Primary thyroid lymphoma is a relatively rare disease of the thyroid gland. PTL represents approximately 1%–5% of thyroid malignancies and less than 2% of extra nodal lymphomas: the prognosis is generally good.1 Thyroid lymphomas are more common in women with a predominance of 3–4:1.2
The main clinical manifestation is a rapidly enlarging thyroid mass, commonly in the seventh decade. Approximately 30%–50% of patients manifest compression symptoms of the adjacent structures, in addition to dysphagia, stridor, hoarseness, cough and a pressure sensation in the neck. Symptoms such as fever, night sweats and weight loss are less common. Hashimoto's thyroiditis appears to be a risk factor for thyroid lymphoma although the association is still debated.1,2
The most common histopathological type of thyroid lymphomas is non-Hodgkin's lymphoma with B cell origin. Hodgkin's diseases and T-cell lymphomas are rare tumors. Patients with pure mucosa associated lymphoid tissue (MALT) lymphomas tend to demonstrate a more indolent course and a better prognosis compared with patients with diffuse large B-cell types or mixed histological subtypes, which may have a more aggressive clinical course.3
A general 5-year survival rate for PTL is approximately 90%; therefore a well-planned treatment after rapid and accurate diagnosis generally results in good prognosis.4
Case reportA 52-year-old-woman was admitted to the otorhinolaryngology service because of a two-month history of hoarseness and left otalgia. No breathing or swallowing complaints were present. Prior to admission to our clinic, medical treatment had been provided for her twice for laryngitis, but her complaints did not improve.
She reported a history of diabetes mellitus, hypertension and hypothyroidism (chronic lymphocytic thyroiditis) and also cholecystectomy.
