Sudden deafness is characterized by an abrupt hearing loss of at least 30dB in three sequential frequencies in the standard pure tone audiogram over three days or less. Treatment is based on its etiology, and oral corticosteroids are widely used. Intratympanic corticosteroids are included as primary or secondary treatment when there is no improvement with the use of oral corticosteroids.
ObjectiveTo determine the effectiveness of therapy with intratympanic steroids in sudden deafness.
MethodsA systematic review was performed of publications on the topic in the databases of PubMed/MEDLINE, with the keywords: sudden deafness, sudden hearing loss, and corticosteroids.
ResultsThirty scientific studies were analyzed. As to the objectives of the study analyzed, 76.7% sought to evaluate the use of intratympanic therapy salvage after failure to conventional treatment, and intratympanic therapy was used as the primary treatment 23.3% of the studies.
ConclusionIntratympanic corticosteroid therapy is prescribed primarily when there is failure of conventional therapy and when it is limited to use systemic corticosteroids, such as the diabetic patient.
A surdez súbita é caracterizada por uma perda abrupta da audição de pelo menos 30dB em três frequências sequenciadas no audiograma tonal de rotina ao longo de três dias, ou menos. O tratamento é fundamentado em sua etiologia e corticosteroides orais são amplamente utilizados. A terapia com corticosteroide intratimpânico foi incluída como tratamento primário ou secundário nos casos em que não houve melhora com o uso de corticosteroides orais.
ObjetivoDeterminar a eficácia da terapia intratimpânica com esteroides em casos de surdez súbita.
MétodoFoi realizada uma revisão sistemática das publicações sobre o tópico no banco de dados Pubmed/Medline, com as palavras-chave: surdez súbita, perda súbita da audição e corticosteroides.
ResultadosForam analisados 30 estudos científicos. Com relação aos objetivos dos estudos analisados, 76,7% procuravam avaliar o uso da terapia intratimpânica em seguida ao insucesso com o tratamento convencional; a terapia intratimpânica foi empregada como tratamento primário em 23,3% dos estudos.
ConclusãoA terapia com corticosteroide intratimpânico é prescrita primariamente nos casos de insucesso com a terapia convencional e quando há limitação para o uso de corticosteroides sistêmicos, como ocorre com o paciente diabético.
Sudden hearing loss (SHL) was first described by de Kleyn in 1944 and defined as a hearing loss of at least 30dB in three sequential frequencies in the standard pure tone audiogram over three days or less.1 It may be characterized as an impairment of the inner ear and/or central auditory pathways, with variable intensity and frequency, ranging from mild feeling of ear being clogged to total loss of hearing.2,3
Although it is thought to originate mainly from viral, vascular, or immunologic causes, the etiopathogenesis of the disease is still unknown, so the disease is usually referred to as idiopathic sudden hearing loss (ISHL). It has a reported incidence of 5–20 per 100,000 patients per year, with a mean of 50–60 years and no predominance of sex. In most cases, there is unilateral hearing loss, with bilateral involvement reported in less than 5%.1
Recovery rate in untreated patients ranges from 25% to 50%, mostly resolving within two weeks of onset of symptoms. Although the methods of treatment of SHL patients vary among different centers, systemic steroid (SS) therapy is the most commonly used modality for treatment of sudden hearing loss.2
The treatment of sudden hearing loss is based on its etiology. In idiopathic cases, oral corticosteroids are widely used; intratympanic steroids have been trialed in patients with sudden hearing loss, because they provide a high concentration in the labyrinth in animal models,1 although their results are conflicting.
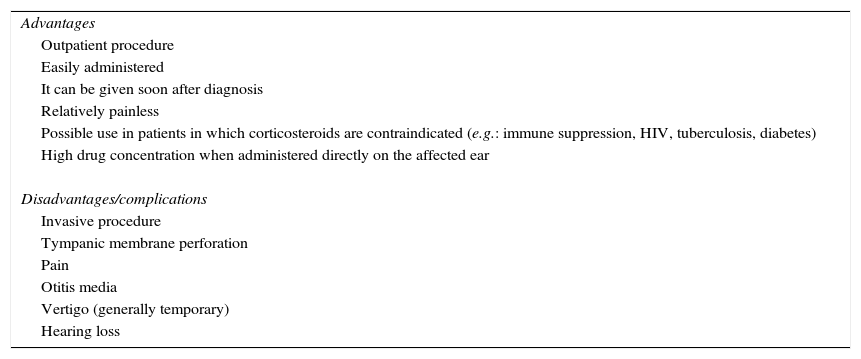
There are several advantages of intratympanic treatment (Table 1): (1) the procedure is well tolerated and relatively easy to perform as an outpatient procedure performed under local anesthesia (topical); (2) general anesthesia can be avoided; (3) most patients understand the concept of intratympanic therapy and easily accept the proposed therapy.4
Advantages of intratympanic treatment.
| Advantages |
| Outpatient procedure |
| Easily administered |
| It can be given soon after diagnosis |
| Relatively painless |
| Possible use in patients in which corticosteroids are contraindicated (e.g.: immune suppression, HIV, tuberculosis, diabetes) |
| High drug concentration when administered directly on the affected ear |
| Disadvantages/complications |
| Invasive procedure |
| Tympanic membrane perforation |
| Pain |
| Otitis media |
| Vertigo (generally temporary) |
| Hearing loss |
Intratympanic steroid has become an attractive alternative, especially in cases when systemic therapy fails, or to avoid the side effects of the systemic use of steroids. However, the standardization of number and frequency of intratympanic treatments and drug delivery methods remain to be determined.5–7
In 2011, Rauch et al. conducted a multicenter, randomized non-inferiority trial comparing oral corticosteroid therapy and intratympanic corticosteroid therapy, and found that the two treatment methods are equally effective.4 These treatments for sudden hearing loss still generate conflicting opinions among otolaryngologists. In certain situations, such as sudden hearing loss in patients with diabetes, intratympanic corticosteroids are recommended as the primary treatment.5
The aim of this study was to present the effectiveness of intratympanic corticosteroid therapy in sudden hearing loss.
MethodsThis was a systematic review that followed the precepts of the Cochrane Handbook as to the formulation of the question, location, selection, and critical evaluation of the articles. The research was based upon the question “should intratympanic corticosteroid therapy be indicated for sudden deafness?” with ‘sudden deafness’ and ‘sudden hearing loss’ associated by the Boolean AND operator to ‘corticosteroids’. All descriptors are contained in the vocabulary and PubMed/MEDLINE using as strategy the descriptor Medical Subject Heading Terms (MeSH).
The type of study and English language were considered as inclusion criteria. Thus, articles written in another language, case studies, and letters to the editor and review articles were excluded.
Abstracts from 149 articles were assessed by two reviewers, who pre-selected for analysis those correlated descriptors focusing on the application of intratympanic corticosteroid in isolation, as rescue therapy, or in combination.
