It is an erroneous but commonly held belief that intracranial complications (ICCs) of chronic and acute otitis media (COM and AOM) are past diseases or from developing countries. These problems remain, despite improvements in antibiotic care.
ObjectiveThis paper analyzes the occurrence and clinical characteristics and course of the main ICCs of otitis media (OM).
MethodsRetrospective cohort study of 51 patients with ICCs from OM, drawn from all patients presenting with OM to the emergency room of a large inner-city tertiary care hospital over a 22-year period.
Results80% of cases were secondary to COM of which the incidence of ICC was 0.8%; 20% were due to AOM. The death occurrence was 7.8%, hearing loss in 90%, and permanent neurological sequelae in 29%. Patients were 61% male. In the majority, onset of ear disease had occurred during childhood. Delay of diagnosis of both the initial infection as well as the secondary ICC was significant. ICCs included brain abscess and meningitis in 78%, and lateral sinus thrombosis, empyema and otitic hydrocephalus in 13%, 8% and 1% of cases, respectively. Twenty-seven neurosurgical procedures and 43 otologic surgery procedures were performed. Two patients were too ill for surgical intervention.
ConclusionICCs of OM, although uncommon, still occur. These cases require expensive, complex and long-term inpatient treatment and frequently result in hearing loss, neurological sequelae and mortality. It is important to be aware of this potentiality in children with COM, especially, and maintain a high index of suspicion in order to refer for otologic specialty care before such complications occur.
É uma crença comum, porém errônea, que complicações intracranianas (CICs) de otite média tanto aguda (OMA) quanto crônica (OMC) sejam doenças do passado ou de países em desenvolvimento. No entanto, esses problemas continuam, apesar de melhorias na terapia antimicrobiana.
ObjetivoAnalisar a ocorrência, as características clínicas e a evolução das principais CICs secundárias às otites médias (OM).
MétodoEstudo de coorte retrospectivo de 51 pacientes com CIC secundárias a OM, provenientes do pronto-socorro de um Hospital Universitário ao longo de um período de 22 anos.
ResultadoNo total, 80% dos casos de CICs foram secundários a OMC, cuja incidência foi de 0,8%, e apenas 20% foram secundárias a OMA. A letalidade foi de 7,8%, perda auditiva em 90%, com sequela neurológica permanente em 29%. Dentre os pacientes, 61% eram do sexo masculino. Na maioria, o início da doença otológica tinha ocorrido durante a infância. A demora no diagnóstico, tanto da infecção primária como da complicação secundária, foi significativa. CICs, incluindo abscesso cerebral e meningite, corresponderam a 78%, e trombose do seio lateral, empiema e hidrocefalia otítica em 13%, 8% e 1% dos casos, respectivamente. Foram realizados 27 procedimentos neurocirúrgicos e 43 cirurgias otológicas. Dois pacientes não apresentavam condições clínicas para a intervenção cirúrgica.
ConclusãoCICs de OM, embora incomuns, ainda ocorrem. Esses casos exigem tratamento hospitalar oneroso, complexo e de longo prazo, e frequentemente resultam em perda auditiva, sequelas neurológicas e mortalidade. É importante estar ciente dessa potencialidade especialmente em crianças com OMC e manter um alto índice de suspeita, encaminhar para avaliação otológica e antecipar a ocorrências de tais complicações.
Otitis media (OM) is one of the most prevalent infectious diseases worldwide: over 80% of children have acute OM (AOM) once before age 3, and 40% have 6 or more recurrences by age 7.1 Globally, OM is the third most important cause of hearing loss (HL), with a prevalence of 30.82 per 10,000.1,2 In developed countries, OM accounts for the largest number of non-well-child doctor visits and is the primary reason for childhood antibiotic prescriptions. Children spend a mean of 90 days on antibiotics for OM in their first two years of life.3
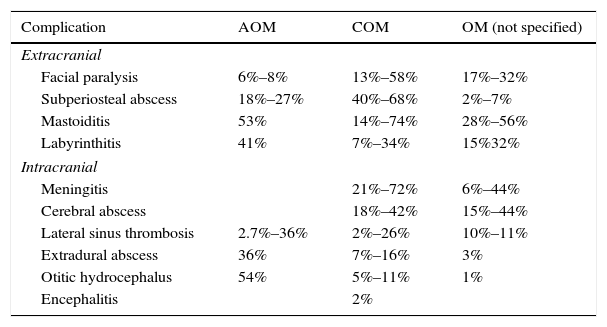
AOM, which is generally self-limited, has an incidence of 10.9%. Chronic OM (COM) is more difficult to diagnose and treat and has an incidence of 4.8%,4–6 OM complication rates are as high as 12.5%6,7 and can be extracranial and/or intracranial. The most common extracranial complications of OM include facial paralysis, subperiosteal abscess, mastoiditis, and labyrinthitis. The most common intracranial complications (ICCs) of OM are meningitis, cerebral abscess, lateral sinus thrombosis (LST), extradural abscess, otitic hydrocephalus, and encephalitis.8–11 Reported incidences for these complications (summarized in Table 1) range widely.
Complication rates from otitis media.
| Complication | AOM | COM | OM (not specified) |
|---|---|---|---|
| Extracranial | |||
| Facial paralysis | 6%–8% | 13%–58% | 17%–32% |
| Subperiosteal abscess | 18%–27% | 40%–68% | 2%–7% |
| Mastoiditis | 53% | 14%–74% | 28%–56% |
| Labyrinthitis | 41% | 7%–34% | 15%32% |
| Intracranial | |||
| Meningitis | 21%–72% | 6%–44% | |
| Cerebral abscess | 18%–42% | 15%–44% | |
| Lateral sinus thrombosis | 2.7%–36% | 2%–26% | 10%–11% |
| Extradural abscess | 36% | 7%–16% | 3% |
| Otitic hydrocephalus | 54% | 5%–11% | 1% |
| Encephalitis | 2% | ||
AOM, acute otitis media; COM, chronic otitis media; OM, otitis media. Refs.: 8–12,17,27.
Despite the introduction of effective antibiotic therapy, the rate of ICC from OM is still about 8%. Anaerobic bacteria play a significant role.12 Thirty percent of complications from OM are intracranial; of ICCs, 5–26% result in mortality.13–15 ICCs of AOM usually develop rapidly and are often recognized and treated promptly, with reasonable recovery of function.16 Conversely, early COM is often unrecognized and untreated, and it may take years to develop complications, which are often hard to diagnose and are much more severe and life-threatening.
There is persistent inaccuracy in diagnosis of AOM by primary care physicians (PCPs) – pediatricians, family physicians, general practitioners, emergency room physicians, and otolaryngologists. In a study of 590 children, only 62% were diagnosed accurately by their PCPs, more frequently in complicated rather than simple AOM.17 Using video-recorded otoscopy of AOM, OM with effusion (OME), and normal, otolaryngologists were correct 74±16% of the time; pediatricians, 51±11%; and general practitioners, 46±21%.18 There is a lack of formalized PCP resident education in OM diagnosis, despite this being the most pediatric diagnosis.19,20 Diagnostic accuracy is most important in COM, to prevent the higher likelihood of intra- and extra-cranial complications.13 However, the average age at diagnosis for even congenital cholesteatoma is 4–5 years old.21 Even after entering otolaryngologic care, there is an average of 3.2 years delay in diagnosis of pediatric cholesteatoma.22 This unrecognized, and therefore untreated, COM can cause significant complications later on.