On physical examination, the left vocal cord was fixed in the midline and fullness on left false vocal cord could be observed. The thyroid lobes demonstrated nodules bilaterally and were enlarged, with the left lobe being slightly firmer and larger than the right. There were no cervical palpable masses or lymphadenopathy.
Thyroid function tests were within normal range although she was using thyroid hormones for hypothyroidism. Thyroid biopsy had been performed 2 years previously and the histopathologic report revealed a chronic lymphocytic thyroiditis.
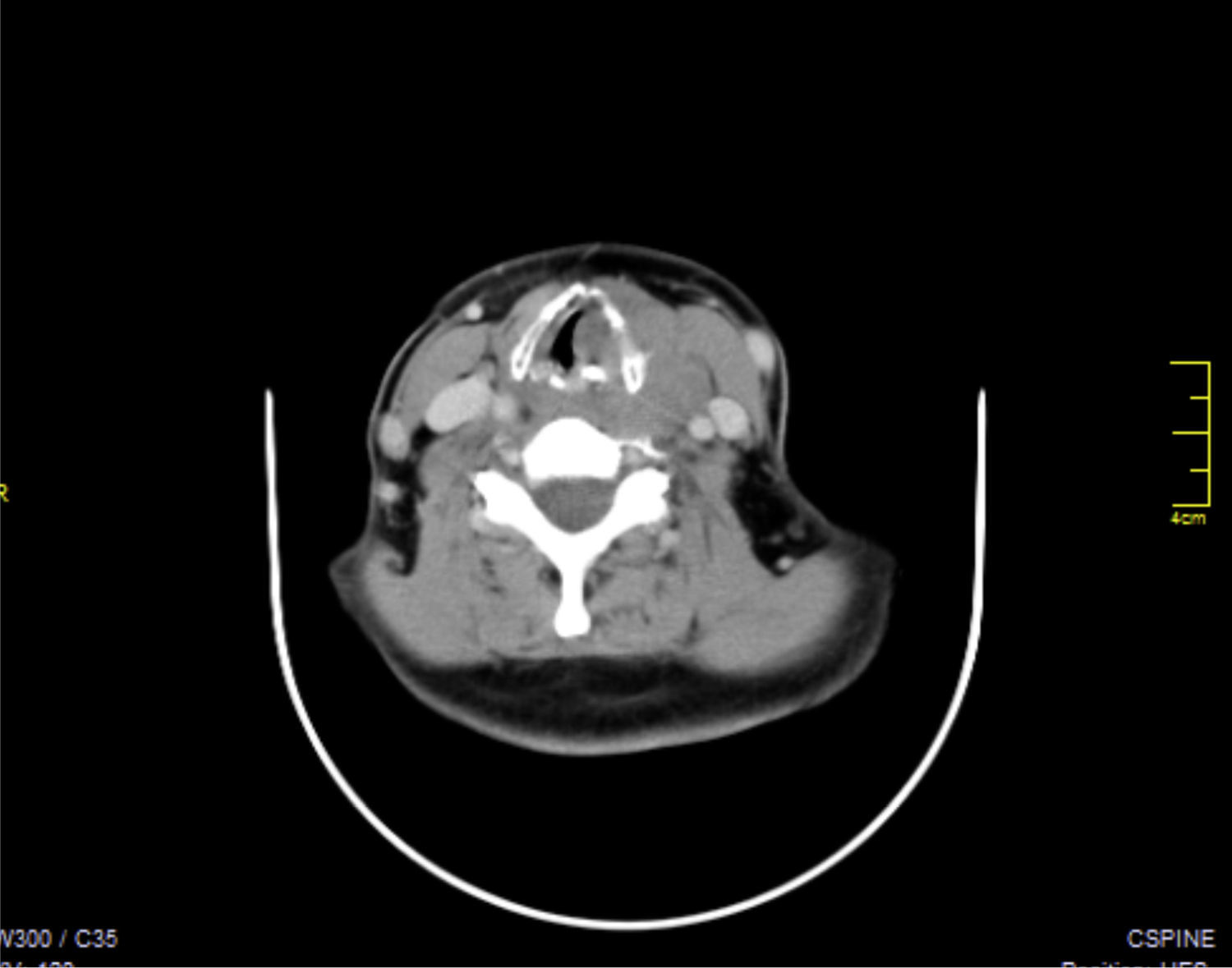
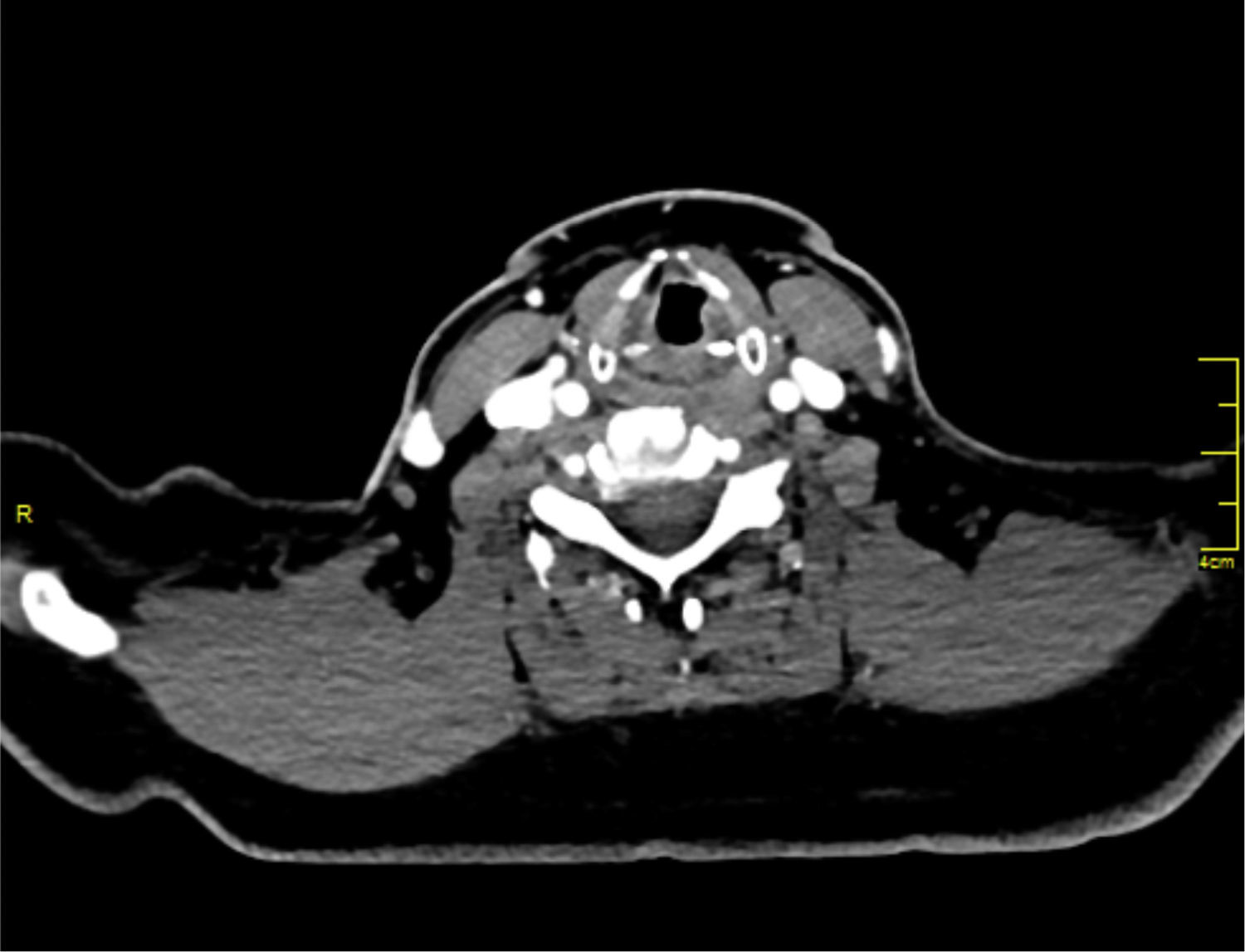
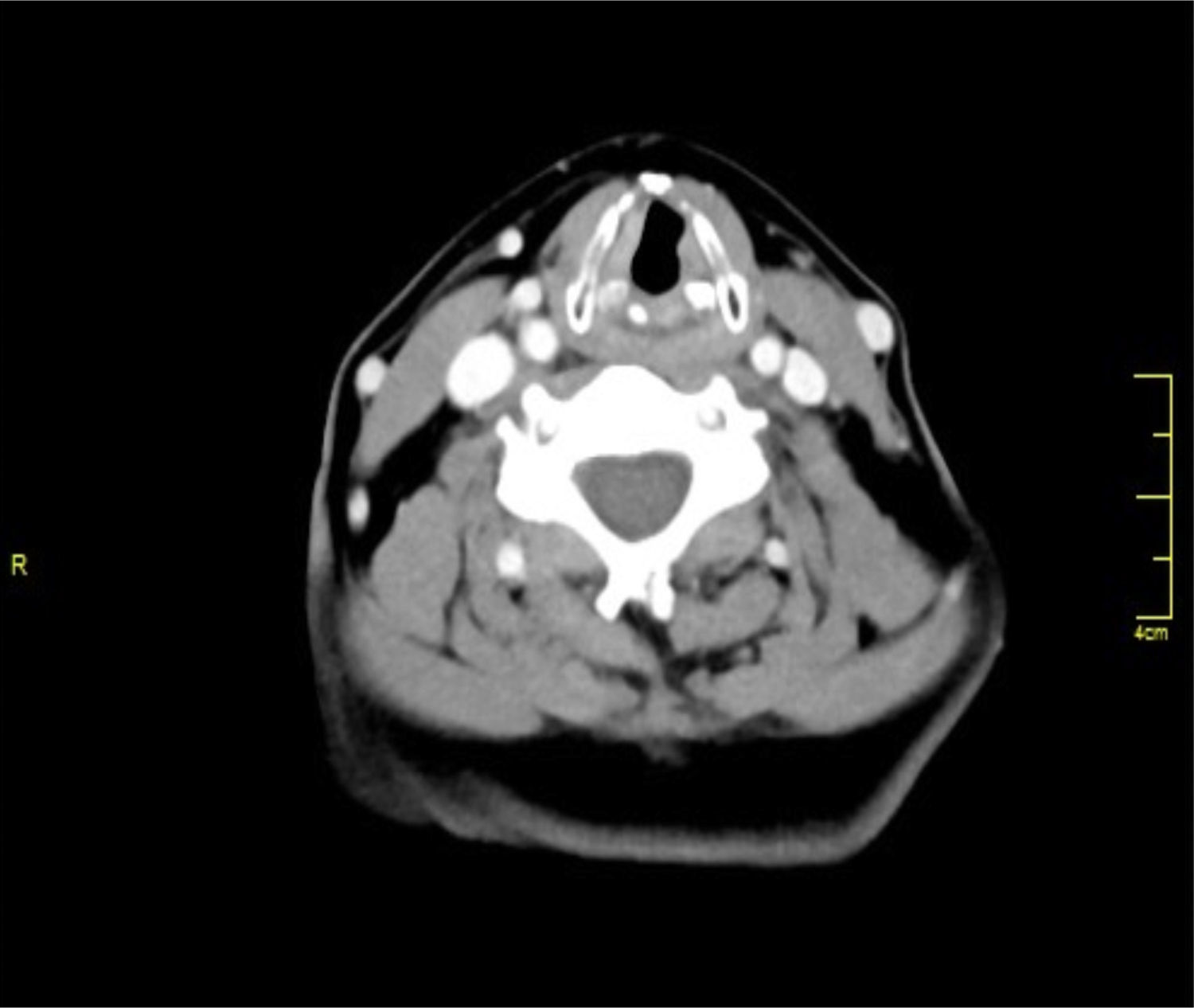
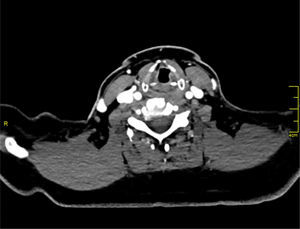
On radiologic evaluation masses in the left false vocal cord eroding the left thyroid cartilage, continuous with the thyroid gland, were observed. There were nodules in both thyroid lobes (Fig. 1).
