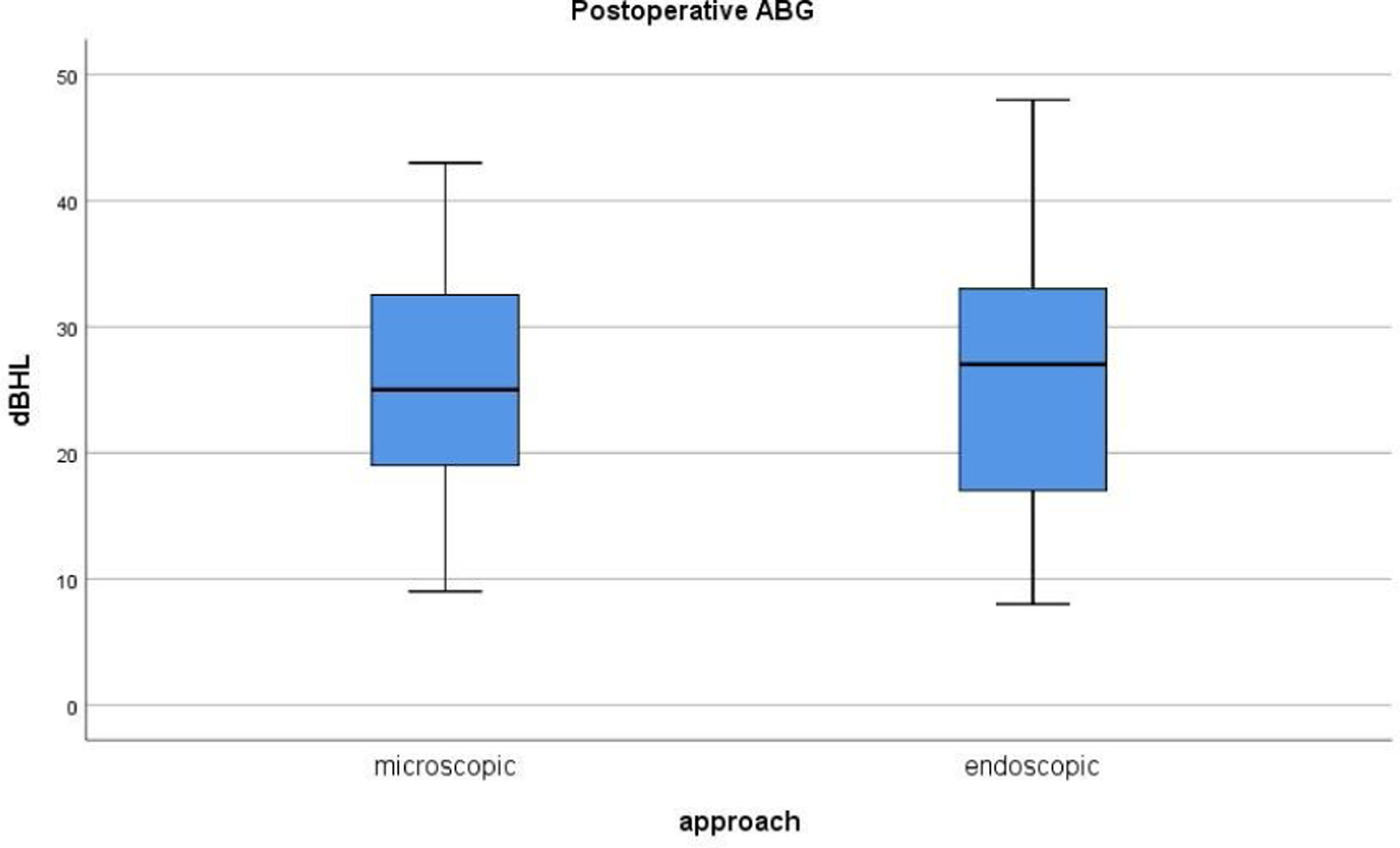
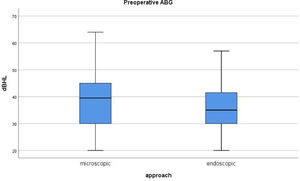
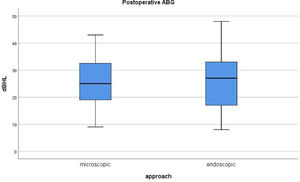
The Shapiro–Wilk test and a visual inspection of histograms, normal QQ plots and box plots (Fig. 2) showed that the pre-operative ABG values were normally distributed for the microscopic (p = 0.64) and endoscopic group (p = 0.69). Post-operative ABG values were also found to be normally distributed for the microscopic (p = 0.97) and endoscopic group (p = 0.96) groups (Fig. 3). Thus, comparison of preoperative and postoperative ABG values between groups was performed using the “Wilcoxon signed-rank test”.