A 15-year review of negligence claims in the United Kingdom found that otologic claims made up 137 (26%); of the 97 successful claims, 15 were related to misdiagnosis/delayed diagnosis, with COM being the condition most frequently missed, and 4 additional cases were claims for morbidity due to delayed surgery.23
Even complications are difficult to diagnose: a study of four cases of pediatric lateral sinus thrombosis (LST), 3 from OM and 1 from tonsillitis, reported on the non-specific presentation and propensity to miss early diagnosis.24 In a US tertiary care hospital, asymptomatic ICCs were found in 8 of 11 children with acute mastoiditis treated over a one-year period.25 The clinical evolution of LST is very variable and is often missed because of lack of “pathognomonic” features, such as picket fence fever, which are, in fact, infrequently seen.26
ICCs of AOM and COM represent life-threatening situations and require immediate action. Due to atypical manifestations and the possibility of hidden expression, often related to the previous use of antibiotics, the prompt identification of ICCs requires a high clinical index of suspicion and a team approach by physicians, including PCPs, infectious disease specialists, otolaryngologists, radiologists, and neurosurgeons.27–29
Given the high incidence of OM, the inaccuracies in diagnosis, and the possibility of life threatening sequelae, this is an important ongoing problem.30
The aim of this study is to describe the epidemiological and clinical aspects of ICCs resulting from OM, to analyze the progression of the condition and to determine the relevant aspects that should be evaluated to minimize morbidity and mortality.
MethodsThis is a retrospective review of clinical data that was carried out in a teaching and research institution. Fifty-one cases of ICC from OM identified from one emergency room (ER) over a 22-year period, from 1990 to 2012, were analyzed. In addition, the single year 2010 was selected for more detailed analysis of the incidence of ear infections and their complications as they presented to the ER of the tertiary referral hospital with 743 inpatient beds and 366,488 emergency room (ER) visits in the representative year 2010.
The treatment team included neuroradiology, neurosurgery, pediatrics, infectious disease, medical intensive care, and otolaryngology physicians. Specific tests, such as computerized tomography (CT) scan, magnetic resonance imaging (MRI), magnetic resonance (MR) angiography, and lumbar puncture were tailored to the patient and the presentation. The outcomes considered for analysis included: death, other permanent sequelae, and deafness. Patients were stratified by gender, type of otitis, and type of intracranial complication.
Data were collected in four main categories:
- 1.
Demographic data: age at presentation, gender.
- 2.
Disease data: the type of otitis media – AOM or COM, which was divided into non-cholesteatomatous COM (NCCOM) and cholesteatomatous COM (CCOM); patient age at first COM diagnosis; duration of illness (time between initial symptoms of OM and the development of the ICC); time delay to ICC diagnosis (interval between presentation with initial ICC symptoms and diagnosis of the ICC); the type of ICC, the bacteriology involved, and results of other specific tests as outlined above.
- 3.