A total of 30 items had tabular data containing the following information: author, origin and year of publication, journal, sample size (n), study design, description of intratympanic corticosteroids and corticosteroid, frequencies analyzed in pure tone audiometry, and results of studies (Tables 2–5).
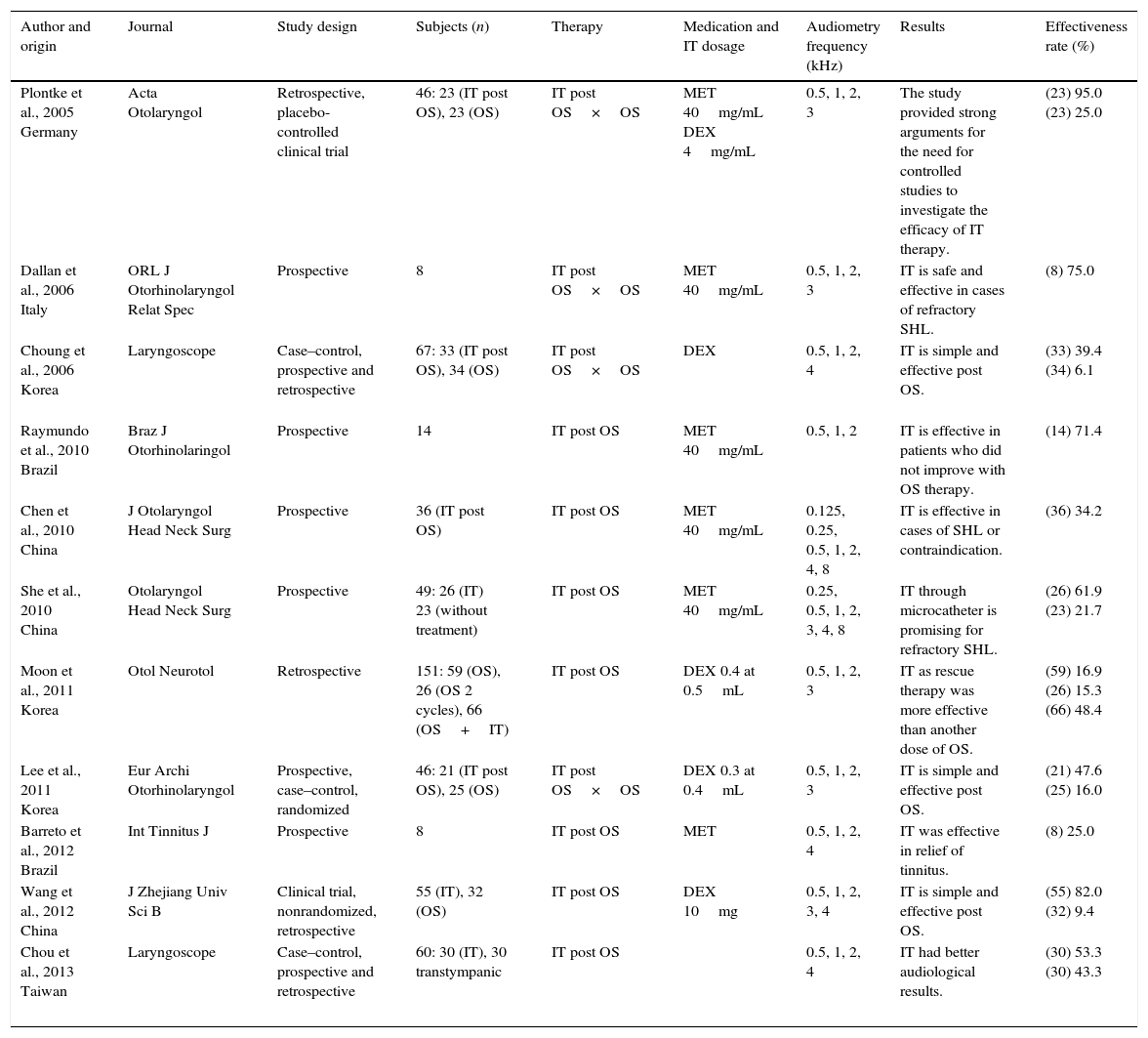
Studies emphasizing salvage therapy failure of oral steroids.
| Author and origin | Journal | Study design | Subjects (n) | Therapy | Medication and IT dosage | Audiometry frequency (kHz) | Results | Effectiveness rate (%) |
|---|---|---|---|---|---|---|---|---|
| Plontke et al., 2005 Germany | Acta Otolaryngol | Retrospective, placebo-controlled clinical trial | 46: 23 (IT post OS), 23 (OS) | IT post OS×OS | MET 40mg/mL DEX 4mg/mL | 0.5, 1, 2, 3 | The study provided strong arguments for the need for controlled studies to investigate the efficacy of IT therapy. | (23) 95.0 (23) 25.0 |
| Dallan et al., 2006 Italy | ORL J Otorhinolaryngol Relat Spec | Prospective | 8 | IT post OS×OS | MET 40mg/mL | 0.5, 1, 2, 3 | IT is safe and effective in cases of refractory SHL. | (8) 75.0 |
| Choung et al., 2006 Korea | Laryngoscope | Case–control, prospective and retrospective | 67: 33 (IT post OS), 34 (OS) | IT post OS×OS | DEX | 0.5, 1, 2, 4 | IT is simple and effective post OS. | (33) 39.4 (34) 6.1 |
| Raymundo et al., 2010 Brazil | Braz J Otorhinolaringol | Prospective | 14 | IT post OS | MET 40mg/mL | 0.5, 1, 2 | IT is effective in patients who did not improve with OS therapy. | (14) 71.4 |
| Chen et al., 2010 China | J Otolaryngol Head Neck Surg | Prospective | 36 (IT post OS) | IT post OS | MET 40mg/mL | 0.125, 0.25, 0.5, 1, 2, 4, 8 | IT is effective in cases of SHL or contraindication. | (36) 34.2 |
| She et al., 2010 China | Otolaryngol Head Neck Surg | Prospective | 49: 26 (IT) 23 (without treatment) | IT post OS | MET 40mg/mL | 0.25, 0.5, 1, 2, 3, 4, 8 | IT through microcatheter is promising for refractory SHL. | (26) 61.9 (23) 21.7 |
| Moon et al., 2011 Korea | Otol Neurotol | Retrospective | 151: 59 (OS), 26 (OS 2 cycles), 66 (OS+IT) | IT post OS | DEX 0.4 at 0.5mL | 0.5, 1, 2, 3 | IT as rescue therapy was more effective than another dose of OS. | (59) 16.9 (26) 15.3 (66) 48.4 |
| Lee et al., 2011 Korea | Eur Archi Otorhinolaryngol | Prospective, case–control, randomized | 46: 21 (IT post OS), 25 (OS) | IT post OS×OS | DEX 0.3 at 0.4mL | 0.5, 1, 2, 3 | IT is simple and effective post OS. | (21) 47.6 (25) 16.0 |
| Barreto et al., 2012 Brazil | Int Tinnitus J | Prospective | 8 | IT post OS | MET | 0.5, 1, 2, 4 | IT was effective in relief of tinnitus. | (8) 25.0 |
| Wang et al., 2012 China | J Zhejiang Univ Sci B | Clinical trial, nonrandomized, retrospective | 55 (IT), 32 (OS) | IT post OS | DEX 10mg | 0.5, 1, 2, 3, 4 | IT is simple and effective post OS. | (55) 82.0 (32) 9.4 |
| Chou et al., 2013 Taiwan | Laryngoscope | Case–control, prospective and retrospective | 60: 30 (IT), 30 transtympanic | IT post OS | 0.5, 1, 2, 4 | IT had better audiological results. | (30) 53.3 (30) 43.3 |
IT; intratympanic; IT post OS, intratympanic salvage therapy post oral steroid IT; OS, oral steroid.
