Kawasaki disease (KD) is an acute systemic vasculitis of unknown etiology, also called an acute febrile mucocutaneous lymph node syndrome, which is first identified by Dr. Tomisaku Kawasaki in 1967. This disease is characterized by fever, erythematous rash, cervical lymphadenitis, strawberry tongue, nonpurulent conjunctivitis and desquamation of hands and feet. Of these symptoms, the most infrequent symptom is cervical lymphadenitis (50%–75%) while the others occur in 90% of the cases.1 Cervical lymphadenitis as initial presenting symptom occurs in only 12% of the times2 and may be misdiagnosed as other disease entity.
KD involves all blood vessels, especially medium sized vessels like the coronary artery. In this regard, KD may cause severe complications with delayed treatment.
Image of retropharyngeal low-density area, in addition to retropharyngeal abscess and edema is usually associated to a fatal condition if not appropriately treated. Otolaryngologists are familiar with this disease and may treat it with surgical draining of the abscess, preventing blockage of the airway.
KD with retropharyngeal abscess is a very rare disease and can be a challenge to many otolaryngologists. We experienced a 9 year-old girl who presented as a retropharyngeal abscess, thus resulting in delayed diagnosis.
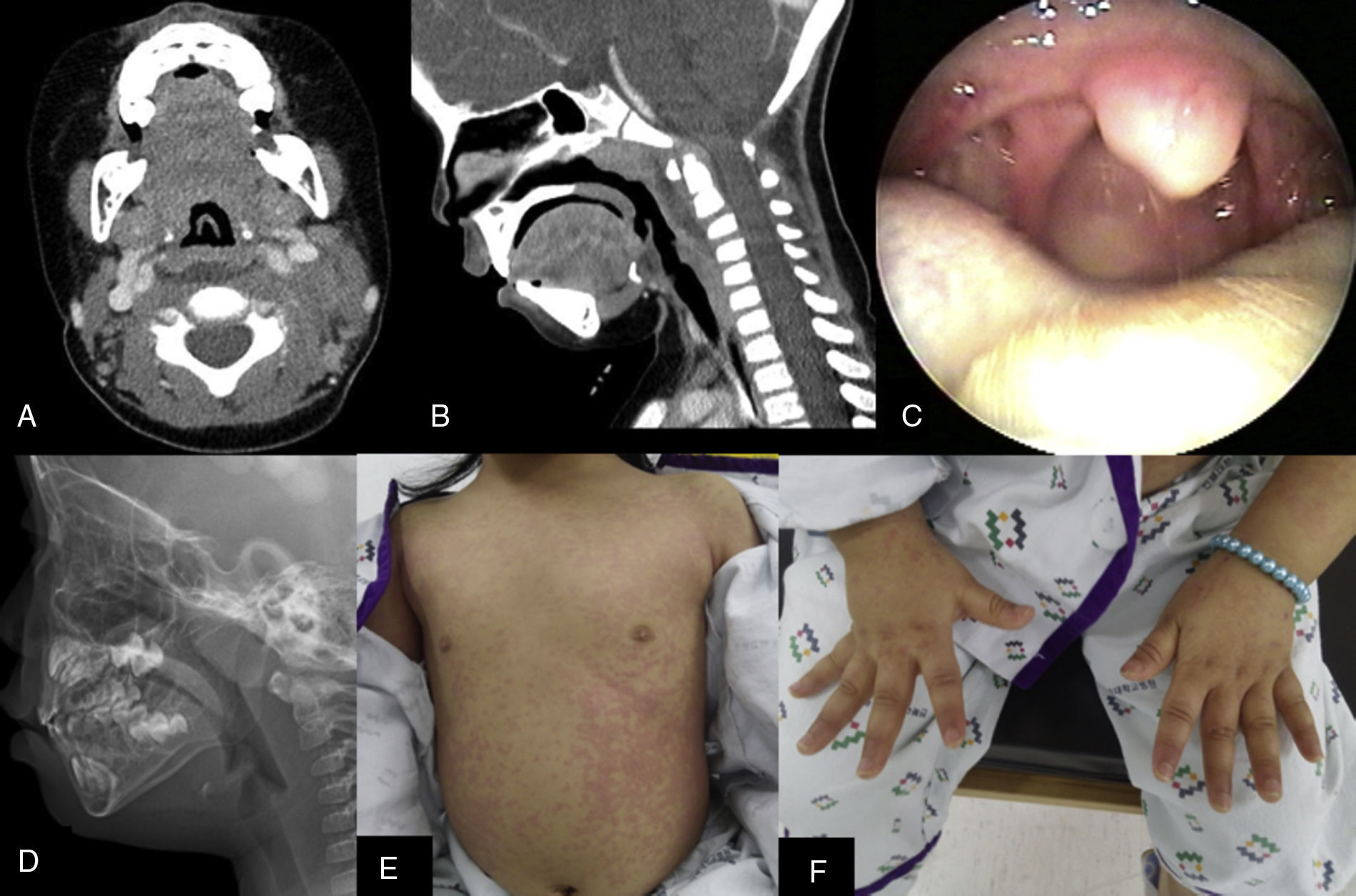
Case reportA 9-year-old girl was transferred to our hospital because of a retropharyngeal abscess. She had suffered from fever and sore throat, and had seeked for a secondary health care center. Computed tomography (CT) showed a retropharyngeal abscess with bilateral cervical lymphadenopathy (Fig. 1A and B). She was admitted in the intensive care unit and treated with amoxicillin-clavulanate (120mg/kg/day) and clindamycin (100mg/kg/day) for 4 days. However, her symptoms did not improve with this conservative therapy, and the patient was transferred to a tertiary medical center. On admission, cardiac murmur was audible and breathing sounds were clear without crackles. CT was rechecked and showed a retropharyngeal low density area from C2 to C5 with bilateral cervical lymphadenitis. Simple lateral neck X-ray revealed a mild soft tissue thickening of the retropharyngeal area. The abscess pocket had been decreased when comparing with the previously done CT at the secondary health care unit. (4cm×1cm→2cm×0.5cm) White blood cell count (WBC) was 14,040mm3 (neutrophil 11,170), erythrocyte sedimentation rate (ESR) 58mm/h, C reactive protein (CRP) was elevated, 165mg/dL. Endoscopic findings consisted of enlarged tonsils, injected throat, and mild narrowed airway. She had no dyspnea. (Fig. 1C) We treated the patient with high dose ceftriaxone (80mg/kg/day) and metronidazole (22.5mg/kg/day). On day 2, fever had disappeared and WBC, CRP had decreased. However, the fever reappeared on the third day of hospitalization, twice a day. Urine culture and blood culture were all negative. Her inflammatory lab results had ameliorated, and neck lateral X-ray showed decreasing of the retropharyngeal edema, but spiking fever had not disappeared in a similar fashion. Her lip was fissured and the color of the tongue became red on 3rd admission day; we referred her to the department of pediatrics, suggesting a diagnosis of scarlet fever or Kawasaki disease. However, the pediatrician believed that the focus of the fever was the retropharyngeal abscess, not from an inflammatory disease. Although the neck lateral X-ray revealed no increase of thickness in the retropharyngeal space, the patient was inevitably treated with high dose of antibiotics (Fig. 1D). WBC and CRP decreased with this therapy but her fever was not controlled.
