Inadequate drooling can cause serious clinical, functional and social problems. Validated questionnaires to evaluate drooling impact on quality of life are lacking in Brazilian Portuguese.
ObjectivesTo translate and validate the drooling impact scale to Brazilian Portuguese.
MethodsThe drooling impact scale was translated to Brazilian Portuguese and back- translated to English to assess potential conceptual differences. Brazilian Portuguese version of drooling impact scale was applied to a 40 patients’ sample of sialorrhea presenting pediatric patients (up to 20 years of age). Chronbach’s alpha, exploratory factorial analysis and confirmatory factorial analysis were then proceeded with data collected.
ResultsThe mean drooling impact scale value for the whole population was 51.77 (SD = 16.13). The internal consistency obtained with Cronbach’s alpha indicated a value of 0.72 for the entire sample. The Bartlett’s test of sphericity was significant (p < 0.0001), confirming correlation among variables tested. Kaiser-Meyer-Olkin measure of sampling adequacy revealed a value of 0.72, indicating that the correlation matrix was reasonably suitable for factor analysis. Regarding exploratory factorial analysis, parallel analysis suggested a two-factor solution that was used for confirmatory factorial analysis. The first factor was responsible for 33.78% of the variance with an Eigenvalue of 3.38. The second factor explained 16.1% of the variance with an Eigenvalue of 1.61. At confirmatory factorial analysis, the two-factor model showed consistently better adjustments parameters than the one-factor model.
ConclusionThe drooling impact scale has been successfully translated to Brazilian Portuguese language, showing adequate internal validity. Validation of this instrument allows physicians and other personnel involved in the care of these patients to perform a better management of patients experiencing drooling. With this tool, we are now able to guide routines and provide guidelines both before and after the different kinds of treatments in order to improve the general well-being of the patient and his family.
Sialorrhea or drooling is considered normal in children up to 2 years of age,1 and generally improves after 18 months of age as sensorial function and oral-motor maturity develops. Drooling may cause serious clinical, functional and social problems, such as aspiration, asphyxia, feeding problems, skin tears, isolation, stigmatization and rejection.2
Quality of life (QOL) is usually described as a multidimensional item attempting to point out the characteristics of human experience from the perspective of the individual himself regarding his subjective perception, considering physical, psychological, social, economic and also emotional aspects and with the sensation of well-being as central factor.3,4 Validated questionnaires are one of the means to quantify QOL and to check the potential impact of an injury or illness on it. These questionnaires can be universal or specific to any affliction. The Drooling Impact Scale (DIS) evaluates the impact of sialorrhea on the QOL of the caregiver and of the child.