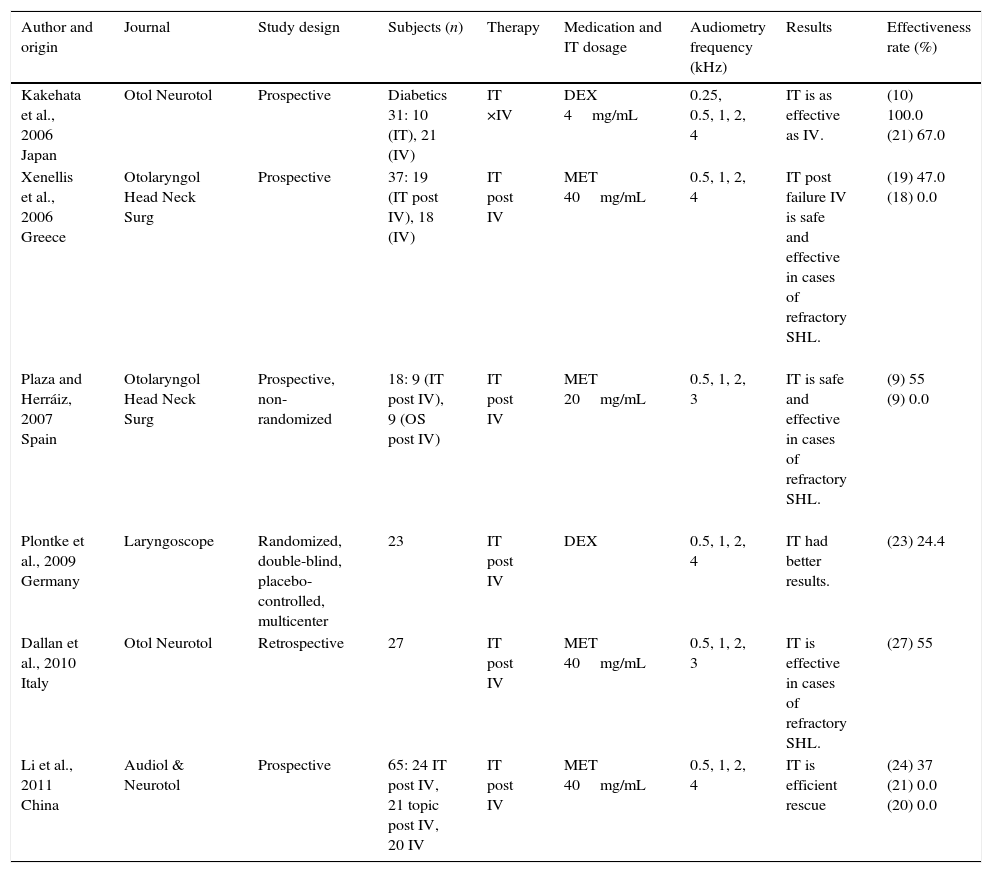
Studies emphasizing salvage therapy after failure of intravenous steroids.
| Author and origin | Journal | Study design | Subjects (n) | Therapy | Medication and IT dosage | Audiometry frequency (kHz) | Results | Effectiveness rate (%) |
|---|---|---|---|---|---|---|---|---|
| Kakehata et al., 2006 Japan | Otol Neurotol | Prospective | Diabetics 31: 10 (IT), 21 (IV) | IT ×IV | DEX 4mg/mL | 0.25, 0.5, 1, 2, 4 | IT is as effective as IV. | (10) 100.0 (21) 67.0 |
| Xenellis et al., 2006 Greece | Otolaryngol Head Neck Surg | Prospective | 37: 19 (IT post IV), 18 (IV) | IT post IV | MET 40mg/mL | 0.5, 1, 2, 4 | IT post failure IV is safe and effective in cases of refractory SHL. | (19) 47.0 (18) 0.0 |
| Plaza and Herráiz, 2007 Spain | Otolaryngol Head Neck Surg | Prospective, non-randomized | 18: 9 (IT post IV), 9 (OS post IV) | IT post IV | MET 20mg/mL | 0.5, 1, 2, 3 | IT is safe and effective in cases of refractory SHL. | (9) 55 (9) 0.0 |
| Plontke et al., 2009 Germany | Laryngoscope | Randomized, double-blind, placebo-controlled, multicenter | 23 | IT post IV | DEX | 0.5, 1, 2, 4 | IT had better results. | (23) 24.4 |
| Dallan et al., 2010 Italy | Otol Neurotol | Retrospective | 27 | IT post IV | MET 40mg/mL | 0.5, 1, 2, 3 | IT is effective in cases of refractory SHL. | (27) 55 |
| Li et al., 2011 China | Audiol & Neurotol | Prospective | 65: 24 IT post IV, 21 topic post IV, 20 IV | IT post IV | MET 40mg/mL | 0.5, 1, 2, 4 | IT is efficient rescue | (24) 37 (21) 0.0 (20) 0.0 |
IT, intratympanic; post-IV, intratympanic salvage therapy post intravenous steroid; OS, oral steroid; IV, intravenous steroid.