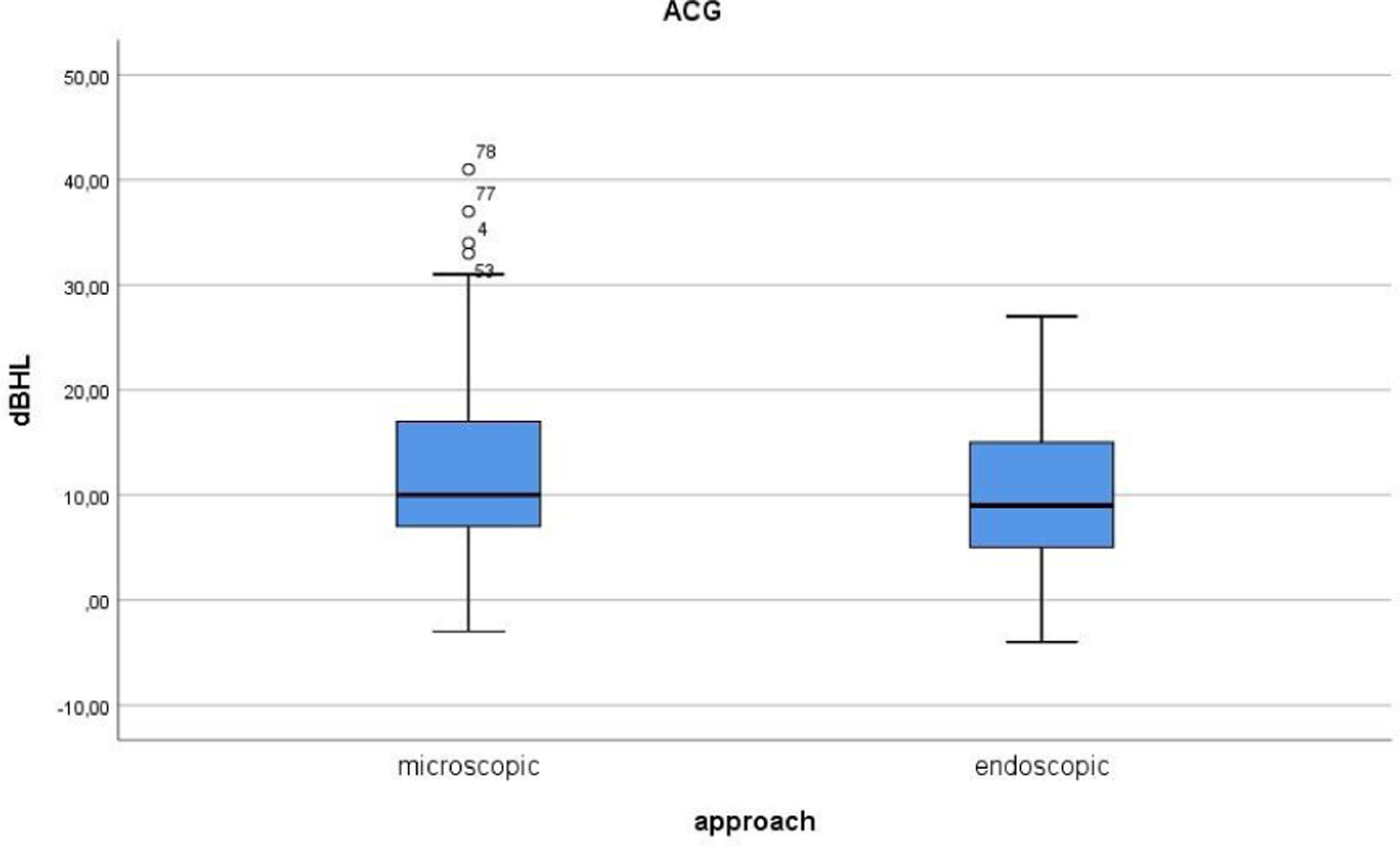
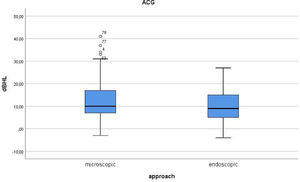
The Shapiro–Wilk test and a visual inspection of histograms, normal QQ plots and box plots (Fig. 4) showed that the ACG values for the microscopic (p = 0.001) were found to be not normally distributed while the endoscopic group (p = 0.47) was found to be normally distributed. Thus, comparison of ACG on group basis was done by independent samples-t test.