Treatment data: the clinical and surgical treatments adopted in each case. Preoperative imaging findings and suspicions were confirmed during surgery.
- 4.
Outcome data: the duration of hospitalization, hearing status post-treatment, neurological sequelae and mortality rate.
Statistical analysis was performed by calculating the relative risk and correlation coefficient of Yule, with subsequent calculation of the X2 test and Pearson association. Statistical significance was set at 5% alpha with 1 degree of freedom (critical value of 3.84).
This study was approved by the Institutional Ethics Committee (protocol: 0352/08).
ResultsDemographic dataIn 2010, there was a total of 21,096 emergency room (ER) visits related to ear nose and throat (ENT) complaints. 1816 of these patients were diagnosed with otitis media, for an incidence in our ER of 8.6%. Of the 1816 OM patients, 52% were female, and the mean age was 31 years.
Disease dataOf the 1816 cases of OM seen in 2010, 1224 (67%) were AOM, and 592 (33%) were COM. This equates to 5.8% and 2.8% of all ER ENT visits, respectively. In the single year 2010, there were two cases of ICC secondary to COM, and no case secondary to AOM.
Over the entire 22-year period of the study, the ENT service followed 5667 patients with COM, 3060 (54%) female, and 2607 (46%) male, with a mean age of 32 years (range: 1–100). During this period, 51 patients had ICC secondary to OM, 31 (61%) of the ICC patients were male, 20 were female, and the mean age of the patients at the time of ICC diagnosis was 27 years.
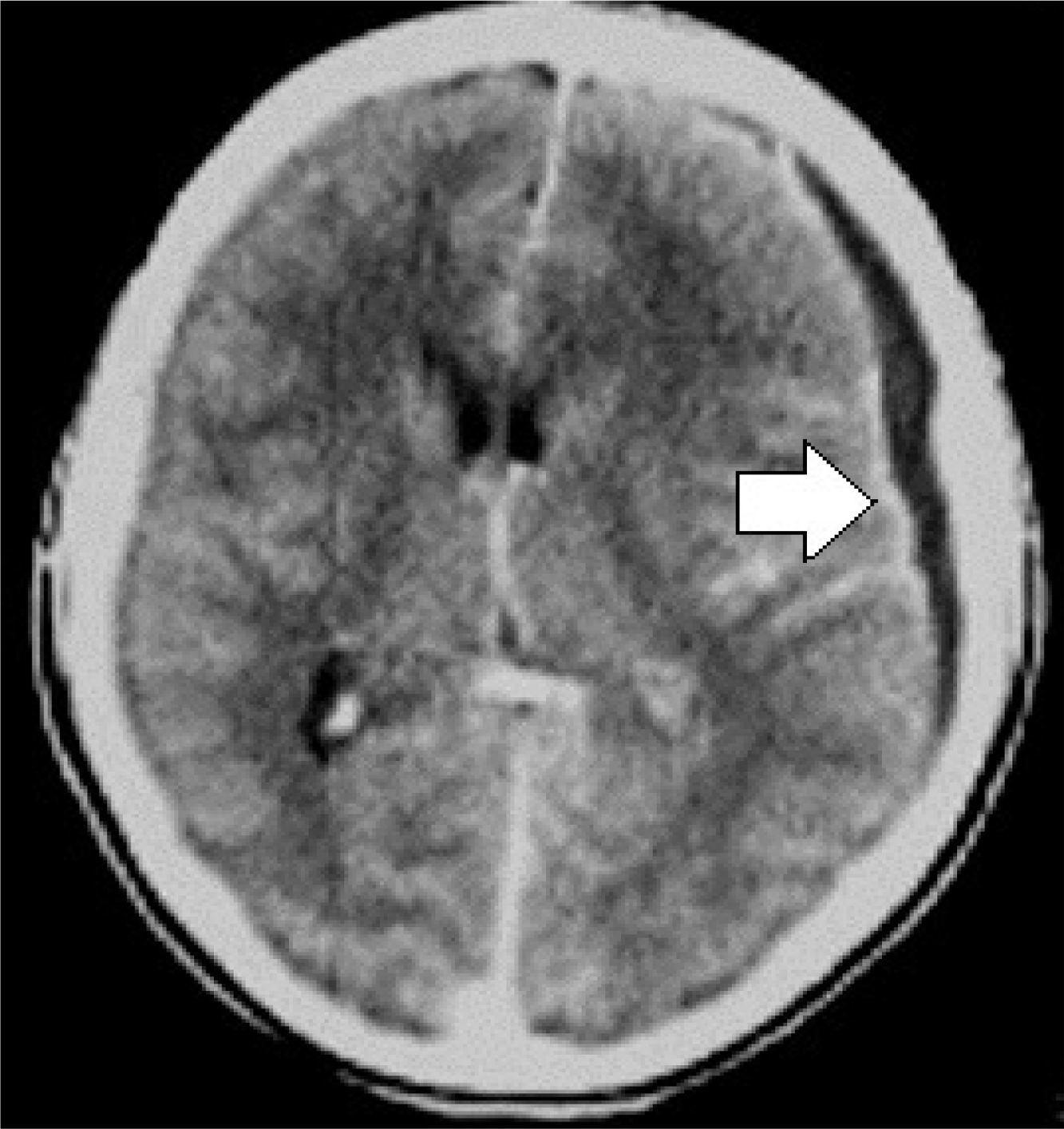
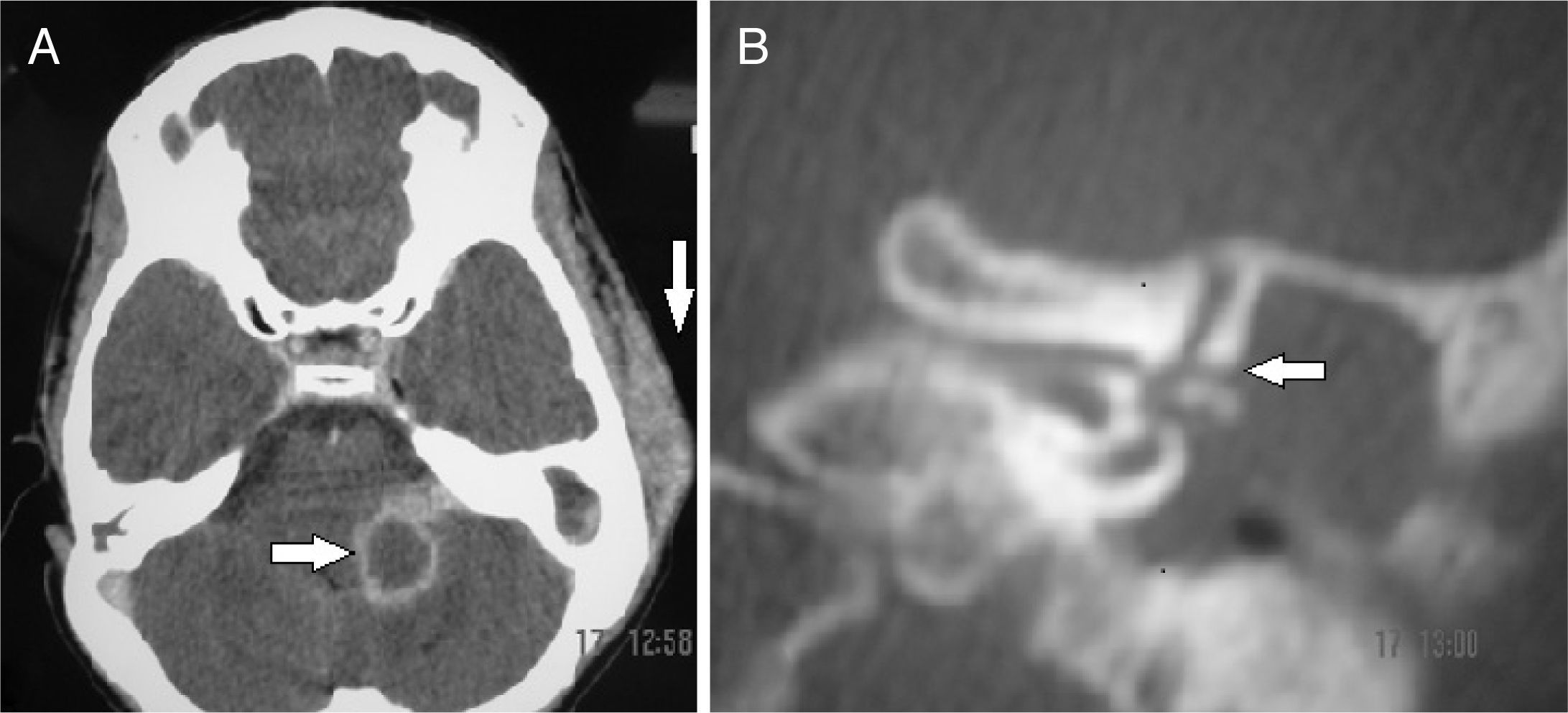
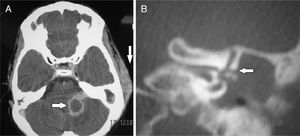
ICCs were related to AOM in 10 cases and COM in 41 cases, with a 0.8% incidence rate for the chronic cases, with CCOM in 39 cases and NCCOM in 2 cases. The mean age of ear disease onset was 11 years in patients with COM. The mean age at the time of ICC diagnosis was 30 years for AOM patients, and 26 years for COM patients. The mean period between onset of COM and manifestation of the intracranial complication was 15 years. The time delay for ICC diagnosis (the interval between the initial ICC symptoms and definitive diagnosis) was 25 days in AOM cases and 34 days in COM cases. Thirty patients presented with two or more concomitant ICCs, totaling 84 different intracranial complications in 51 patients. Cerebral abscesses and meningitis represented 78% of all ICCs, followed by empyema, lateral sinus thrombosis and otitic hydrocephalus (Figs. 1 and 2). The great majority of cerebral abscesses were located in the vicinity of the petrous bone: the temporal lobe and cerebellum were involved in 62% and 38% of cases, respectively. Proteus mirabilis, Enterococcus, Pseudomonas aeruginosa, Staphylococcus aureus and extended-spectrum beta-lactamase Klebisiella were the most common microorganisms in COM-related ICC, and Pneumococcus, Haemophilus and Staphylococcus were the most common microorganisms in AOM-related ICC.
Treatment dataAll patients received intravenous antibiotics for 3–8 weeks, initially with combination therapy employing a third generation cephalosporin (ceftriaxone) and either clindamycin or metronidazole, and then adjusted as culture and sensitivity results became available. A small number of cases required vancomycin, imipenem or meropenem. Additionally, oral antibiotics were given for LST.