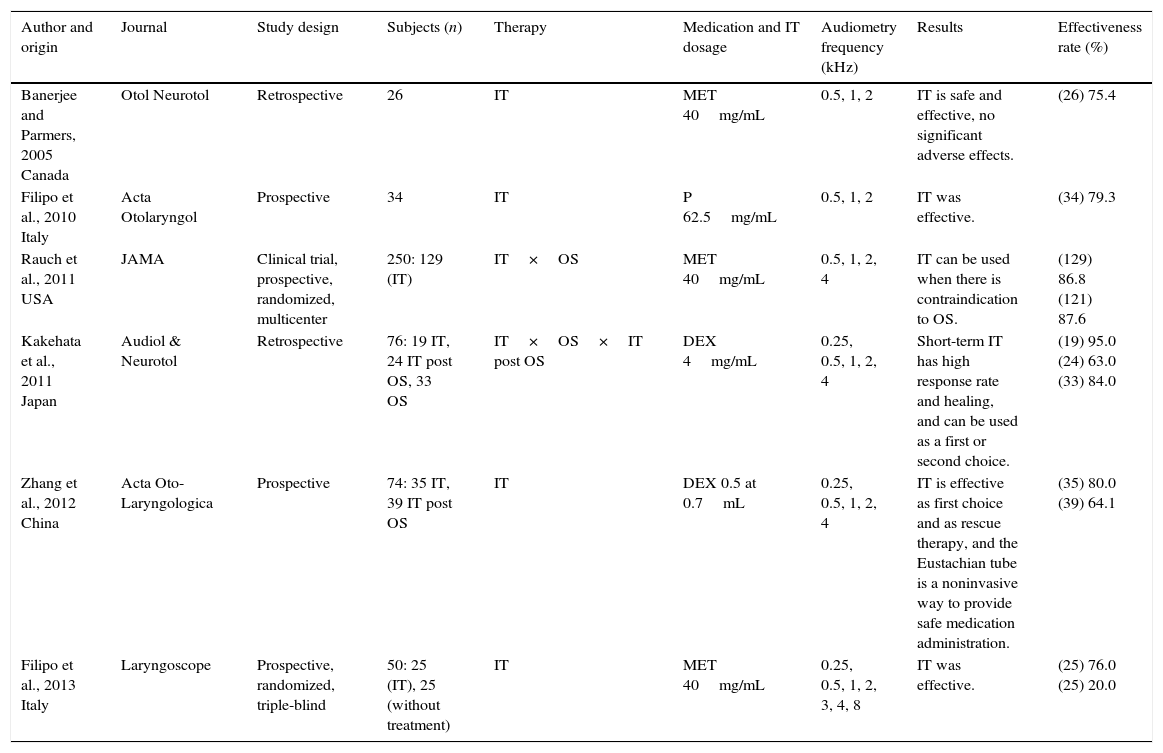
Studies emphasizing primary therapy.
| Author and origin | Journal | Study design | Subjects (n) | Therapy | Medication and IT dosage | Audiometry frequency (kHz) | Results | Effectiveness rate (%) |
|---|---|---|---|---|---|---|---|---|
| Banerjee and Parmers, 2005 Canada | Otol Neurotol | Retrospective | 26 | IT | MET 40mg/mL | 0.5, 1, 2 | IT is safe and effective, no significant adverse effects. | (26) 75.4 |
| Filipo et al., 2010 Italy | Acta Otolaryngol | Prospective | 34 | IT | P 62.5mg/mL | 0.5, 1, 2 | IT was effective. | (34) 79.3 |
| Rauch et al., 2011 USA | JAMA | Clinical trial, prospective, randomized, multicenter | 250: 129 (IT) | IT×OS | MET 40mg/mL | 0.5, 1, 2, 4 | IT can be used when there is contraindication to OS. | (129) 86.8 (121) 87.6 |
| Kakehata et al., 2011 Japan | Audiol & Neurotol | Retrospective | 76: 19 IT, 24 IT post OS, 33 OS | IT×OS×IT post OS | DEX 4mg/mL | 0.25, 0.5, 1, 2, 4 | Short-term IT has high response rate and healing, and can be used as a first or second choice. | (19) 95.0 (24) 63.0 (33) 84.0 |
| Zhang et al., 2012 China | Acta Oto-Laryngologica | Prospective | 74: 35 IT, 39 IT post OS | IT | DEX 0.5 at 0.7mL | 0.25, 0.5, 1, 2, 4 | IT is effective as first choice and as rescue therapy, and the Eustachian tube is a noninvasive way to provide safe medication administration. | (35) 80.0 (39) 64.1 |
| Filipo et al., 2013 Italy | Laryngoscope | Prospective, randomized, triple-blind | 50: 25 (IT), 25 (without treatment) | IT | MET 40mg/mL | 0.25, 0.5, 1, 2, 3, 4, 8 | IT was effective. | (25) 76.0 (25) 20.0 |
IT, intratympanic; IT post OS, intratympanic salvage therapy post oral steroid IT; OS, oral steroid.
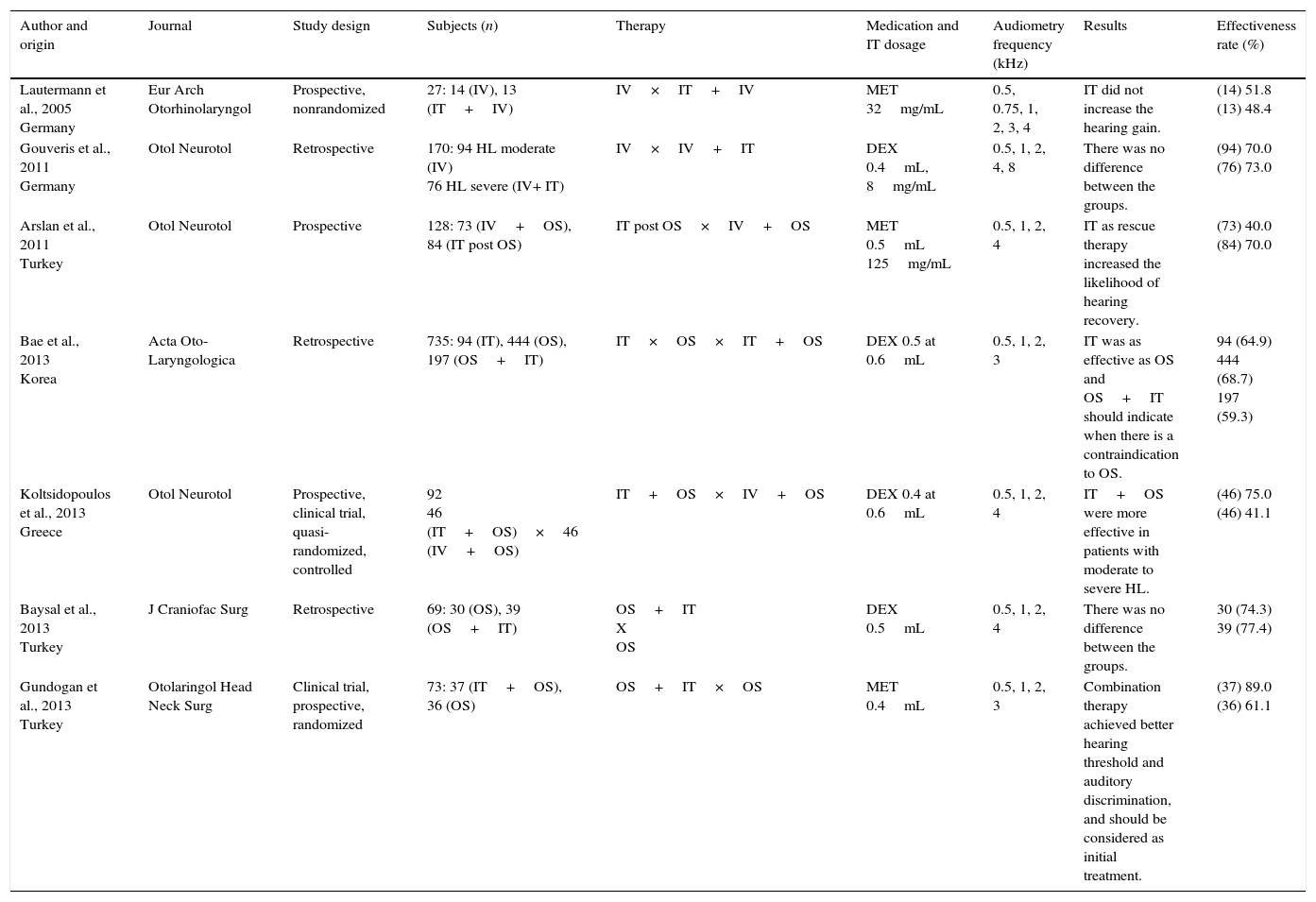
Studies emphasizing combination therapy.