Since the reality of our country is different than that of developed countries regarding both economic aspects and the access to health services, it is necessary to study how and in what ways sialorrhea is affecting the lives of family members and patients.
However, no specific instrument for this target population was found in Brazilian Portuguese, making such an assessment impossible. As such, this study carried out the translation of the DIS into Brazilian Portuguese as well as its validation for our population.
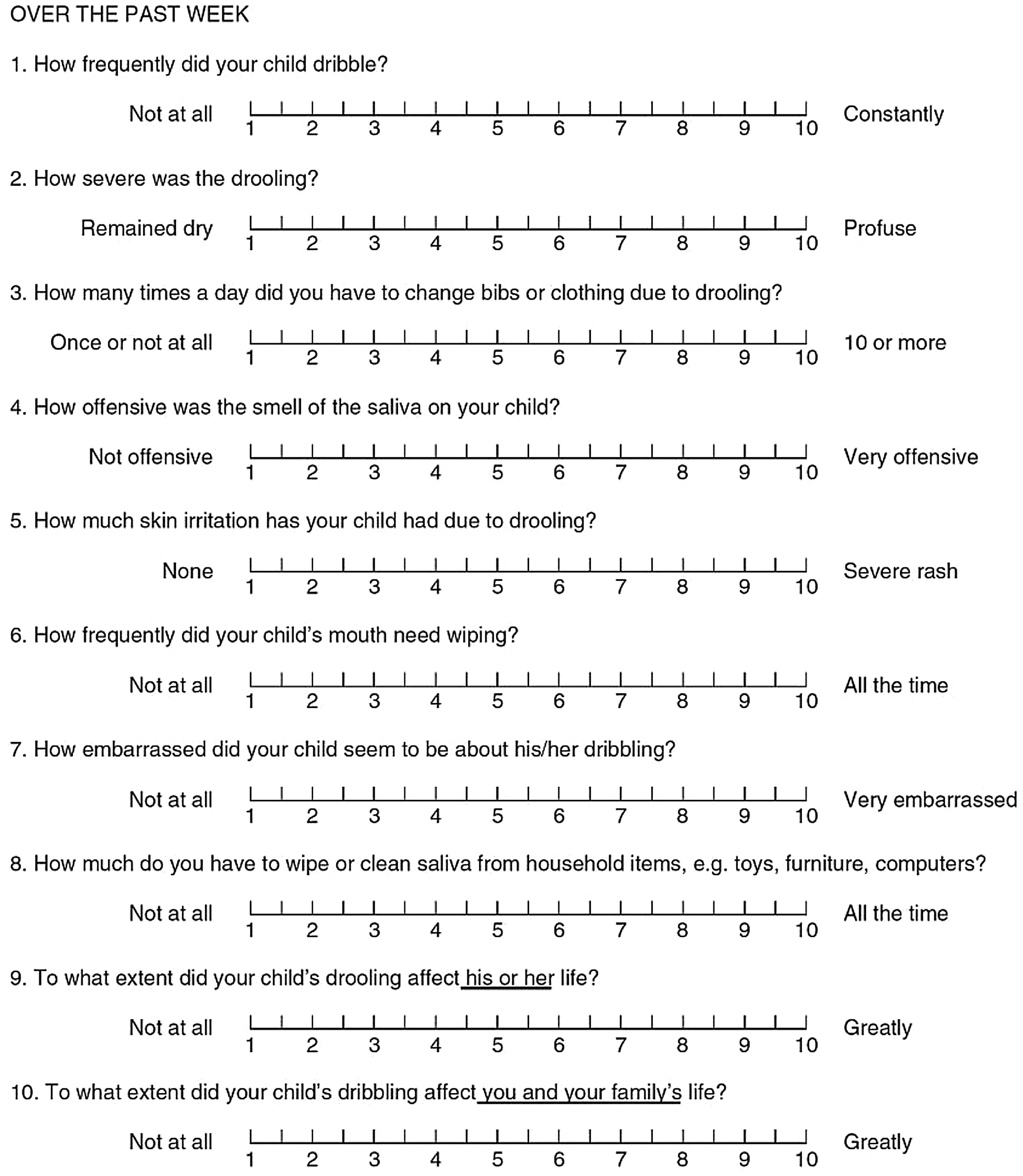
MethodsThe Drooling Impact Scale (DIS)This is a cross-sectional study. The DIS is an instrument developed by Reid et al.,5 and it is specific for the parents and caregivers of children who present sialorrhea (Fig. 1). It consists of 10 questions, and each question presents a 1 to 10 point-scale, in which higher scores reflect a greater impact of the drooling on the QOL. The questions seek to assess the parents' perception of the severity of the sialorrhea, in addition to including the social aspect, the child's well-being, and the impact on the caregiver.
Translation authorizationThe authorization for the Portuguese version of the DIS was obtained from one of the original developers (Reid, S.) and followed the standardized protocol for translations from Beaton et al. in 2000.6
The English version was translated into Brazilian Portuguese by two independent bilingual translators with Portuguese as their native language. One of them was aware of the concepts that were being examined in the instrument, and the other one had no knowledge of the issue. The consensus between these two versions was reached by those same translators. The translation back into English was then performed by two native English speakers who were totally blinded to the original version of the instrument, in order to check the validity and reliability of Portuguese version.
A consensus by a committee of experts was reached for the preliminary final version of the questionnaire, taking into account all translations and back-translations. The differences in semantic, linguistic, cultural and conceptual equivalence were corrected through consensus of this committee.
The only term in the questionnaire considered to have different regional translations was “bibs”, which in some Brazilian regions would be translated to “babeiros” instead of the term “babadores”. However, the latter term is broadly understood, even in regions where “babeiros” is more frequently used in spoken language, therefore eventually “babadores” was included in the questionnaire.
During the preliminary test of the final version, respondents were asked to answer the questionnaire and, after each inquiry, describe what they understood about the question. Questions not adequately understood or not adequately answered by the participants were then replaced by another one, concerning the same concept by the expert committee. Only after finishing all these validations was the final version considered to have an equivalent meaning to the original version. Nonetheless, during this process, no question was verified to have its comprehension compromised. The results of the preliminary test of the final version were all evaluated by the expert committee, which verified if all previous steps were properly followed.