Functional outcome measuresThe mean ACG along with preoperative and postoperative ABG concerning approach is summarized in Table 2. Comparison of ACG, pre- and postoperative ABG between groups revealed statistically insignificant difference (Table 2).
Comparison of functional parameters regarding surgical approach.
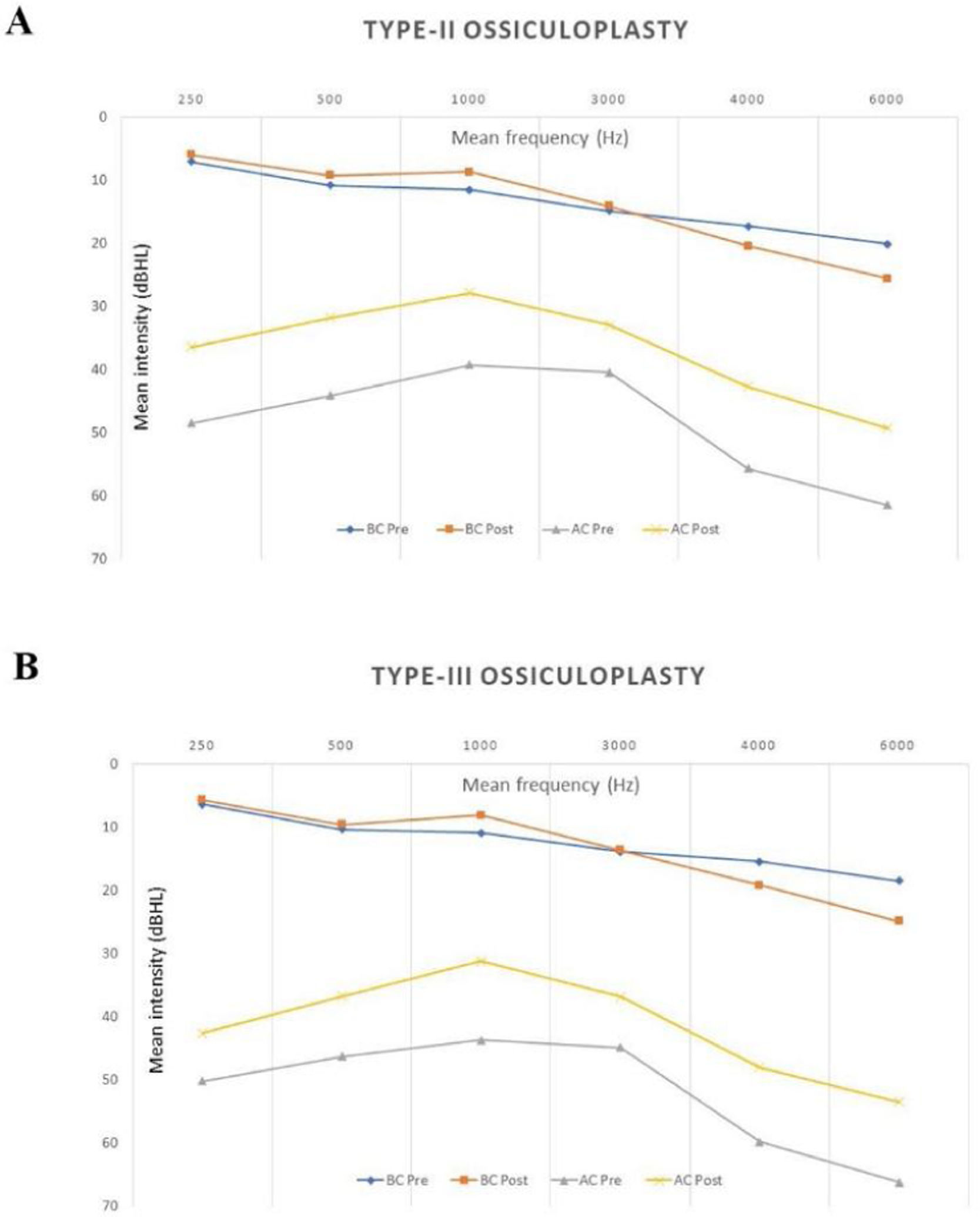
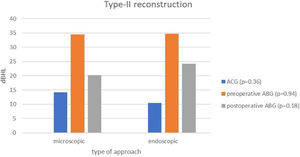
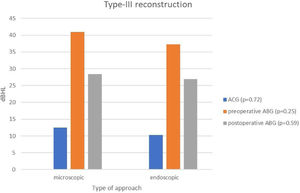
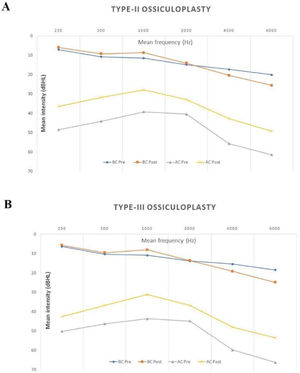
We also compared both approaches in terms of type-II and type-III reconstructions separately. We did not find any statically significant difference in terms of ACG, pre- and postoperative ABG between two approaches for type-II (Fig. 5) and type-III (Fig. 6) reconstructions. In addition, mean audiometric results of type-II and type-III ossiculoplasty including pre- and postoperative frequency-based hearing intensity is provided in Fig. 7.
Evaluation of preoperative status of tympanic membrane on groups basisComparison of site and size of perforation between both approaches does not reveal statistically significant difference (Table 3).
Comparison of status of tympanic membrane on groups basis regarding size and site of perforation.
| Status of tympanic membrane | Microscopic (n, %) | Endoscopic (n, %) | p-value |
|---|---|---|---|
| Size of perforation | |||
| Small (<25%) | 7 (19.4) | 5 (11.6) | p = 0.35 |
| Moderate (25%–75%) | 16 (44.4) | 25 (58.2) | p = 0.23 |