| Author and origin | Journal | Study design | Subjects (n) | Therapy | Medication and IT dosage | Audiometry frequency (kHz) | Results | Effectiveness rate (%) |
|---|---|---|---|---|---|---|---|---|
| Lautermann et al., 2005 Germany | Eur Arch Otorhinolaryngol | Prospective, nonrandomized | 27: 14 (IV), 13 (IT+IV) | IV×IT+IV | MET 32mg/mL | 0.5, 0.75, 1, 2, 3, 4 | IT did not increase the hearing gain. | (14) 51.8 (13) 48.4 |
| Gouveris et al., 2011 Germany | Otol Neurotol | Retrospective | 170: 94 HL moderate (IV) 76 HL severe (IV+ IT) | IV×IV+IT | DEX 0.4mL, 8mg/mL | 0.5, 1, 2, 4, 8 | There was no difference between the groups. | (94) 70.0 (76) 73.0 |
| Arslan et al., 2011 Turkey | Otol Neurotol | Prospective | 128: 73 (IV+OS), 84 (IT post OS) | IT post OS×IV+OS | MET 0.5mL 125mg/mL | 0.5, 1, 2, 4 | IT as rescue therapy increased the likelihood of hearing recovery. | (73) 40.0 (84) 70.0 |
| Bae et al., 2013 Korea | Acta Oto-Laryngologica | Retrospective | 735: 94 (IT), 444 (OS), 197 (OS+IT) | IT×OS×IT+OS | DEX 0.5 at 0.6mL | 0.5, 1, 2, 3 | IT was as effective as OS and OS+IT should indicate when there is a contraindication to OS. | 94 (64.9) 444 (68.7) 197 (59.3) |
| Koltsidopoulos et al., 2013 Greece | Otol Neurotol | Prospective, clinical trial, quasi- randomized, controlled | 92 46 (IT+OS)×46 (IV+OS) | IT+OS×IV+OS | DEX 0.4 at 0.6mL | 0.5, 1, 2, 4 | IT+OS were more effective in patients with moderate to severe HL. | (46) 75.0 (46) 41.1 |
| Baysal et al., 2013 Turkey | J Craniofac Surg | Retrospective | 69: 30 (OS), 39 (OS+IT) | OS+IT X OS | DEX 0.5mL | 0.5, 1, 2, 4 | There was no difference between the groups. | 30 (74.3) 39 (77.4) |
| Gundogan et al., 2013 Turkey | Otolaringol Head Neck Surg | Clinical trial, prospective, randomized | 73: 37 (IT+OS), 36 (OS) | OS+IT×OS | MET 0.4mL | 0.5, 1, 2, 3 | Combination therapy achieved better hearing threshold and auditory discrimination, and should be considered as initial treatment. | (37) 89.0 (36) 61.1 |
IT, intratympanic; IT post OS, intratympanic salvage therapy post oral steroid IT; OS, oral steroid; IV, intravenous steroid.
Regarding the design of the studies, 63.3% were prospective, 30% and 6.7% retrospective prospective and retrospective. Only three studies (10%) were controlled and randomized. Three other studies (10%) were randomized and only two (5%) were controlled.
As to the objectives of the studies analyzed, 76.7% sought to evaluate the use of intratympanic therapy salvage after failure of conventional treatment. Treatment therapy with systemic steroids was considered as conventional therapy; 52.2% of the studies used oral administration and 47.8%, intravenous administration. Intratympanic therapy was used as the primary treatment 23.3% of the studies.
It is noteworthy that 100% of the studies used auditory evaluation by pure tone audiometry as a method of checking the effectiveness of the therapy chosen, mainly using as improvement criteria 20dB increase in the mean frequencies of 0.5, 1, 2, and 4kHz. Of these, some studies included evaluation through speech audiometry and impedance.
Analyzing the articles published on sudden hearing loss and use of intratympanic corticosteroid therapy, the data showed that this is a promising treatment modality, especially for cases where there was a failure in the conventional treatment, as well as in those where systemic corticosteroid therapy is contraindicated.
It can be seen that in most of the analyzed studies, the authors made three intratympanic corticosteroid applications, usually every other day. However, dosages were different, ranging from one to five applications.
Pure tone audiometry was the audiological test used in all the studies analyzed. However, because of the possibility of sudden deafness is multifactorial and affects the inner ear and/or auditory pathways, the authors suggest testing electrophysiological objectives accompanying a patient.
The study by Rauch et al. in 2011 compared the non-inferiority in the two therapeutic approaches for sudden deafness (intratympanic and oral), and 250 subjects were followed for a period of six months. They found that non-inferiority was defined as a difference of less than 10dB in hearing improvement between treatments. In the group treated with oral prednisolone (n=121), the pure tone average (PTA) improved 30.7dB compared to the group receiving intratympanic corticosteroid therapy (n=129), who presented improvement of 28.7dB.4 Similarly to these authors, Dallan et al.,8 in Italy, also followed patients for six months. However, their study examined the efficacy of intratympanic corticosteroid therapy after failure of oral therapy.
Other researchers followed-up for up to three months, and most of the time, during only one month after starting treatment with intratympanic corticosteroid.
The following studies are presented according to the type of therapy used.
