Langerhans cell histiocytosis (LCH) is characterized by clonal proliferation of Langerhans cells exhibiting Birbeck granules and positive immunohistochemistry for S100 and CD1A.1 A malignant transformation or a functional proliferation of Langerhans cells responding to external stimuli are possible sources.2 In the oral cavity, they can occasionally present as hyperplasia of the gingiva or ulcers of the cheek, palate, or tongue mucosa.3 The diagnosis is made after careful examination, and the exclusion of other similar diagnostic possibilities.
Several therapeutic modalities have been suggested for LCH, such as intralesional corticosteroid injection, antibiotics, steroids, radiation therapy, and chemotherapy. Surgical options ranging from extensive resections to more conservative approaches are available and, in many cases, healing has resulted from a single biopsy.4
The present report regards LCH in the oral cavity and emphasizes the rarity of this lesion, as well as the importance of differential diagnosis, treatment, and appropriate follow-up for these patients.
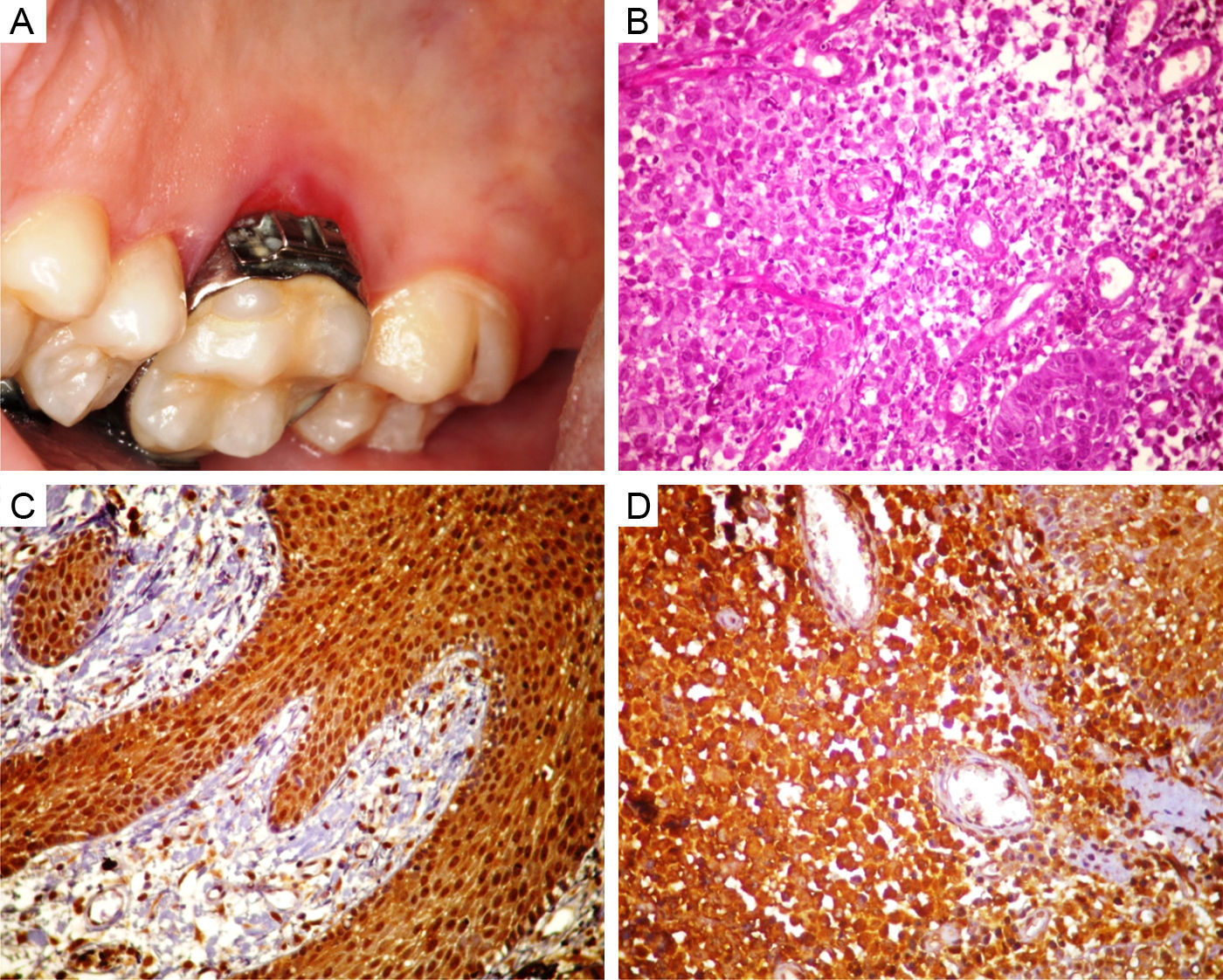
Case presentationA ten-year-old male with leukoderma presented to the Stomatology Clinic, with a three-month history of a lesion on the roof of the mouth. On intraoral examination, a red ulcerated lesion of approximately 1cm size with an orthodontic ring (Fig. 1A) was seen on the palatal gingiva adjacent to the first upper molar. Following periodontal treatment, no improvement was observed, and an initial diagnosis of paracoccidioidomycosis was suggested. Incisional biopsy revealed a lesion predominantly consisting of polygonal cells, at times exhibiting granular cytoplasm (Fig. 1B), consistent with LCH and confirmed by strongly positive immunohistochemistry for S100 (Fig. 1C) and CD1A (Fig. 1D). The condition was treated by chemotherapy and surgical removal of the lesion. Over the next ten years, the patient was assessed twice a year, and showed no clinical signs of relapse. On his last visit, he underwent a bone scan and temporal bone computed tomography and there was no evidence of relapse or metastases.