| Large (>75%) | 13 (36.2) | 13 (30.2) | p = 0.58 |
| Site of perforation | |||
| Anterior | 12 (33.3) | 10 (23.3 | p = 0.33 |
| Posterior | 13 (36.1) | 15 (34.8) | p = 0.91 |
| Central | 7 (19.5) | 16 (37.2) | p = 0.08 |
| Marginal | 4 (11.1) | 2 (4.7) | p = 0.30 |
Comparison of operative duration revealed statistically significant difference in favor of endoscopic approach (p < 0.001).
DiscussionIn the current study, we did not find any statistically significant difference in terms of ACG, pre- and postoperative ABG between two approaches. The pre- and postoperative ABGs were found to be similar between the two groups for both ossiculoplasty types. This homogeneity of ABGs throughout groups increases the reliability of our results. It should also be noted here that the main indicator of functional success is ACG, which was found to be similar in both approaches, regardless of the ossiculoplasty type (Fig. 5, Fig. 6). Comparison of tympanic membrane perforation with regard to size and localization did not reveal any significant statistical difference (Table 3). This finding can be accepted as a factor against possible group selection bias. Considering these findings, it can be asserted that endoscopic type-II and type-III ossiculoplasty is just as effective as the microscopic approach. In other words, type of ossiculoplasty has no effect on the functional outcome of either approach.