Ethical aspectsFree and informed consent form was obtained from all participants. An approval of the Ethics Committee of Hospital de Clínicas de Porto Alegre was obtained for this study under the CAAE registry number 94748218.4.0000.5327.
PopulationThe population consisted of the parents or guardians of children and adolescents with sialorrhea up to 20 years of age. The patients came from the Pediatric Airway outpatient clinic of the Otorhinolaryngology Unit of Hospital de Clínicas de Porto Alegre. Clinical information was also collected.
As proposed by Beaton et al.,6 the preliminary pilot test version was applied to a sample of 40 patients (Phase 1). At this point, issues regarding understanding and content of each question are discussed with respondents to ensure accuracy of the translated version.
The final version in Portuguese was applied to a population of 40 patients (Phase 2), in accordance with Terwee et al.7 It was applied in conjunction with the Drooling Severity and Frequency Scales (DSFS) questionnaire, which has already been used in several studies since 1988 and analyzes the severity of sialorrhea. The DSFS was used to evaluate the correlation of the questionnaires and the validity of the DIS for the Portuguese language.
Statistical analysisCronbach’s alpha for the whole scale, corrected item-total correlations and Cronbach’s alpha if item is deleted were employed to evaluate the scale reliability. According to Nunnally’s criteria,8 an α ≥ 0.70 should be regarded as an acceptable reliability. Correlation between different scales was performed with Pearson or Spearman correlation test, according to variable distribution.
Exploratory Factorial Analysis (EFA) was performed with all 10 items of the scale. The Bartlett’s test of Sphericity9 was calculated to verify if the correlations between the original variables raised are sufficient so that the EFA has utility in the estimation of the common factors. Initial Kaiser-Meyer-Olkin (KMO)10,11 was performed to evaluate the sampling adequacy to carry out factor analysis of the 10 DIS variables. Factor were extracted through the principal component extraction with varimax rotation. Factor loadings equal or higher to 0.3 were considered satisfactory. For factor number determination, scree plot and parallel analysis were performed. Communalities were examined to assess how much of the variance of each item was accounted for the extracted factors.
Confirmatory Factorial Analysis (CFA) was used to evaluate the goodness-of-fit of the present data regarding that described in literature. A first model was drawn considering all 10 items loading into one single latent variable. The second model, based on EFA within this study, considers that two latent variables receive loading from 5 items each. We have chosen to use multiple goodness-of-fit analysis approaches in this study (approximate fit, incremental fit and residual-based indexes): Chi-Square value (x2), the Root Mean Square Error of Approximation (RMSEA), the Comparative Fit Index (CFI), the Tucker-Lewis Index (TLI) and the Standardized Root Mean Residual (SRMR).
For the purpose of statistical analyses, we have used SPSS 22.0 for Mac (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.) for EFA, Monte Carlo PCA for Parallel Analysis (Watkins, M.W.,2000). Monte Carlo PCA for Parallel Analysis (Computer Software). State College, PA: Ed & Psych Associates.) and Classical & Bayesian Instrument Development (Byron Gajewski; Beta Version) online (http://biostats-shinyr.kumc.edu/CBID/) for CFA.
ResultsThere were no conceptual differences in the back-translation compared to the original version. The final Portuguese version of the DIS was then approved in format and content.
A total sample of 40 subjects (and respective respondent parents) was enrolled for this validation protocol, as recommended by Terwee et al.7 Population characteristics are shown in Table 1.
Population characteristics (40 patients).
| Parameter | Descriptiona |
|---|---|
| Gender (male) | 20 (50%) |
| Age (months) | 42.5 (19.75 − 150.75) |
| Patient weight (Kg) | 16 (9.05 − 26.25) |
| Syndromic disorders | 12 (30%) |
| Current use of anticholinergic drug | 7 (17.5%) |
| Previous botulinum toxin application | 15 (37.5%) |
| Hospitalization within the last year | 30 (75%) |
| Number of hospitalizations within the last year (for those answering positively the last item) | 2.5 (1 − 4) |
| Length of stay (inpatient days) | 17 (10.25 − 75) |
| Need for antimicrobial therapy | 31 (77.5%) |
| Any hospitalization due to pneumonia | 24 (60%) |
| Current tracheostomy | 16 (40%) |
| Current feeding route | |
| Oral | 4 (10%) |
| Nasoenteral/Nasogastric tube | 17 (42.5%) |
| Gastrostomy | 19 (47.5%) |
| RSSFD | |
| Severity | 5 (3 − 5) |
| Frequency | 4 (3.25 − 4) |
The mean DIS value for the whole population was 51.77 (SD = 16.13). The internal consistency obtained with Cronbach’s alpha indicated a value of 0.72 for the entire sample. Table 2 presents DIS individual item mean scores, SD, corrected item-total correlation coefficients and Cronbach’s alphas if the item is deleted. Mean individual item scores ranged from 1.48 (Item 7. “Quão envergonhada a criança parecia estar por causa da baba?”) to 8.08 (Item 2. “Qual era a quantidade da baba?”). Items showing the lowest corrected item-total correlation coefficient were 7 (“Quão envergonhada a criança parecia estar por causa da baba?”) and 9 (“Em que medida a baba afetou a vida de seu filho?”), standing below acceptance criterion value of 0.30. The exclusion of those items 7 and 9 from the questionnaire would result in a Cronbach’s alpha value of 0.74 and 0.76, respectively.