A total of 27 neurosurgical procedures were performed to drain cerebral abscesses, 6 for AOM and 21 for COM. Two AOM cases and 5 COM cases required two or more neurosurgical drainage procedures due to abscess recurrence. Forty-three otological surgeries were performed, 4 in AOM cases (3 tympanocentesis and 1 tympanomastoidectomy) and 39 in COM cases (35 canal walls down mastoidectomies and 4 intact canal wall tympanomastoidectomies). In 8 cases of recurrent abscess after initial neurosurgical drainage attempt, definitive drainage of the intracranial abscess was achieved through the mastoidectomy approach. This drainage into the temporal bone was performed at the same time as cholesteatoma removal. There was no recurrence in any of these 8 cases. In five additional cases, the abscess was drained only through the mastoid approach and there was no need for any neurosurgical intervention. Two patients with ICC from COM were critically ill and died before surgery could be performed.
Outcome dataThe mean time of hospitalization for patients with OM-related ICC was 34 days. Audiological evaluation could be done in only 38 patients as the poor neurological condition of the other 13 patients precluded testing. Significant hearing loss (HL) was defined according to World Health Organization (WHO) criteria as greater than 31dB in children and 41dB in adults. In the COM patients, new onset of significant HL occurred and persisted in 33 patients (in all of whom premorbid audiograms were available). Twelve patients developed deafness: 11 in the COM group, and 1 in the AOM group.
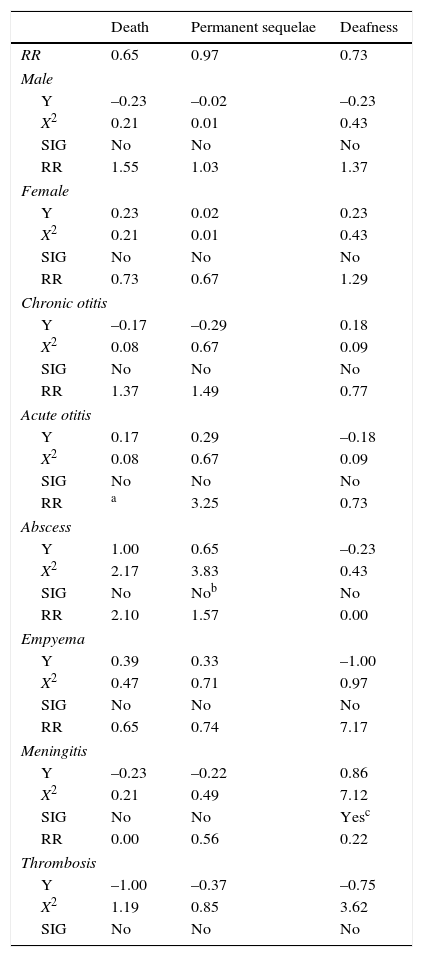
Patients with the ICC complication of meningitis had over seven time's higher risk of deafness (p<0.05). Audiological tests were obtained for 4 patients with ICCs related to AOM: 3 cases had initial conductive hearing loss which resolved after treatment, the fourth case presented with moderate to severe sensorineural hearing loss which evolved into permanent deafness. Bilateral HL was present in 10 patients; 9 with bilateral COM and 1 with bilateral AOM.