A laryngeal pathology originating from the left laryngeal structures that eroded thyroid cartilage and extended to the thyroid gland was considered after examination. A direct laryngoscopy and biopsy procedure from both left laryngeal ventricles and a fine needle thyroid biopsy from nodules of both thyroid lobes was planned.
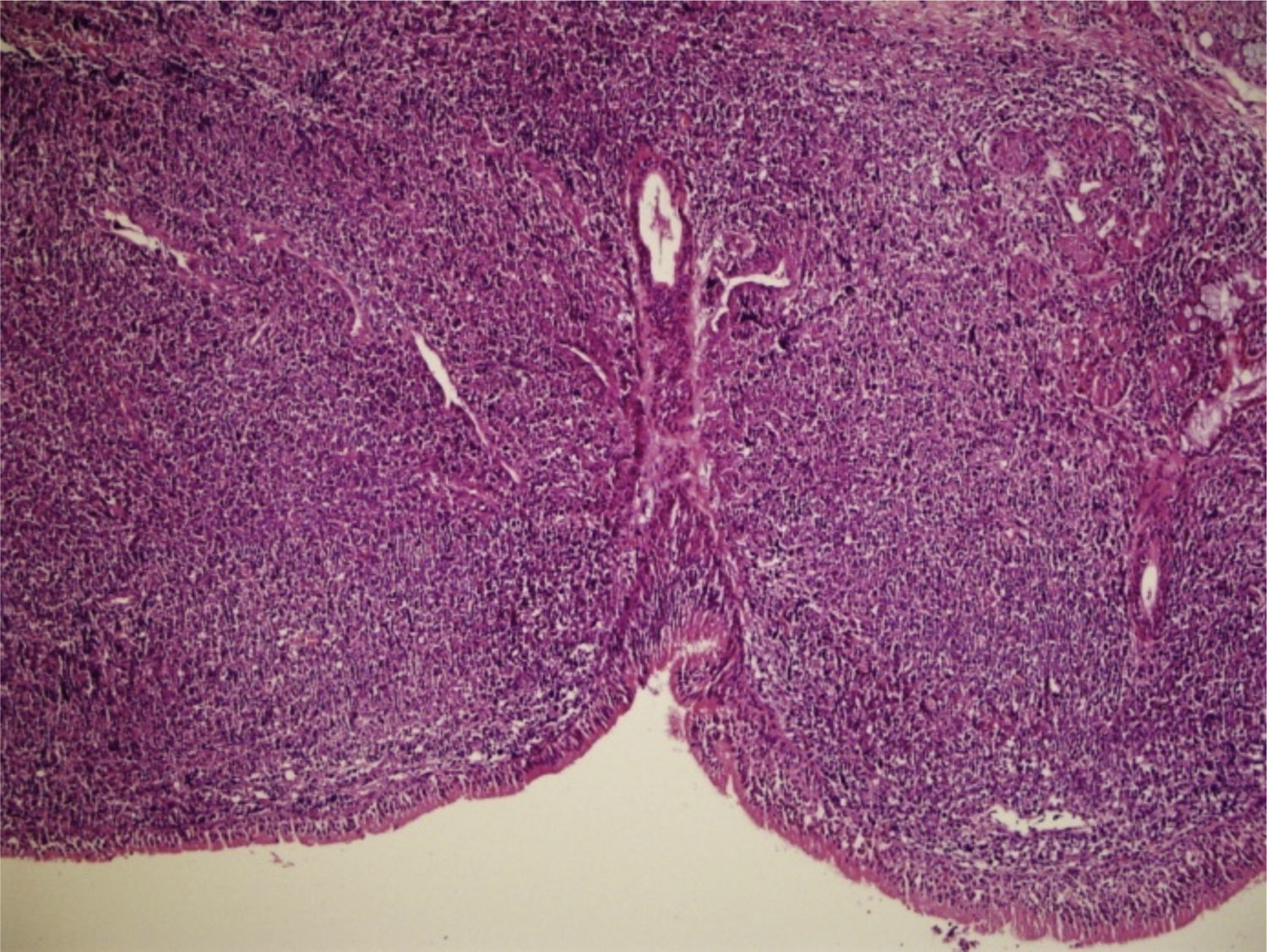
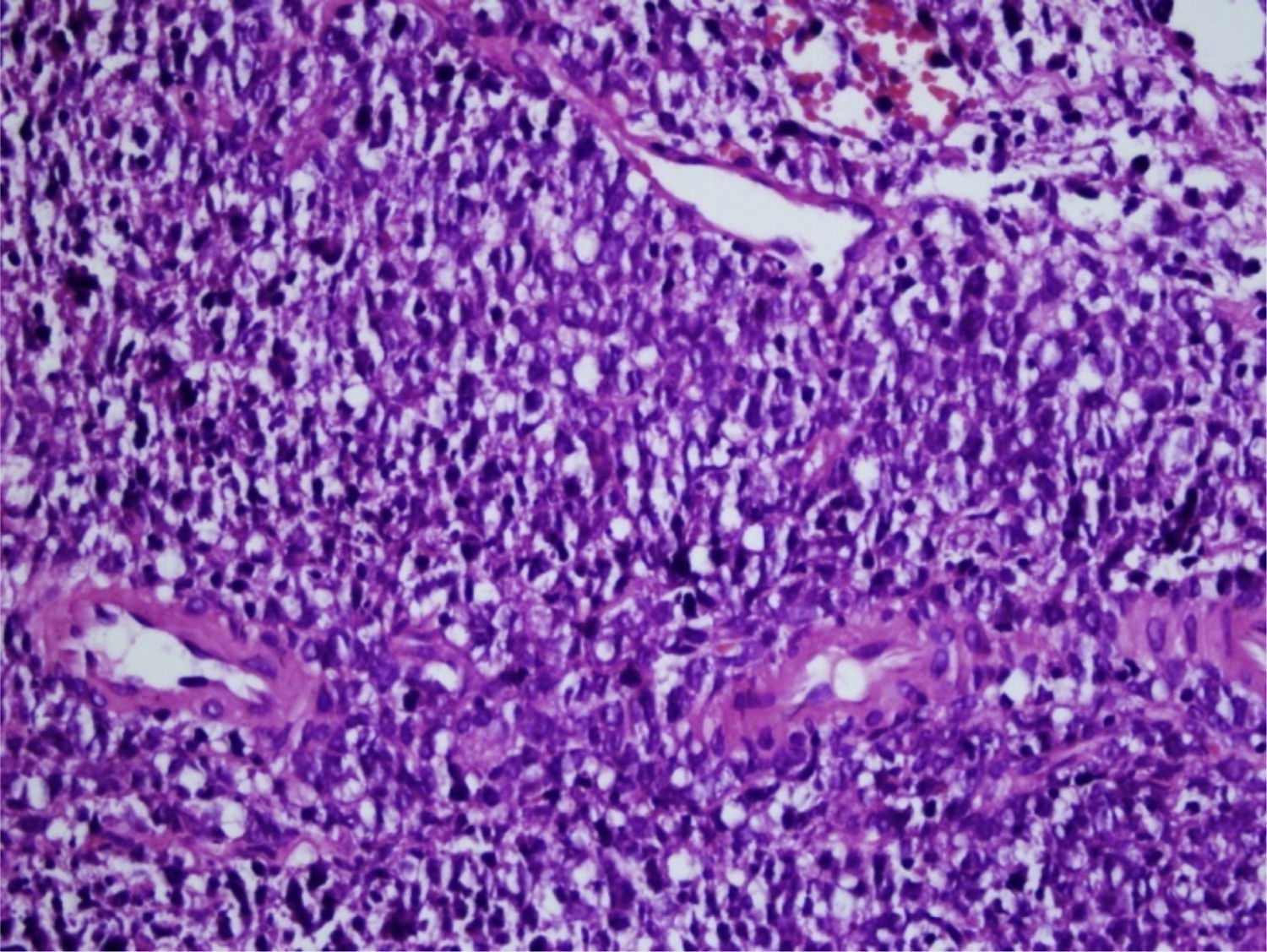
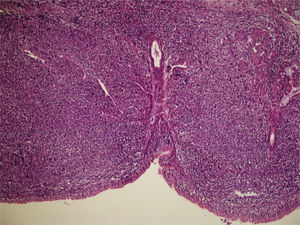
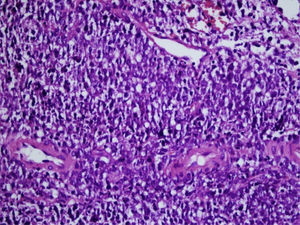
Biopsy of the left false vocal cord was reported as diffuse large B cell lymphoma. Fine needle aspiration from both thyroid lobes was reported as atypical lymphocytes (Figs. 2 and 3). The prognostic factors of lymphoma were diagnosed as follows: proliferative index of Ki 67 was 80%–90%, LDH (lactate dehydrogenase) and sedimentation was normal. The patient reported weight loss of 20kg in the last 4 months. International prognostic index (IPI) score was found as 0.