Salvage therapy after failure of oral steroidsPlontke et al. evaluated 23 patients with unilateral severe and profound SHL refractory to initial systemic therapy and compared them with a control group (n=23) who did not receive salvage treatment. The PTA threshold after intratympanic salvage treatment showed a statistically significant improvement of 15dB (7–24dB). The local therapy group showed a significantly better improvement (mean 19dB, 6–32dB) than the historical control group (mean 5dB, 2–11dB).9
In 2006, Choung et al. analyzed the effect of intratympanic dexametasone (IT-DEX). Hearing was assessed immediately before every injection and at one week after therapy. Hearing improvement was defined as more than 10dB in PTA and was observed in 13 (39.4%) of 33 patients who underwent IT-DEX, and in two (6.1%) of 34 patients in the control group.10
In 2006, Dallan et al. sought to understand the real efficacy of transtympanic steroid therapy for SHL in patients in whom traditional therapies had failed. A solution of methylprednisolone (MP) and sodium bicarbonate was administered via transtympanic injection to eight patients. Hearing level was evaluated before therapy and at days one, seven, and 30. Hearing improvement was obtained in 75% of the patients.8
In 2010, Raymundo et al. evaluated 14 patients treated with three intratympanic injections of methylprednisolone (IT-MP) after failing treatment with systemic steroids. Pre-treatment and post-treatment audiometric evaluations including PTA at frequencies of 0.5, 1, and 2kHz, and speech reception thresholds (SRT) were analyzed. Ten of 14 patients presented with hearing recovery >20dB in PTA or 20 percent in SRT.5
In 2010, Chen et al. evaluated the effectiveness of IT-MP in 36 patients who failed routine oral steroid therapy and two patients with a contraindication to systemic steroid, with a maximum of four injections. Hearing level, dizziness, and tinnitus were evaluated before the first procedure and 20 days after the last injection. Thirteen of 38 patients (34.2%) showed an improvement in hearing levels. The average improvement 20 days after treatment was 54dB in the hearing thresholds of 0.125–8kHz.11
In 2010, She et al. investigated 26 patients in the study group (SG) who received methylprednisolone (MP) for ten days and the conventional treatment, and 23 patients who received a second conventional treatment (no steroid) served as the comparison group (CG). The PTA improvement was 20.2±15.6dB in the SG, and 9.2±13.7dB in the CG. In the SG, hearing improvement at low frequencies was better than that at high frequencies. The data suggested that the treatment may be more effective when administered at the earlier stages of SHL when the conventional treatment has failed.12
In 2011, Moon et al. investigated the therapeutic efficacy of IT-DEX as a salvage treatment in 151 patients who were totally unresponsive two weeks after treatment initiation. The 151 refractory patients were divided into three groups: those receiving no further treatment (control group, n=59), those receiving one more ten day cycle of oral steroids (systemic reapplication group, n=26), and those receiving IT-DEX therapy (IT-DEX group, n=66). Overall hearing improvement was observed in ten of 59 patients in the control group, in four of 26 in the systemic reapplication group, and in 32 of 66 in the IT-DEX group. Analyzing by frequency, hearing of the low and mid frequencies was more significantly improved than high frequencies in the IT-DEX group.13
In 2011, Lee et al. analyzed patients who were randomly classified into two groups: the IT-DEX group (n=21) received four sequential IT-DEX within two weeks after systemic steroids, and the control group (n=25) took any more medications. Hearing improvement was defined as a 10dB or more decrease in the PTA of the four frequencies (0.5, 1, 2, and 3kHz). Hearing improvement was observed in ten (47.6%) of 21 IT-DEX patients and in four (16.0%) of 25 control patients. The improvement of the mean PTA was 11.4dB in the IT-DEX group and 1.7dB in the control group. The IT-DEX group showed significant hearing improvement at low frequency (0.5Hz) compared to the control group. The patients with ≥70dB in PTA before IT-DEX showed significant hearing improvement compared to the other patients with better PTAs.6
In 2012, Barreto et al. analyzed the effectiveness of oral and intratympanic steroids for tinnitus control in eight patients with SHL and severe disabling tinnitus. Hearing evaluation and application of the Tinnitus Handicap Inventory and visual analogue scale were performed before and after treatment of sudden deafness with oral and intratympanic steroids. Two patients showed improvement in the hearing, but seven showed large improvements in their tinnitus, which was demonstrated by an improvement in the values of the degrees of severity of tinnitus. Patients with SHL and severe disabling tinnitus who underwent intratympanic and oral corticosteroids showed, in this study, significant reduction and/or remission of tinnitus.14
In 2012, Wang et al. observed and compared the efficacy of IT-DEX for the treatment 55 patients with refractory SHL. For 21 patients (the perfusion group), DEX (2.5mg/0.5mL) was perfused transtympanically through a round window catheter, using an infusion pump for one hour twice a day for seven days, giving a total amount of 35.0mg. For 23 patients (the injection group), DEX (2.5mg/time) was injected by tympanic membrane puncture at intervals of two days on a total of four occasions, giving a total amount of 10.0mg. For 11 patients (the drip group), DEX (2.5mg/0.5mL) was dripped via a ventilation tube placed by myringotomy, once on the first day and twice a day for the remaining six days, giving a total amount of 32.5mg. Thirty-two patients with refractory SHL who refused to undertake further treatments were defined as the control group. Hearing results were evaluated based on PTA in four frequencies (0.5, 1, 2, and 4kHz). The improvements in mean PTA for the perfusion, injection, and drip groups were 9.0, 8.6, and 1.7dB, respectively. Hearing improvement was significantly greater in the perfusion and injection groups than in the control group (1.4dB). In the perfusion group, eight out of 21 patients (38.1%) had a PTA improvement of 15–56dB (mean 29.8dB); in the injection group, eight out of 23 patients (34.8%) had a PTA improvement of 16–54dB (mean 24.9dB); in the drip group, one of 11 patients (9.1%) had a PTA improvement of 26.0dB; in the control group, three out of 32 patients (9.4%) had a PTA improvement of 15–36dB (mean 14.9dB).15
In 2013, Chou et al. investigated whether near-continual transtympanic steroid perfusion is more effective than intermittent intratympanic steroid injection as a salvage therapy for SHL in 60 patients. The pre-salvage pure tone threshold was 65.4±13.5dB in the transtympanic steroid perfusion group. After the therapy, the hearing threshold was improved by an average of 15.0±9.7dB, and 53.3% of subjects had improved by 10dB or more. The speech discrimination score (SDS) was improved from 12.6±7.0% to 54.4±6.4%. In the intratympanic steroid injection group, the pre-salvage pure tone threshold was 68.8±16.0dB. After the therapy, the hearing threshold was improved by an average of 10.7±9.8dB, and 43.3% of subjects had improved by 10dB or more. The speech discrimination score was improved from 13.3±6.0% to 46.4±12%.16
Topical intratympanic injection may be considered as a substitute for systemic administration in patients with refractory SHL, especially those who have contraindications to systemic steroid administration.