Permanent sequelae occurred in 15 patients (29.4% of all ICC cases). Cranial nerve VII and VI nerve palsies were the most common permanent consequences seen. All cases of facial palsy (n=7) were observed in patients with COM. Three patients with COM developed 2 or more neurological sequelae including hemiparesis (n=3), reduced intellectual ability (n=2), dysmetria (n=1) and dysarthria (n=1). Patients with cerebral abscess had over 3 time's higher risk of developing permanent sequelae (p<0.05).
Four of 51 patients with ICC died, yielding a mortality rate of 7.8%. All patients who died had an abscess. It is not possible to calculate the relative risk, since there were no deaths without abscess. Abscess and death had a high correlation of Yule but could not reach statistical significance, probably due to the relatively low number of events. Presence of intracranial empyema was also associated with a high (>2) relative risk of death, but this could also not reach statistical significance.
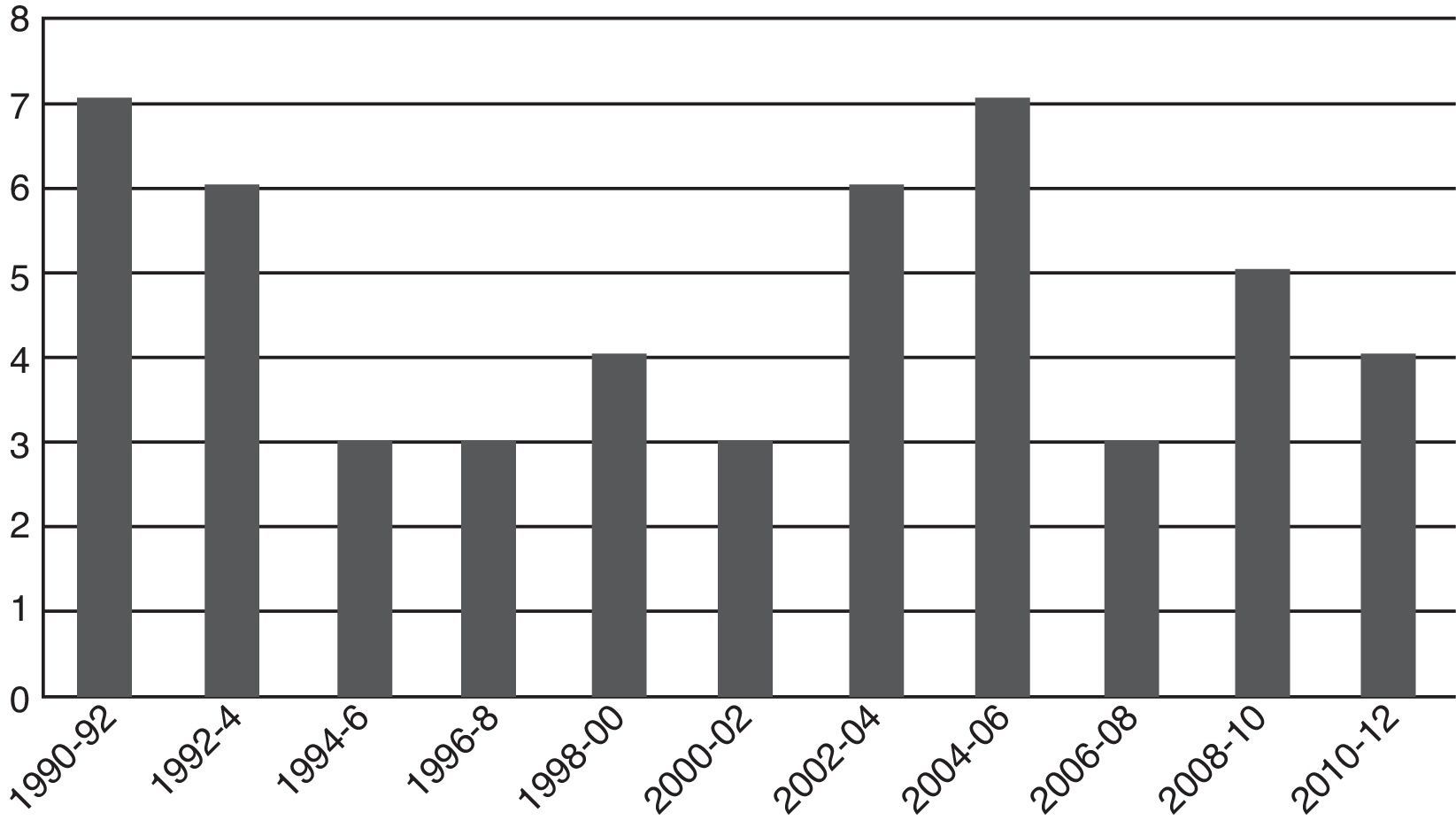
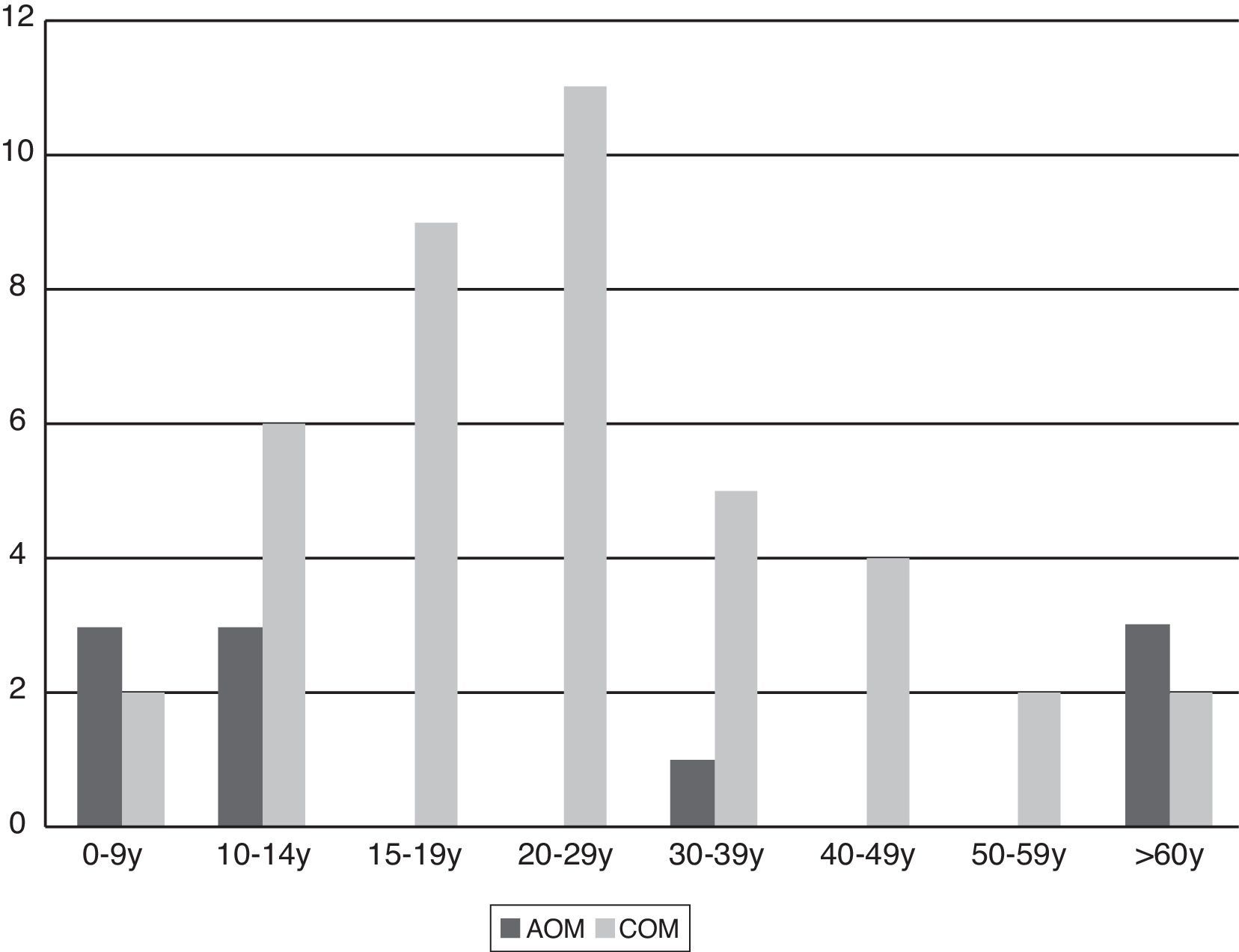
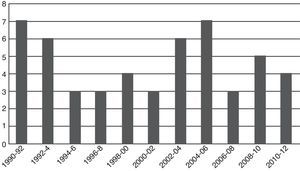
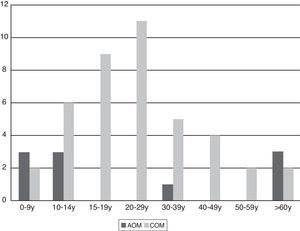
Over the 22 years, 3–7 cases of ICC from OM were seen consistently every 2 years (Fig. 3). There was a higher percentage of ICCs in cases of AOM among patients at the extremes of age (Fig. 4). A total of 60% of complications due to AOM occurred in infants and children; 30% occurred in the elderly, and only 10% occurred in non-elderly adults. On the other hand, ICCs in COM cases occurred mostly in teenagers and young adults (aged 10–39 years).
Distribution of intracranial complications cases by age intervals and type of otitis. AOM ICC cases (black bars) are seen in the first 2 decades and then after age 40, reflecting the incidence of AOM in the population overall. COM ICC cases (gray bars) are more common in the second 15 years of life, reflecting the time that it takes for unrecognized or undertreated COM to develop into an ICC.