Drooling Impact Scale (DIS) mean scores (M) and Standard Deviation (SD) for individual items, corrected item-total correlation (CTIC) and internal consistency (Cronbach's alpha) if the item is deleted (ICIID).
| Question (Portuguese) | M | SD | CTIC | ICIID |
|---|---|---|---|---|
| 1. “Com que frequência seu filho produziu baba?” | 7.58 | 2.86 | 0.50 | 0.68 |
| 2. “Qual era a quantidade da baba?” | 8.08 | 2.53 | 0.70 | 0.66 |
| 3. “Quantas vezes por dia você teve de trocar o babador ou a roupa da criança por causa da baba?” | 4.80 | 3.32 | 0.50 | 0.68 |
| 4. “Quão desagradável era o cheiro da saliva no seu filho?” | 2.55 | 2.72 | 0.30 | 0.71 |
| 5. “Quanta irritação na pele seu filho apresentou por causa da baba?” | 2.43 | 2.74 | 0.40 | 0.70 |
| 6. “Com que frequência você teve de secar a boca da criança?” | 7.65 | 2.73 | 0.66 | 0.66 |
| 7. “Quão envergonhada a criança parecia estar por causa da baba?” | 1.48 | 1.74 | 0.06 | 0.74 |
| 8. “Com que frequência você teve de secar ou limpar a saliva deixada em artigos domésticos, como brinquedos, móveis e computadores?” | 4.98 | 3.74 | 0.50 | 0.68 |
| 9. “Em que medida a baba afetou a vida de seu filho?” | 6.55 | 3.57 | 0.05 | 0.76 |
| 10. “Em que medida a baba de seu filho afetou a sua vida e a de sua família?” | 5.70 | 3.65 | 0.27 | 0.72 |
The Bartlett’s test of sphericity was significant (p < 0.0001), confirming correlation among variables tested. Kaiser-Meyer-Olkin (MO) measure of sampling adequacy revealed a value of 0.72, indicating that the correlation matrix was reasonably suitable for factor analysis. Initial Eigenvalues and the Scree plot suggested a three-factor structure, but Parallel analysis suggested a two-factor solution. As this last approach is considered less prone to overestimate the number of latent factors, we have proceeded with a two-factor confirmatory factor analysis. Factor loadings and communalities for this solution are shown in Table 3. The first factor was responsible for 33.78% of the variance with an Eigenvalue of 3.38. The second factor explained 16.1% of the variance with an Eigenvalue of 1.61. The first factor apparently encompassed items relating to an objective frequency of drooling events and consequences, while the second factor seemed to embrace a more subjective experience on how drooling affected the patient and respective caretakers. Cronbach’s alpha for the first and second factor was 0.74 and 0.61, respectively.
Principal axis factoring analysis factor loading and communalities (h2) of the 10 Drooling Impact Scale (DIS) items following varimax rotation.