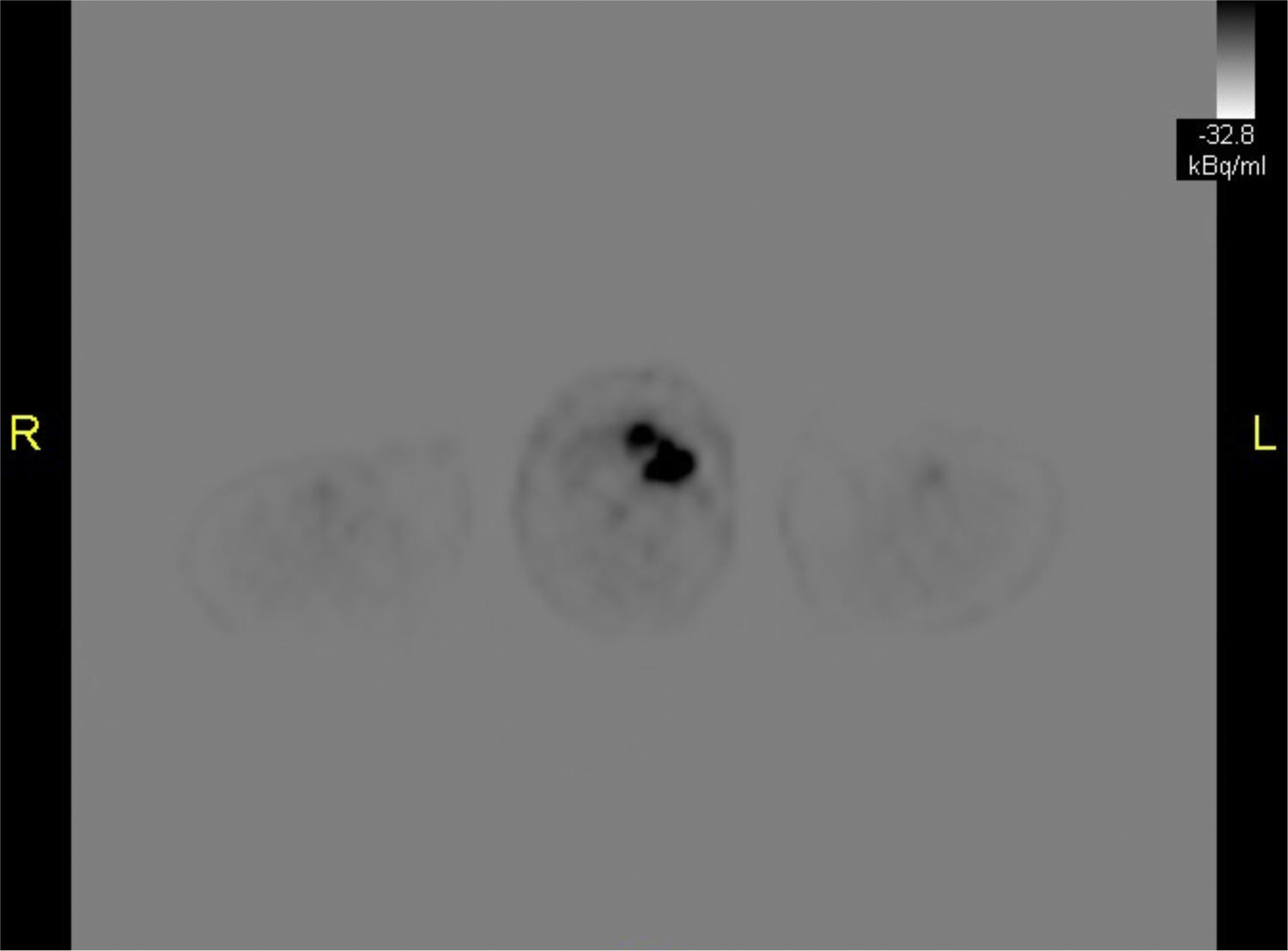
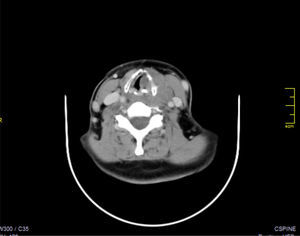
A fludeoxy glucose-positron emission tomography (FDG-PET) scan for differentiating the lesion between primary thyroid lymphoma or thyroid involvement of a systemic disease showed only diffuse involvement in left thyroid lobe (Fig. 4).