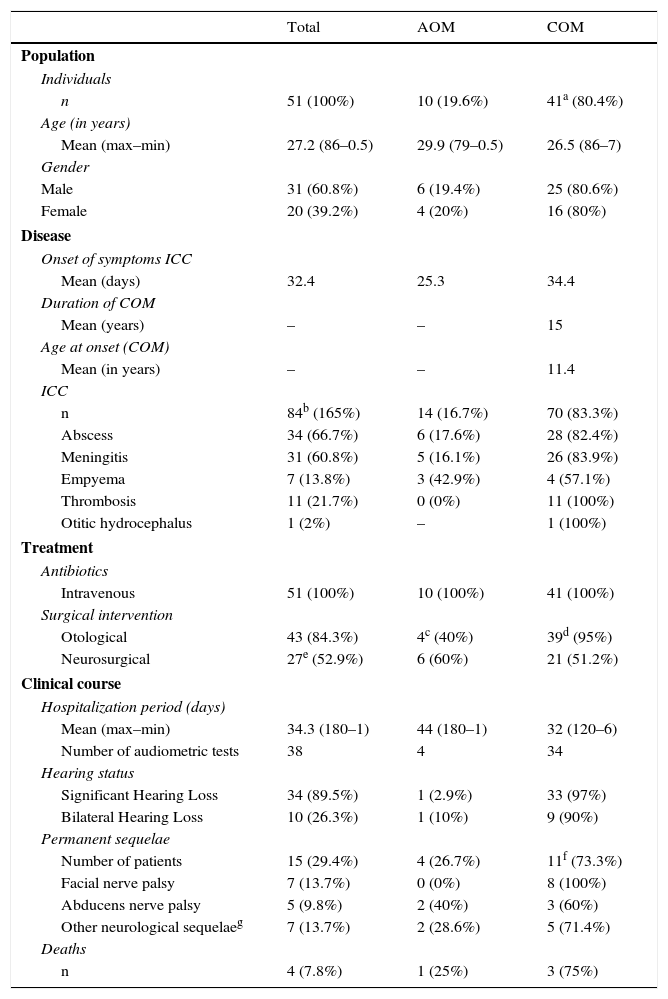
These data are summarized in Tables 2–4.
Summary of current study data regarding cases of intracranial complication secondary to otitis media.
| Total | AOM | COM | |
|---|---|---|---|
| Population | |||
| Individuals | |||
| n | 51 (100%) | 10 (19.6%) | 41a (80.4%) |
| Age (in years) | |||
| Mean (max–min) | 27.2 (86–0.5) | 29.9 (79–0.5) | 26.5 (86–7) |
| Gender | |||
| Male | 31 (60.8%) | 6 (19.4%) | 25 (80.6%) |
| Female | 20 (39.2%) | 4 (20%) | 16 (80%) |
| Disease | |||
| Onset of symptoms ICC | |||
| Mean (days) | 32.4 | 25.3 | 34.4 |
| Duration of COM | |||
| Mean (years) | – | – | 15 |
| Age at onset (COM) | |||
| Mean (in years) | – | – | 11.4 |
| ICC | |||
| n | 84b (165%) | 14 (16.7%) | 70 (83.3%) |
| Abscess | 34 (66.7%) | 6 (17.6%) | 28 (82.4%) |
| Meningitis | 31 (60.8%) | 5 (16.1%) | 26 (83.9%) |
| Empyema | 7 (13.8%) | 3 (42.9%) | 4 (57.1%) |
| Thrombosis | 11 (21.7%) | 0 (0%) | 11 (100%) |
| Otitic hydrocephalus | 1 (2%) | – | 1 (100%) |
| Treatment | |||
| Antibiotics | |||
| Intravenous | 51 (100%) | 10 (100%) | 41 (100%) |
| Surgical intervention | |||
| Otological | 43 (84.3%) | 4c (40%) | 39d (95%) |
| Neurosurgical | 27e (52.9%) | 6 (60%) | 21 (51.2%) |
| Clinical course | |||
| Hospitalization period (days) | |||
| Mean (max–min) | 34.3 (180–1) | 44 (180–1) | 32 (120–6) |
| Number of audiometric tests | 38 | 4 | 34 |
| Hearing status | |||
| Significant Hearing Loss | 34 (89.5%) | 1 (2.9%) | 33 (97%) |
| Bilateral Hearing Loss | 10 (26.3%) | 1 (10%) | 9 (90%) |
| Permanent sequelae | |||
| Number of patients | 15 (29.4%) | 4 (26.7%) | 11f (73.3%) |
| Facial nerve palsy | 7 (13.7%) | 0 (0%) | 8 (100%) |
| Abducens nerve palsy | 5 (9.8%) | 2 (40%) | 3 (60%) |
| Other neurological sequelaeg | 7 (13.7%) | 2 (28.6%) | 5 (71.4%) |
| Deaths | |||
| n | 4 (7.8%) | 1 (25%) | 3 (75%) |
Otologic procedures for AOM cases: 3 patients underwent myringotomy; 1 underwent tympanomastoidectomy.
Otological procedures for COM cases: 36 patients had canal wall down mastoidectomy and 3 patients had canal wall up tympanomastoidectomy; only 2 patients with COM were too sick and died before any otological surgical intervention could be performed.
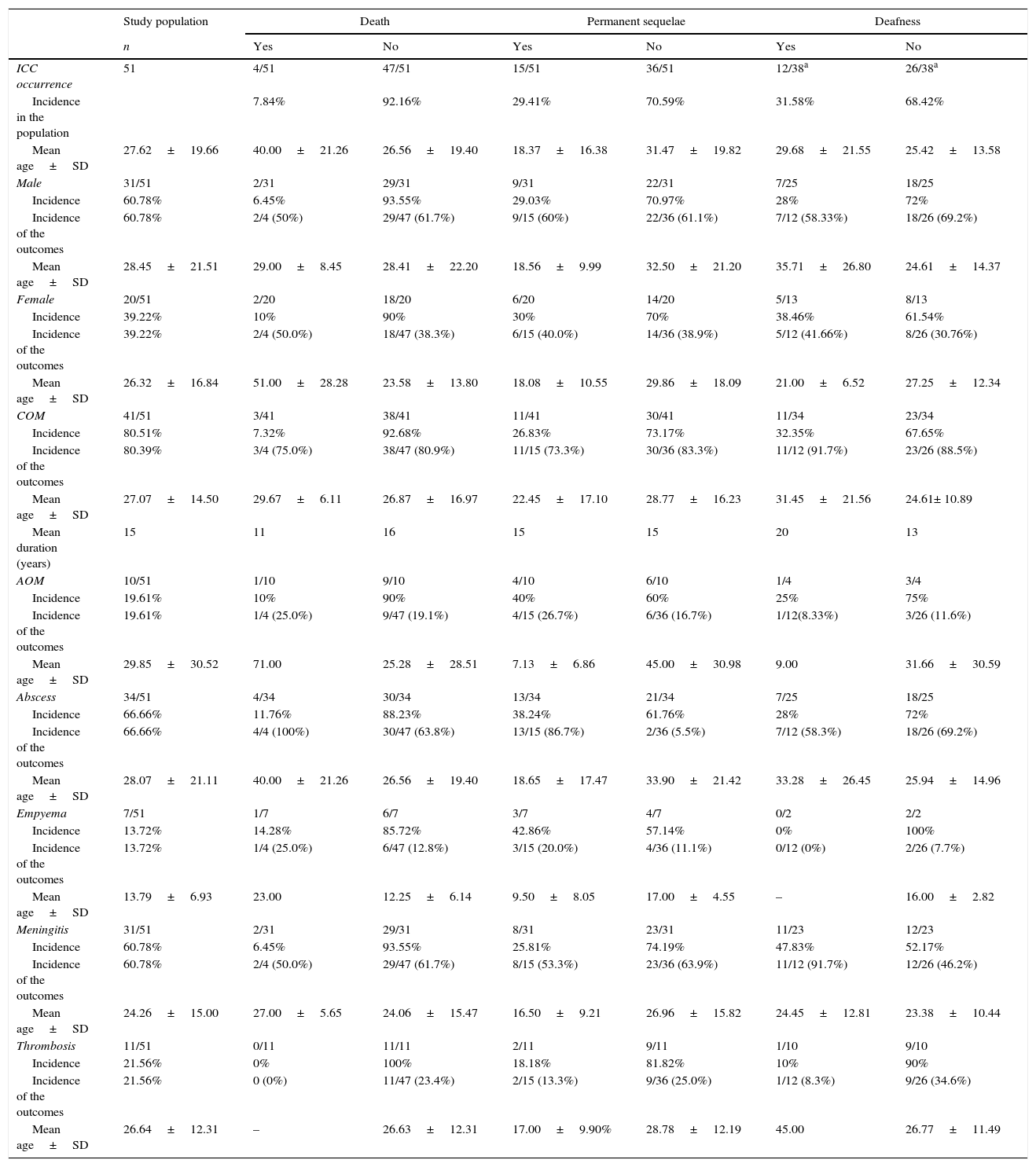
Incidence of the outcomes of death, permanent sequelae, and deafness in relation to age, gender, diagnosis of otitis and major intracranial complications.