| Question | Factor 1 | Factor 2 | h2 |
|---|---|---|---|
| 3. “Quantas vezes por dia você teve de trocar o babador ou a roupa da criança por causa da baba?” | 0.82 | 0.00 | 0.67 |
| 8. “Com que frequência você teve de secar ou limpar a saliva deixada em artigos domésticos, como brinquedos, móveis e computadores?” | 0.72 | 0.11 | 0.54 |
| 1. “Com que frequência seu filho produziu baba?” | 0.69 | 0.15 | 0.50 |
| 4. “Quão desagradável era o cheiro da saliva no seu filho?” | 0.63 | -0.21 | 0.44 |
| 5. “Quanta irritação na pele seu filho apresentou por causa da baba?” | 0.55 | 0.08 | 0.31 |
| 9. “Em que medida a baba afetou a vida de seu filho?” | -0.28 | 0.75 | 0.64 |
| 6. “Com que frequência você teve de secar a boca da criança?” | 0.51 | 0.69 | 0.74 |
| 2. “Qual era a quantidade da baba?” | 0.57 | 0.65 | 0.75 |
| 10. “Em que medida a baba de seu filho afetou a sua vida e a de sua família?” | 0.16 | 0.53 | 0.30 |
| 7. “Quão envergonhada a criança parecia estar por causa da baba?” | -0.04 | 0.32 | 0.10 |
| Eigenvalue | 3.38 | 1.61 | |
| Variance (%) | 33.78% | 16.1% | |
| Cronbach’s alpha | 0.74 | 0.61 |
Final fit indices for the two DIS factor models (Model 1 = 1 factor, Model 2 = 2 factors) tested according to confirmatory factor analysis are described in Table 4. The Chi-Square (x2) p-value for models 1 and 2 are 0.073 and 0.577, respectively. Although both models did not reject the null hypothesis that the model fits the true covariance structure from the population, evaluated indices showed systematically better fit results for model 2 (2 factors) compared to model 1.
Fit indices for the two Drooling Impact Scale (DIS) factor models tested according to confirmatory factor analysis.
| Model | x2 | df | RMSEA | CFI | TLI | SRMR |
|---|---|---|---|---|---|---|
| Model 1 | 47.837 | 35 | 0.096 | 0.840 | 0.794 | 0.106 |
| Model 2 | 31.784 | 34 | 0 | 1.0 | 1.037 | 0.089 |
RMSEA, Root Mean Square Error of Approximation; CFI, Comparative Fit Index; Tucker-Lewis Index (TLI); SRMR, Standardized Root Mean Residual (SRMR).
There are quantitative and qualitative methods to assess the QOL of patient and caretaker concerning the impact of salivation. Qualitative scales, such as DSFS, The Visual Analogue Scale (VAS)12 and DIS are scales that rate scores and give a subjective impression.
The DSFS is based on the Thomas-Stonell and Greenberg scale1 and assesses the severity of sialorrhea compromise. VAS measures the salivation reference rate where “0” indicates normal salivation and “100”, extremely high salivation rate.12 The DIS assesses the impact of sialorrhea on the quality of life of the caretaker and the patient. None of these or any other instrument was found with a validated translation into Brazilian Portuguese.
After completing the steps described in the methods section and according to the definition of the measurement properties proposed by the Mokkink et al. in 2010,13 the final Portuguese version was tested to verify its equivalence with the original questionnaire. The ideal population is in the range of 3 to 5 respondents for each question in a translated questionnaire. The DIS has 10 questions, therefore an adequate population for this study would be between 30 and 50 participants,7 justifying our final enrollment of 40 respondents.
The Brazilian Portuguese language version of the DIS questionnaire showed an acceptable internal consistency, with a Cronbach’s alpha above 0.7. Regarding individual analysis of the items in the scale, it was found that mainly Item 7 (“Quão envergonhada a criança parecia estar por causa da baba?”) and Item 9 (“Em que medida a baba afetou a vida de seu filho?”) showed poor correlation with the remaining items, and their exclusion would potentially result in a higher global Cronbach’s alpha. Item 7 also showed the lowest communality value (0.1) contributing poorly to the scale variance. Both questions are directed to a subjective experience of how much drooling affects interaction between patient and caretakers. A hypothesis is that attributing higher scores at those items would elicit a perception of directing negative feelings towards the patient, and consequently could have discouraged caretakers in doing so.
Upon exploratory factorial analysis, a two-factor structure was identified: “objective” × “subjective” experience on drooling. This solution seemed reasonable when considering the DIS questions. Confirmatory factorial analysis confirmed superiority of a two-factor model base on different fit indices.
As a validated and globally utilized scale, there is no intention in changing its original structure. The purpose is solely a better understanding on how this scale performs not only in our language, but also in our culture. Exploratory factorial analysis also allowed for a deeper appreciation of latent factors existing within the scale framework.
Validation of this instrument allows physicians and other personnel involved in the care of these patients to perform a better management of patients experiencing drooling. With this tool, we are now able to guide routines and provide guidelines both before and after the different kinds of treatments in order to improve the general well-being of the patient and his family.
ConclusionDIS has been successfully translated to Brazilian Portuguese language. Although some items have shown poorer correlation results, whole consistency was considered acceptable.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.