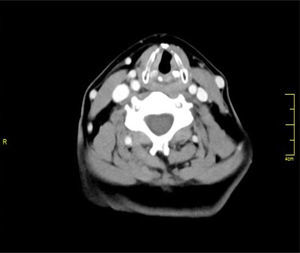
As a result of these diagnostic tests patient was diagnosed as diffuse large B cell primary thyroid lymphoma, stage 1E. She received 3 courses of R-CHOP (rituximab–cyclophosphamide, doxorubicin, vincristine and prednisolone) treatment and involved-field radiation therapy following chemotherapy. Her treatment course was uneventful and her hoarseness improved after treatment (Fig. 5).
A team including oncology, radiation oncology, otorhinolaryngology, endocrinology departments followed the patient every month after chemoradiation treatment. She continues thyroid replacement treatment. Her thyroid is now grade 3 palpable in diffuse and hard pattern. There cannot be identified any nodular pattern in examination. Both vocal cords are mobile and there is no visible pathologic finding in laryngeal evaluation.
Six months after chemoradiation therapy the patient is now in a good health without any complaint. Her physical, laboratory, laryngeal and radiologic evaluation is completely normal without any evidence of relapse (Fig. 6).
DiscussionExtranodal lymphomas are usually seen as non-Hodgkin's lymphoma (NHL) which constitute 10%–29% of all lymphomas. Adult NHLs commonly arise from B cells. The main clinical symptom is an enlarging mass in head and neck region, which may also manifest a destructive clinical progress.
Extranodal marginal zone B-cell lymphoma of MALT type may occur in the stomach, orbit, intestine, lung, thyroid, salivary gland, skin, soft tissues, bladder, kidney and central nervous system. The most common extranodal extralymphatic sites are the paranasal sinuses, the salivary glands and the thyroid gland.4
The larynx is a rare site for localization of a primary NHL because of relatively low lymphoid content. In the literature, there are fewer than 100 cases of lymphoproliferative tumors arising from the larynx (including both NHL and immunosuppression-related lymphoproliferative diseases) and few cases of laryngeal infiltration of PTL have been reported. There is no reported case of PTL presenting with hoarseness and diagnosed through direct laryngoscopic biopsy, since it typically does not erode thyroid cartilage.
Primary or secondary laryngeal pathologies may manifest similar symptoms including dysphonia, hoarseness, dysphagia: a cervical mass can be found. A smooth submucosal swelling or polypoid mass without ulceration are the usual physical examination findings of primary laryngeal lymphomas. Primary laryngeal lymphomas usually arise from the supraglottic region, specifically from the epiglottis and aryepiglottic folds.5 Our case also demonstrates supraglottic infiltration especially in left laryngeal ventricule. Extralaryngeal tumor extension is most frequently noted to involve the hypopharynx, and less commonly the oropharynx and strap muscles.
PTL is a lymphamatous process which develops in the thyroid without involvement of primary lymphoid organs or distant metastasis at the time of diagnosis. PTL comprises 2%–8% of thyroid malignancies. It is mostly seen in a middle-aged elderly women with a median age of 56 years. Patients usually have a history of hypothyroidism or thyroiditis and mass in thyroid gland which can rapidly grow. Dyspnea, stridor, dysphagia, and hoarseness are common symptoms in patients with thyroid lymphoma, while main finding may only be an enlarging cervical mass which presents in over 87% of patients. However PTL may suddenly grow and compromise the airway.