| Study population | Death | Permanent sequelae | Deafness | ||||
|---|---|---|---|---|---|---|---|
| n | Yes | No | Yes | No | Yes | No | |
| ICC occurrence | 51 | 4/51 | 47/51 | 15/51 | 36/51 | 12/38a | 26/38a |
| Incidence in the population | 7.84% | 92.16% | 29.41% | 70.59% | 31.58% | 68.42% | |
| Mean age±SD | 27.62±19.66 | 40.00±21.26 | 26.56±19.40 | 18.37±16.38 | 31.47±19.82 | 29.68±21.55 | 25.42±13.58 |
| Male | 31/51 | 2/31 | 29/31 | 9/31 | 22/31 | 7/25 | 18/25 |
| Incidence | 60.78% | 6.45% | 93.55% | 29.03% | 70.97% | 28% | 72% |
| Incidence of the outcomes | 60.78% | 2/4 (50%) | 29/47 (61.7%) | 9/15 (60%) | 22/36 (61.1%) | 7/12 (58.33%) | 18/26 (69.2%) |
| Mean age±SD | 28.45±21.51 | 29.00±8.45 | 28.41±22.20 | 18.56±9.99 | 32.50±21.20 | 35.71±26.80 | 24.61±14.37 |
| Female | 20/51 | 2/20 | 18/20 | 6/20 | 14/20 | 5/13 | 8/13 |
| Incidence | 39.22% | 10% | 90% | 30% | 70% | 38.46% | 61.54% |
| Incidence of the outcomes | 39.22% | 2/4 (50.0%) | 18/47 (38.3%) | 6/15 (40.0%) | 14/36 (38.9%) | 5/12 (41.66%) | 8/26 (30.76%) |
| Mean age±SD | 26.32±16.84 | 51.00±28.28 | 23.58±13.80 | 18.08±10.55 | 29.86±18.09 | 21.00±6.52 | 27.25±12.34 |
| COM | 41/51 | 3/41 | 38/41 | 11/41 | 30/41 | 11/34 | 23/34 |
| Incidence | 80.51% | 7.32% | 92.68% | 26.83% | 73.17% | 32.35% | 67.65% |
| Incidence of the outcomes | 80.39% | 3/4 (75.0%) | 38/47 (80.9%) | 11/15 (73.3%) | 30/36 (83.3%) | 11/12 (91.7%) | 23/26 (88.5%) |
| Mean age±SD | 27.07±14.50 | 29.67±6.11 | 26.87±16.97 | 22.45±17.10 | 28.77±16.23 | 31.45±21.56 | 24.61± 10.89 |
| Mean duration (years) | 15 | 11 | 16 | 15 | 15 | 20 | 13 |
| AOM | 10/51 | 1/10 | 9/10 | 4/10 | 6/10 | 1/4 | 3/4 |
| Incidence | 19.61% | 10% | 90% | 40% | 60% | 25% | 75% |
| Incidence of the outcomes | 19.61% | 1/4 (25.0%) | 9/47 (19.1%) | 4/15 (26.7%) | 6/36 (16.7%) | 1/12(8.33%) | 3/26 (11.6%) |
| Mean age±SD | 29.85±30.52 | 71.00 | 25.28±28.51 | 7.13±6.86 | 45.00±30.98 | 9.00 | 31.66±30.59 |
| Abscess | 34/51 | 4/34 | 30/34 | 13/34 | 21/34 | 7/25 | 18/25 |
| Incidence | 66.66% | 11.76% | 88.23% | 38.24% | 61.76% | 28% | 72% |
| Incidence of the outcomes | 66.66% | 4/4 (100%) | 30/47 (63.8%) | 13/15 (86.7%) | 2/36 (5.5%) | 7/12 (58.3%) | 18/26 (69.2%) |
| Mean age±SD | 28.07±21.11 | 40.00±21.26 | 26.56±19.40 | 18.65±17.47 | 33.90±21.42 | 33.28±26.45 | 25.94±14.96 |
| Empyema | 7/51 | 1/7 | 6/7 | 3/7 | 4/7 | 0/2 | 2/2 |
| Incidence | 13.72% | 14.28% | 85.72% | 42.86% | 57.14% | 0% | 100% |
| Incidence of the outcomes | 13.72% | 1/4 (25.0%) | 6/47 (12.8%) | 3/15 (20.0%) | 4/36 (11.1%) | 0/12 (0%) | 2/26 (7.7%) |
| Mean age±SD | 13.79±6.93 | 23.00 | 12.25±6.14 | 9.50±8.05 | 17.00±4.55 | – | 16.00±2.82 |
| Meningitis | 31/51 | 2/31 | 29/31 | 8/31 | 23/31 | 11/23 | 12/23 |
| Incidence | 60.78% | 6.45% | 93.55% | 25.81% | 74.19% | 47.83% | 52.17% |
| Incidence of the outcomes | 60.78% | 2/4 (50.0%) | 29/47 (61.7%) | 8/15 (53.3%) | 23/36 (63.9%) | 11/12 (91.7%) | 12/26 (46.2%) |
| Mean age±SD | 24.26±15.00 | 27.00±5.65 | 24.06±15.47 | 16.50±9.21 | 26.96±15.82 | 24.45±12.81 | 23.38±10.44 |
| Thrombosis | 11/51 | 0/11 | 11/11 | 2/11 | 9/11 | 1/10 | 9/10 |
| Incidence | 21.56% | 0% | 100% | 18.18% | 81.82% | 10% | 90% |
| Incidence of the outcomes | 21.56% | 0 (0%) | 11/47 (23.4%) | 2/15 (13.3%) | 9/36 (25.0%) | 1/12 (8.3%) | 9/26 (34.6%) |
| Mean age±SD | 26.64±12.31 | – | 26.63±12.31 | 17.00±9.90% | 28.78±12.19 | 45.00 | 26.77±11.49 |
n, number; ICC, intracranial complications; SD, standard deviation; COM, chronic otitis media; AOM, acute otitis media; Permanent sequelae, neurological sequelae, VI, VII nerve paralysis.