Salvage therapy after failure of intravenous steroidsIn 2006, Xenellis et al. analyzed 37 patients with SHL who, at the end of ten days of therapy with intravenous steroids as a first line treatment, had four frequency PTA (0.5, 1, 2, and 4kHz) and were randomized into two groups: treatment and control. Nineteen patients of the treatment group received approximately 0.5mL sterile aqueous suspension of MP in a concentration of 80mg/2mL by direct injection. The procedure was carried out four times, and an audiogram was performed before each injection and approximately 1.5 months after the last session. With regard to the 19 patients who received intratympanic treatment (IT), in nine patients, the PTA threshold improved more than 10dB, in ten patients there was no change greater than 10dB, and no patients deteriorated more than 10dB. In the control group, none of the patients showed any change greater than 10dB. The difference was statistically significant. The treatment group showed an improvement in mean PTA of 14.9dB, whereas the control group showed a deterioration of 0.8dB, and this difference also was statistically significant.17
In 2006, Kakehata et al. evaluated the efficacy of IT-DEX treatment on SHL patients with diabetes by comparing the results with intravenous administration of dexamethasone (IV-DEX) treatment. In the IT-DEX group (n=10, 4mg/mL for eight days) the average hearing level before the treatment was 79dB. Overall, all ten patients showed improvement of more than 10dB in the PTA, with a mean improvement of 41dB. Seven patients (70%) demonstrated successful results, and four recovered completely. In the IV-DEX group (n=21, 8mg/d for ten days), 14 (67%) showed improvement of more than 10dB, with a mean improvement of 25dB. Thirty-three patients (62%) demonstrated successful results. IT-DEX treatment is at least as effective as IV-DEX treatment for SHL patients with diabetes.18
In 2007, Plaza and Herráiz described their experience with 50 patients presenting with idiopathic SHL, treated intravenously over five days. After this period, patients with treatment failure (18 cases) were offered intratympanic steroid treatment. Nine patients refused, whereas the other nine patients received three weekly injections of MP. Recovery of hearing was reported as improvement of more than 15dB in PTA. Intratympanic steroid treatment improved hearing loss in five patients (55%).19
In 2009, Plontke et al. studied the safety and efficacy of continuous IT-DEX in patients with SHL and insufficient recovery (mean four PTA=97dB) after systemic high-dose glucocorticoid therapy, who received either IT-DEX (4mg/mL) or placebo (NaCl 0.9%) continuously applied for 14 days. Intention-to-treat analysis for the primary outcome criterion (four PTA: 0.5, 1, 2, 3kHz) during the placebo controlled study period (14 days) showed an average hearing improvement in the treatment group of 13.9dB and in the placebo group of 5.4dB. Of the secondary outcome parameters, the largest benefit of local salvage therapy was found for maximum speech discrimination, with an improvement of 24.4% in the treatment and 4.5% in the placebo group. After a three-month follow-up period, hearing improvement in the two groups was very similar.20
In 2010, Dallan et al. analyzed 27 patients unresponsive to traditional systemic therapy who were treated with intratympanic steroids. The mean PTA before intratympanic treatment was 79.9±21.4dB; at day 30, after local steroid administration, the mean PTA was 60.6±24.9dB. Fifteen (55%) of 27 patients presented a “useful” improvement in the hearing status, to confirm the usefulness (at least 50% of patients) of local steroids administration in cases of refractory SHL.21
In 2011, Li et al. followed 65 patients with SHL who did not respond to IV treatment with prednisolone, randomized into three groups: treatment with IT steroid, treatment with steroid in ear drops, and a control group. The 24 patients in the IT group received IT-MET, and the 21 patients in the eardrop group received IT-MET that was directly dropped onto the tympanic membrane through the ear canal. In the IT treatment group, audiogram results showed that the PTA for speech frequencies (0.5, 1, 2, and 4kHz) was 52.9dB at the end of systemic treatment, and 64.8dB at the end of IT treatment. The improvement in the IT group was significantly better than that in the other two groups, with 37% of the IT patients demonstrating significant improvement in their hearing.22
IT steroid administration after failed intravenous steroids is a safe and effective treatment in sudden hearing loss.
Primary therapyIn 2005, Banerjee and Parners determined whether instillation of intratympanic steroids (methylprednisolone and/or dexamethasone) is effective in the treatment of SHL. Pre-treatment and post-treatment of 26 patients’ PTA and SDS were compared. Overall, there was a 27.2±5.7dB improvement in the pure tone thresholds and a 25.4%±6.2% improvement in SDS.23
In 2010, Filipo et al. evaluated the overall success rate, morbidity, and prognostic factors of a protocol of intratympanic steroid administration as a means of primary therapy for SHL. 34 patients were treated once a day for three consecutive days with a single intratympanic injection of prednisone diluted in saline solution. Among them, 16 patients (47%) reported complete recovery, with a PTA that returned within 25dB; 11 patients (32.3%) showed improvement in hearing of more than 30dB, and four patients presented improvement in PTA between 10 and 30dB.24
In 2011, the clinical study by Rauch et al. from Harvard University was a scientific milestone because of the number of monitored patients (n=250). It was a multicentric study, including 16 research centers and universities in North America and comparing the efficacy of two therapeutic methods for unilateral SHL, namely, intratympanic corticosteroids as a first-line treatment and oral corticosteroids, also as a first-line treatment. The patients were followed for six months. One hundred twenty-nine patients received four doses of MET 40mg/mL and 121 patients received oral prednisolone 60mg/day. The results demonstrated no statistically significant difference when comparing the two treatment methods. These findings could be obtained after analyzing the audiological results by pure tone audiometry, analyzing means in the frequencies 0.5Hz, 1, 2, and 4kHz.4
In 2011, Kakehata et al. evaluated the efficacy of daily short-term IT-DEX treatment alone in 76 SHL patients for initial and/or salvage treatment. The average hearing level was determined by five frequencies (0.25, 0.5, 1, 2, and 4kHz). 19 out of 76 patients fit the criteria for initial treatment in the study (group I), while 24 patients, who had failed systemic therapy, received salvage treatment (group S). In group I, 18 of the 19 patients (95%) showed improvement of more than 10dB in the PTA, with a mean improvement of 40dB. 20 patients (63%) recovered completely and 16 patients (84%) demonstrated successful results, with an improvement of more than 30dB. In group S, 14 of the 24 patients (58%) showed improvement of 16dB and two (8%) of the seven patients (29%) with successful results recovered completely. Daily short-term IT-DEX administration using LAM for SHL patients without concurrent therapy showed a high response rate and high cure rate, and proved to be an alternative therapeutic option to high-dose systemic steroids as a first- and/or second-line treatment.7
In 2012, Zhang et al. investigated the effectiveness and safety of noninvasive IT-DEX perfusion through the Eustachian tube in 74 patients with SHL. 35 patients met the criteria for initial treatment in the study (Group I), while 39 patients, who had failed systemic therapy, received salvage treatment (Group S). IT-DEX perfusion through the Eustachian tube was applied four times at two-day intervals. Pure tone test and tympanometry were performed before starting treatment, and 24h and one week afterwards. With regard to the 74 patients who received IT, 80.0% (28 of 35) of the patients in Group I and 64.1% (25 of 39) patients in Group S had improvement in their hearing ability. Noninvasive IT-DEX perfusion through the Eustachian tube is an effective and safe therapy in cases of SHL.25
In 2013, Filipo et al. investigated 50 patients affected by moderate SHL, involving all frequencies from 250Hz to 8kHz (a flat audiogram). Patients were randomized into two groups of 25 each. The first group (intratympanic steroid) underwent a daily intratympanic administration of prednisolone for three consecutive days. The second group (control) received a daily intratympanic injection of a saline solution for three consecutive days. Audiometric tests were performed at day seven after the beginning of therapy (T1), and then 10 and 30 days after T1. The patients in both groups who did not show a complete recovery at T1 were treated with oral prednisone at a tapering dose. In the intratympanic steroid group, 19 out of 25 patients presented complete recovery at T1 (76%), whereas in the control group, the number of patients who recovered completely at T1 was five out of 25 (20%). The PTA recorded at T1 demonstrated a statistically significant improvement in the hearing threshold of the first group compared to the control group. The mean PTA recorded after the first-line treatment (T1) demonstrated a significant therapeutic action of the short-duration intratympanic steroid therapy on moderate SHL, with a flat audiogram shape, compared to the natural course of the disease and the placebo effect at that time point.26
IT is safe, effective, without significant adverse effects, and can be used as a first or second choice.