The majority of PTLs are high grade while only 30% are low-grade. Early diagnosis and appropriate treatment of thyroid lymphomas can provide long time survival.3
Anaplastic thyroid cancers (ATC) also present with a rapidly growing large mass in elderly patients. Anaplastic thyroid cancers, which compromise 1%–2% of thyroid malignancies, have similar clinical progress and must be included in the differential diagnosis of thyroid lymphomas. ATC's may rapidly progress and compromise the air way with an average mean survival of 6–7 months. On radiologic evaluation ATC is presents as a large, solid mass accompanied by necrosis, hemorrhage, dense calcification, direct invasion of adjacent structures and cervical lymph node metastasis. Tumor necrosis has been known to be one of the most valuable parameters in differentiating ATC from other thyroid masses, and low attenuation value on post contrast scan (attenuation value<100HU) is another predictor of anaplastic carninoma.6
Benign or malignant thyroid nodules generally grow slowly which can be less than 1cm over 38 months. Compression symptoms due to acute enlargement of thyroid nodules are very rare and may result in life-threatening complications like acute respiratory compromise. Spontaneous hemorrhage in a thyroid nodule or a malignant process such as ATC or lymphomas may result in acute enlargement.
PTL patients mostly have the history of autoimmune thyroiditis; PTL development process takes an average of 20–30 years to develop after the onset of lymphocytic thyroiditis.7
Fine needle aspiration with or without ultrasonography is the first step in diagnostic strategy for a thyroid nodule, but accuracy is quite low in thyroid lymphoma or anaplastic cancer. The diagnostic approaches for an enlarging thyroid mass are FNA, core needle biopsy (CNB), open biopsy, and/or surgical intervention. The diagnostic effect of FNA identifies 30%–80% of thyroid lymphoma patients; therefore further diagnostic approaches may be useful when FNA is inconclusive.8 Core needle biopsy (CNB) generally provides enough tissue needed for the certain diagnosis of aggressive thyroid cancers like lymphoma or ATC. Therefore CNB may be the first diagnostic step when a large aggressive thyroid mass is encountered on radiologic evaluation.
Histological and phenotypic analyses such as flow cytology or immunohistochemistry are very helpful in pathological evaluation. Most thyroid lymphomas are B-cell origin with diffuse large-cell type.
Most patients present with early stages IE (30%–66%) or stage IIE (25%–66%) disease.9 For staging, CT scans of head, neck, chest, abdomen and pelvis or FDG-PET scan should be performed.
Treatment options consist of chemotherapy alone, radiation therapy alone and combined chemo-radiation therapy. Although there are some articles that advise thyroidectomy followed by radiation therapy, the series reported are too small to accept as widespread use as a treatment option.
The overall relapse rates are 7.7%, 37.1% and 43% for chemoradiation therapy, radiation therapy alone, and chemotherapy alone respectively. Local relapse rates are 2.6%, 12.6% and 23% for chemoradiation therapy, radiation therapy alone, and chemotherapy alone respectively.1
The most common chemotherapy regimen is R-CHOP (rituximab–cyclophosphamide, doxorubicin, vincristine and prednisolone). The biologic agent rituximab, a monoclonal antibody directed against B-cell-specific antigen CD 20 is generally used with CHOP chemotherapy in the treatment of thyroid lymphoma.
Radiotherapy is generally chosen after 3–6 CHOP courses in the form of modified mantle irradiation, including thyroid, bilateral neck, supraclavicular area and mediastinum.
Age (>60 years), elevated levels of serum lactate dehydrogenase (LDH), and β2 macroglobulin, extra nodal site involvement and stage III–IV classification are poor prognostic factors.10
Our patient received R-CHOP based chemotherapy and radiotherapy and is alive without any sign of disease.
ConclusionThe present report details the first known case diagnosed with thyroid lymphoma through direct laryngoscopy and biopsy.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Gökdoğan O, Koybasioglu A, Ismail E, Erol T, Alagoz G, Yagmurlu B, et al. Hoarseness: an unusual presentation of primary thyroid lymphoma with laryngeal infiltration. Braz J Otorhinolaryngol. 2016;82:737–40.