Statistical analysis of risk factors for death, permanent sequelae and deafness.
| Death | Permanent sequelae | Deafness | |
|---|---|---|---|
| RR | 0.65 | 0.97 | 0.73 |
| Male | |||
| Y | –0.23 | –0.02 | –0.23 |
| X2 | 0.21 | 0.01 | 0.43 |
| SIG | No | No | No |
| RR | 1.55 | 1.03 | 1.37 |
| Female | |||
| Y | 0.23 | 0.02 | 0.23 |
| X2 | 0.21 | 0.01 | 0.43 |
| SIG | No | No | No |
| RR | 0.73 | 0.67 | 1.29 |
| Chronic otitis | |||
| Y | –0.17 | –0.29 | 0.18 |
| X2 | 0.08 | 0.67 | 0.09 |
| SIG | No | No | No |
| RR | 1.37 | 1.49 | 0.77 |
| Acute otitis | |||
| Y | 0.17 | 0.29 | –0.18 |
| X2 | 0.08 | 0.67 | 0.09 |
| SIG | No | No | No |
| RR | a | 3.25 | 0.73 |
| Abscess | |||
| Y | 1.00 | 0.65 | –0.23 |
| X2 | 2.17 | 3.83 | 0.43 |
| SIG | No | Nob | No |
| RR | 2.10 | 1.57 | 0.00 |
| Empyema | |||
| Y | 0.39 | 0.33 | –1.00 |
| X2 | 0.47 | 0.71 | 0.97 |
| SIG | No | No | No |
| RR | 0.65 | 0.74 | 7.17 |
| Meningitis | |||
| Y | –0.23 | –0.22 | 0.86 |
| X2 | 0.21 | 0.49 | 7.12 |
| SIG | No | No | Yesc |
| RR | 0.00 | 0.56 | 0.22 |
| Thrombosis | |||
| Y | –1.00 | –0.37 | –0.75 |
| X2 | 1.19 | 0.85 | 3.62 |
| SIG | No | No | No |
RR, relative risk; Y, Yule association coefficient; X2, X2 test of association of Pearson; SIG, X2 test of significance associated with Pearson's 1 degree of freedom and alpha of 5% (critical value 3.84).
ICC from OM is seen predominantly in male children and young adults, which agrees with other reports in the literature.31–34 CCOM is responsible for over 76% of cases of ICCs. AOM-related ICCs occur mostly below age 15, which corresponds with the highest occurrence of AOM. It is customary to think about AOM as a childhood problem; however, one cannot overlook the second “bump” of AOM in the geriatric population. This bimodal distribution of incidence skews the average age of patients with ICC from AOM misleadingly higher.
ICCs associated with COM occur predominantly between 10 and 39 years of age. Assuming the “age of onset” of COM is approximately 11 years old and the “duration of the disease” is approximately 15 years, we can postulate that indolent pediatric cases of COM, which were not properly diagnosed, treated or followed, would become more aggressive disease that would culminate with intracranial complications during adolescence and early adulthood. COM, in particular CCOM, was the most common etiology in this report, a result that is similar to reports by other authors from other developing countries. In contrast, a different scenario has been observed in developed countries, such as Finland, where AOM accounts for more than 80% of the complications, and COM and CCOM are responsible for only 12% and 8% of complications, respectively.
With the progress achieved through collective action and public health, the mortality rate from infectious diseases has been decreasing in most of the world. In the mid-twentieth century, it was even thought that the eradication of infectious diseases would be achieved imminently;35 however, this prediction failed to materialize, even in countries currently considered highly developed. In fact, what occurred in many places was a change in the pattern of infectious diseases.36 At the present time, although otitis media has a benign course and typically responds well to treatment overall, some cases (both AOM and COM) develop severe and lethal complications with considerable mortality rates ranging from 8% to 18.6%.
Accurate examination with early diagnosis and intervention in cases of COM, before a complication has already developed, is very important in prevention of delayed ICC. Nonetheless, although there have been significant advances in the diagnosis and treatment resources available in medical practice, as well as undeniable socioeconomic improvements in Brazil over the last two decades, we observed a stable occurrence of ICCs over time.
Hearing loss due to OM is a worldwide public health issue. Our data confirm a high prevalence of significant hearing loss and deafness in cases of COM. The inflammatory and infectious events that take place in OM cases are still undervalued in this regard. Additionally, our data confirm that patients with ICCs due to OM have high hospital costs, permanent neurological sequelae in 29%, and a mortality rate of 7.8%, seen in the young and economically active. According to the Brazilian statewide system of data analysis (www.seade.gov.br), there was a total of 6701 admissions to the Brazilian public health system in the state of Sao Paulo related to “diseases of the ear and mastoid process” which cost R$ 2.5 million and resulted in 30 reported deaths in one year. Due to its prevalence and high socioeconomic cost, OM remains a pressing public health issue. Education and training of PCPs is essential for early identification of uncomplicated ear disease, as early and appropriate treatment may prevent the development of more aggressive OM and avoid the ICCs due to OM.
Once the complication has occurred, a multidisciplinary approach is required to maximize recovery. Currently, it is common that when there is a sick patient with a temporal lobe or cerebellar abscess, the possibility of concomitant OM is often overlooked. However, because the primary infection responsible is often not immediately diagnosed, the time of hospitalization and chances of sequelae are increased.
Neurosurgical drainage of the intracranial abscess, without removing the causative cholesteatoma, is directly related to relapse. In these cases, it is mandatory to surgically extirpate the ear infection because it is the focus of continued contamination of the central nervous system. Mastoidectomy should be performed as early as possible and during the same hospitalization. The abscess is frequently able to be drained into the ear.
ConclusionLife-threatening intracranial complications from otitis media still occur. Complications in cases of acute otitis media usually occur in children or in the elderly. In contrast, complications of chronic otitis media are generally observed in young adulthood, particularly cases of cholesteatoma that begin in childhood and take several years to develop. Patients with intracranial complications remain hospitalized for a long period of time, and these individuals have significant morbidity from permanent auditory and neurological sequelae, as well as a substantial mortality rate. We have shown that the high incidence of OM, the inaccuracies in diagnosis, and the possibility of life threatening sequelae make this an important ongoing problem. As such, the primary treating physician must maintain a high index of suspicion when examining a patient with OM.
Conflicts of interestSujana S. Chandrasekhar, MD – shareholder and board member, Scientific Development and Research, Inc. (Intranasal Surfactant Research). Other authors: none.
Please cite this article as: Penido NO, Chandrasekhar SS, Borin A, Maranhão ASA, Testa JRG. Complications of otitis media – a potentially lethal problem still present. Braz J Otorhinolaryngol. 2016;82:253–62.