(A) Intraoral clinical imaging showing red ulcerated lesion in the palatal gingiva, adjacent to the first upper molar. (B) Microphotograph showing neoplastic lesion characterized by polygonal cells, at times exhibiting granular cytoplasm among numerous blood vessels, and inflammatory infiltrate consisting of lymphocytes, neutrophils, and eosinophils (HE ×400). (C) Immunohistochemical findings positive for S100 (×200). (D) Immunohistochemical findings positive for CD1A (×400).
The etiopathogenesis of LCH has not been fully determined, and a possible reaction or neoplastic phenomena has been proposed. A few authors further suggest an immune system regulation disorder and a familial predisposition,5 since it frequently affects children, as in the present report.
The clinical features of LCH are similar to several conditions, including periodontal disease, malignancies such as squamous cell carcinoma or lymphoma, as well as granulomatous or ulcerative lesions that are characteristic of fungal infections.2 Thus, a thorough assessment is appropriate for oral cavity lesions that persist after treatment. In the oral cavity, it usually presents as a mucosal ulcer associated with underlying bone lesions,6 which was not observed in this case.
Diagnosis may be confirmed by detecting the characteristic Birbeck granules (X bodies) or specific monoclonal antibodies to surface antigens (CD1).6 In the present case, diagnosis was confirmed after an immunohistochemical study that characterized the proliferating cell type.
The therapeutic approach depends on the extent of the disease and local treatment is usually effective in forms limited to a single organ. However, a few complications, such as pituitary gland malfunction, and especially diabetes and neurodegenerative diseases can occur.5 A retrospective review of patients with LCH revealed a high ten-year survival rate (93%); most individuals are low-risk and have no bone marrow, spleen, liver, or lung involvement.1 Our patient has had no relapse or metastasis after a ten-year follow-up; however, long-term follow-up is required to detect and control possible late-onset sequelae.3
Final commentsThe present report discussed clinical and laboratory information on LCH, emphasizing the importance of differential diagnosis, appropriate treatment, and long-term follow-up with complication and/or relapse prevention.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Lima EN, de Araújo EM, de Oliveira PT, de Medeiros AM. Oral Langerhans cell histiocytosis: case report with follow-up of ten years. Braz J Otorhinolaryngol. 2014;80:366–7.