There are numerous clinical studies evaluating microscopic and endoscopic approach in terms of outcomes. Considering the design of these studies, basically two different research designs stand out. Namely, in most of the studies5,6,9,22–27 outcomes of only one approach (microscopic or endoscopic) were evaluated solely, while in remaining fewer studies both approaches are compared in a controlled clinical research design.28–30 On the other hand, number of studies which particularly evaluate the functional outcome of “endoscopic ossiculoplasty” is very limited.17–19 As far as we know, the only randomized control trial focusing on endoscopic ossiculoplasty was done by Das et al.18 They compared functional outcome of TORP and PORP in terms of approach (microscopic and endoscopic). Conspicuously, they revealed a significant better ACG in endoscopic group when compared with the microscopic group particularly in the PORP series. But the long term ACG in both approaches for both (TORP and PORP) prosthesis did not differ significantly. The results of the current study are concordant with the study of Das et al. But our study differs in some respects. We constituted the subgroups according to the type of ossiculoplasty as type-II and type-III rather than the type of prosthesis. Thereby, unlike the study of Das et al., other reconstruction methods like incus interposition and bone cement utilization have also been included in the subgroups. Besides, in the study of Das et al., cases with additional pathologies had not been excluded.18 In contrast with the current study, they had included cases with cholesteatoma and retraction pockets which might affect functional outcome in favor of one approach. It is apparent that every additional manipulation or drilling for retraction pocket and/or cholesteatoma would have impact on the eventual status of the ossicular chain. Another study done by Calowey et al.19 was designed comparable to our study in terms of subgroups. Namely, they also included incus interposition and bone cement utilization. Besides, their study was also retrospective just like the current one. But there was a main difference that their study was on pediatric cases below the age of 18. Nevertheless, they also failed to reveal any significant difference between both approaches and both ossiculoplasty techniques in terms of ACG. Besides, Yawn et al.17 also found no significant difference in ACG between both approaches. But they included cases with mastoidectomy, cholesteatoma and recurrent surgery which are defined as exclusion criteria in the current study. They had preferred microscopic approach when middle ear pathology (cholesteatoma, etc.) extend beyond the horizontal semicircular canal. It is apparent that these factors would lead selection bias in favor of endoscopic approach.
To the best of our knowledge, the only meta-analysis on studies comparing endoscopic and microscopic ossiculoplasty was done by Tsetsos et al.31 After a comprehensive search and analyses of three hundred twenty eighth studies they ended up only with 3 eligible studies which are also reviewed above.17–19 Tsetsos et al. concluded that endoscopic approach is at least as feasible as microscopic approach. Our study differs from the previous ones in such a way that we paid regard to the peroperative status of the ossicular chain rather than the type of graft or prosthesis for subgroup classification. In other words, we constituted the subgroups according to the type of ossiculoplasty as type-II and type-III rather than the type of prosthesis.
In both endoscopic and microscopic ossiculoplasty, the reconstruction methods are the same; namely the type of graft and prosthesis, incisions, flap elevations, placement of the reconstruction material etc. does not differ. Thus, one might not expect a significant difference in overall outcome. On the other hand, ossiculoplasty necessitates very delicate manipulation of ossicles. For this reason, some other factors which differ between two approaches might affect particularly the functional outcome. Hence, if there is any difference in functional outcome, it can be linked up to other factors such as depth of field, number of hands in use and heat exposure which are evaluated previously in numerous studies.32 There are some advantages of endoscopic approach particularly in ossiculoplasty. It provides better and closer visualization of the ossicles, oval window and surrounding microanatomical landmarks.33 On the other side, the microscopic approach comes to the fore with the absence of thermal injury and the ability to use both hands.34 It seems that all these factors counter acts and ultimately countervails the functional outcome for both approaches.
Our study has certain limitations. First, it was not possible to totally avoid selection bias due to the retrospective design. To partially forestall this bias, we compare both groups in terms of other clinical factors like preoperative ABG and status of the tympanic membrane. We also excluded cases with additional pathologies (presence of cholesteatoma and retraction pocket) apart from ossicular chain pathologies which might hamper the functional outcome in favor of one approach. In addition, cases with postoperative graft failure were excluded for the detection of exact functional success achieved solely by ossiculoplasty. The second limitation was the lack of early (< 6 months) and late term (>1 year) audiometric results. Audiometric data at one year could be obtained completely which reflects the mid-term functional status sufficiently.
There are limited number of studies regarding impact of approach on functional outcome of different ossiculoplasty types which all have their distinctive limitations.17–19 Similarly, we investigated the impact of approach on functional outcome in terms of ossiculoplasty type. But our study dissociates from the previously mentioned three studies in that we payed regard to the peroperative status of the ossicular chain rather than the type of graft or prosthesis.
In the last instance, it would be appropriate to take into account anatomic characteristics, habitude of the surgeon and duration of the surgery rather than the functional outcome when deciding the type of approach.
ConclusionThe current study revealed that endoscopic approach both in type-II and type-III ossiculoplasty is at least reliable as microscopic approach regarding ACG and postoperative ABG.
Data availabilityData will be made available on request.
Ethical approvalThis retrospective research was approved by the Health Sciences Ethics Committee of Manisa Celal Bayar University (21/05/2021/20478486-800) and records Hafza Sultan Hospital was utilized.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.