(A) Axial CT view revealed 4cm×1cm hypodense area in the retropharyngeal space. (B) Coronal CT showed 1cm×4cm sized hypodense area in the retropharyngeal space, from C2 level to C5 level. (C) Mild injected throat and grade II tonsil was noted on the endoscopy. Swelling of post pharyngeal wall was also identified. (D) Simple neck X-ray revealed mild swelling of retropharyngeal soft tissue and no interval change compared with previous film. (E) Polymorphous erythematous rash appeared on the anterior and posterior trunk. (F) Erythematous rash and edema appeared on both hands.
On the 6th day, erythematous rash turn up on the trunk, in both hands and feet (Fig. 1E and F). The rash was polymorphous with no vesicles in association. WBC and CRP had been normalized, 7130mm3 and 16.8mg/dL, respectively. Viral lab tests were all negative.
Desquamation of hands and feet appeared on the 8th day of hospitalization and her echocardiogram proved to be normal. The pediatrician made a diagnosis of atypical Kawasaki disease and administered high dose of intravenous immunoglobulin (IVIG) (2.5g/kg/day) and aspirin (100mg/kg/day). Fever and rash did not disappear within 48h. On day 10, booster steroid injection (30mg/kg/day) was tried for two days and the fever finally disappeared on the 11th day. On the 13th day, desquamation of hands and feet disappeared and the patient was discharged.
After 6 weeks follow up, the patient was uneventful, echocardiogram revealed no abnormality of the coronary artery, with normal ventricular motion.
DiscussionThere are no specific diagnostic tests for Kawasaki disease. The diagnosis depends on the presence of fever for more than 5 days and together with 4 out of five principal criteria: (1) bilateral nonexudative conjunctival injection, (2) polymorphous exanthema, (3) lips or oral cavity changes including fissuring of the lips, strawberry tongue and/or mucosal hyperemia, (4) changes in the extremities including erythema of the palms and soles, nonpitting edema of hands and feet, or desquamation and (5) cervical lymphadenopathy over 1.5cm in diameter. Other disease causing the symptoms must be excluded.3
Delayed diagnosis may be disastrous. It involves middle sized arteries, and severe complications like coronary artery aneurysm or myocardial infarction can happen.4 Coronary artery aneurysm appears in 7% of children of KD and myocardiac infarction develop in 0.2%–0.5% of these children.
Despite of these serious complications, the problem is that the only diagnostic tools are the symptoms and signs. No specific diagnostic test has been developed for KD. Atypical KD is a disease that symptoms do not occur simultaneously or not met the above described criteria. It involves peritonsillar abscess, retropharyngeal abscess, renal impairment, acute otitis media, pulmonary infiltrates, abdominal pain, arthritis and lymphadenitis.5 Even in atypical KD like this patient, early diagnosis is very important. It is meaningful to investigate the clinical characteristics of atypical KD with retropharyngeal abscess or edema.
Our case had an afebrile period of 2 days. There are two other case reports of afebrile period in KD before the IVIG treatment.5,6 It can be an important clue from several case reports of atypical KD with retropharyngeal abscess. Proper management including wide spectrum antibiotics and surgery can proceed before the diagnosis of KD, however it is crucial to administer early IVIG treatment after the final diagnosis, in order to prevent from serious complications.
ConclusionAny children who present with fever and lymphadenitis, color change of skin and mucosa including oral cavity and conjunctiva should be observed carefully. Even though these symptoms do not appear simultaneously, otolaryngologists should rule out the atypical KD. In addition, afebrile period and retropharyngeal abscess are also to be considerate in atypical KD.
Conflicts of interestThe authors declare no conflicts of interest.
This paper was supported by the Fund of Biomedical Research Institute, Chonbuk National University Hospital.
Please cite this article as: Kim JS, Kwon SH. Atypical Kawasaki disease presenting as a retropharyngeal abscess. Braz J Otorhinolaryngol. 2016;82:484–6.