Combination therapyIn 2005, Lautermann et al. analyzed 27 patients with profound SHL. Fourteen were treated with a rheologic infusion therapy consisting of systemic prednisolone, and 13 were treated additionally with methylprednisolone transtympanically through a ventilation tube. In the first group, three patients had good recovery of hearing. Another five patients had a partial recovery. The average hearing gain from 0.5, 0.75, 1, 2, 3, and 4kHz was 15dB. In the group of patients who were treated additionally with local corticoids, two reported a good recovery of hearing and another two only had a partial recovery. The additional transtympanic application of corticoids did not result in a significantly improved recovery of hearing in comparison to the patients treated with the standard therapy alone.
In 2011, Gouveris et al. evaluated the differences in effectiveness between SHL patients treated with intravenous therapy alone and patients treated with a combination of intravenous and intratympanic therapy. Ninety-four patients with moderate SHL were treated with an intravenous steroid and vasoactive regimen, and 76 patients with severe SHL were treated with a combination regimen of intravenous and intratympanic therapy. In the latter group, a series of three IT-DEX were applied every two days. PTA at 0.5, 1, 2, 4, and 8kHz were compared between groups. The combination therapy in severe SHL did not show any statistically significant difference in effectiveness compared to intravenous therapy in moderate SHL. In patients with severe SHL, starting intratympanic steroid therapy as an adjunct early in the course of intravenous steroid and vasoactive therapy improved hearing to a level which is obtained in patients with less severe (moderate) SHL treated with intravenous therapy alone.27
In 2011, Arslan et al. compared hearing results in SHL in 158 patients treated with systemic steroids alone, or combined intratympanic and steroids. Seventy-three patients in the systemic therapy group received consecutive administration of 100mg intravenous methylprednisolone in the first day, then 80mg/day oral prednisolone in three divided doses for the next two days, and continued with oral administration of steroids by tapering the dose 20mg in every two days. Eighty-five patients in the combined treatment group received intratympanic injection of methylprednisolone (an approximate dose of 0.5mL at 125mg/mL). A total of five injections on alternate days were performed. The mean and median PTA gains of systemic corticosteroid therapy (SCT) group were 7.5 and 5dB at fifth day, 12.1 and 7.5dB at tenth day, and 13.0 and 8.8dB at 15th day. The mean and median PTA gains for combined treatment (CT) group were 12.5 and 7.5dB, 17.8 and 13.8dB, and 21.8 and 20.0dB, respectively. Both the mean and the median PTA gains were significantly different between the SCT and CT groups, and adding intratympanic methylprednisolone to systemic therapy increased the probability of hearing recovery in patients with SHL.28
In 2013, Baysal et al. evaluated the effectiveness of 30 patients using oral steroid treatment vs. 39 patients using combined oral and IT-DEX for SHL. The comparison of the initial PTA threshold results revealed a significant difference between the systemic steroid (SS) group and the systemic and IT steroid group. The initial PTA was 74.33dB in the SS group and 87.49dB in the IT steroid group. The difference in the initial PTA results was significant between the SS group and IT steroid group. The pure tone gain in the SS group was 20.97dB, and that of the group treated with both systemic and IT steroids was 19.36dB. In SHL, the administration of IT steroids in conjunction with SS therapy appears to have the same effect on the restoration of hearing as the effect obtained using SS therapy alone.29
In 2013, Gundogan et al. compared the efficacy of SS alone and combined with IT-MET in the treatment of 73 patients. The patients were randomly divided into two groups according to treatment: group A (n=37) received combination therapy (intratympanic methylprednisolone and oral steroid) and group B (n=36) received oral steroid alone. Group A demonstrated significant hearing improvement and SDS compared with the use of SS alone. In hearing outcomes in patients with severe hearing loss, combination therapy showed statistically significant hearing improvement compared with oral steroid alone, and combination therapy can be considered as an initial treatment, especially for patients with severe hearing loss.30
In 2013, Koltsidopoulos et al. investigated the therapeutic efficacy of IT-DEX combined with systemic prednisolone in 92 patients allocated into two groups. The control group was treated with systemic prednisolone alone and patients in the combined treatment group received three additional IT-DEX injections within five days. The main outcome measures used were the differences between pre-treatment and post-treatment PTA and SDS. Successful treatment was defined as a greater than 10dB improvement in PTA and 15% in SDS. Audiometric evaluation was performed regularly every other day during admission, and subsequently once a month after the discharge. The final assessment of the patients in both groups was performed three months after the completion of treatment.31
In 2013, Bae et al. compared the therapeutic efficacy of intratympanic steroid therapy (IT-S) and combined therapy with SS therapy and IT-S in 735 patients. The patients were divided into three groups: 94 in the IT-S group, 444 in the SS therapy group, and 197 in the combined therapy group (SS plus IT-S). Hearing was evaluated by PTA before initial treatment and at four weeks following the final treatment. A decrease of more than 10dB in average air conduction hearing threshold at 0.5, 1, 2, and 3kHz was defined as improved hearing. No difference in the level of hearing gain or ratio of hearing improvement was observed among the three groups. IT-S was as effective as SS therapy or combined therapy and could be considered a first-line therapeutic modality for SHL. Due to its known safety and efficacy, IT-S should be particularly suitable for patients with SHL who have chronic diseases such as diabetes mellitus, hypertension, or chronic renal failure.32
Some studies have shown benefits in combined therapy, especially for patients with moderate to severe hearing loss, while others found no difference.
ConclusionIntratympanic corticosteroid therapy is prescribed primarily when there is failure of conventional therapy or when use of systemic corticosteroids is limited, such in diabetic patients.
Based on these results, there is still need for more prospective studies with control groups and standardization of treatment for comparison of the data obtained and applicability of the proposed therapy, as well as audiological follow-up through acoustic and electrophysiological methods.
Intratympanic corticosteroid therapy is indicated especially when there is failure of conventional therapy and when the use of systemic corticosteroids should be avoided.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Barreto MASC, Ledesma ALL, de Oliveira CACP, Bahmad Jr F. Intratympanic corticosteroid for sudden hearing loss: does it really work? Braz J Otorhinolaryngol. 2016;82:353–64.
Institution: Universidade de Brasília (UnB), Brasília, DF, Brazil.