The main reason for nasal tampon placement after septoplasty is to prevent postoperative hemorrhage, while the secondary purpose is internal stabilization after operations involving the cartilaginous-bony skeleton of the nose. Silicone intranasal splints are as successful as other materials in controlling postoperative hemorrhages of septal origin. The possibility of leaving the splints intranasally for extended periods helps stabilize the septum in the midline. However, there is nothing in the literature about how long these splints can be retained inside the nasal cavity without increasing the risk of infection, postoperative complications, and patient discomfort.
ObjectiveThe current study aimed to evaluate the association between the duration of intranasal splinting and bacterial colonization, postoperative complications, and patient discomfort.
MethodsPatients who had undergone septoplasty were divided into three groups according to the day of removal of the silicone splints. The splints were removed on the fifth, seventh, and tenth postoperative days. The removed splints were microbiologically cultured. Early and late complications were assessed, including local and systemic infections, tissue necrosis, granuloma formation, mucosal crusting, synechia, and septal perforation. Postoperative patient discomfort was evaluated by scoring the levels of pain and nasal obstruction.
ResultsNo significant difference was found in the rate of bacterial colonization among the different groups. Decreased mucosal crusting and synechia were detected with longer usage intervals of intranasal silicone splints. Postoperative pain and nasal obstruction were also diminished by the third postoperative day.
ConclusionsSilicone splints were well tolerated by the patients and any negative effects on postoperative patient comfort were limited. In fact, prolonged splint usage intervals reduced late complications. Long-term silicone nasal splint usage is a reliable, effective, and comfortable method in patients with excessive mucosal damage and in whom long-term stabilization of the bony and cartilaginous septum is essential.
A principal razão para a colocação de tampões nasais em septoplastias é a prevenção de hemorragia pós-operatória, enquanto o objetivo secundário é a estabilização interna após cirurgias que envolvam o esqueleto cartilaginoso do nariz. Os splints intranasais de silicone são tão eficazes como outros materiais para o controle de hemorragias do septo no pós-operatório. A possibilidade de manter os splints intranasais por longos períodos ajuda a estabilizar o septo na linha média. No entanto, não há nada na literatura sobre quanto tempo esses splints podem ser mantidos na cavidade nasal sem aumentar o risco de infecção, complicações no pós-operatório e causar desconforto ao paciente.
ObjetivosO presente estudo teve como objetivo avaliar a associação entre o tempo de tamponamento com splints intranasais e colonização bacteriana, complicações no pós-operatório e desconforto do paciente.
MétodoOs pacientes submetidos a septoplastia foram divididos em três grupos, de acordo com o dia da remoção dos splints de silicone. Os splints foram removidos no 5°, 7° e 10° dias de pós-operatório, e a seguir, cultivados microbiologicamente. Complicações precoces e tardias foram avaliadas, incluindo infecções locais e sistêmicas, necrose do tecido, formação de granulomas, crostas na mucosa, sinéquias e perfuração do septo. O desconforto do paciente no pós-operatório foi avaliado com o uso de pontuação dos níveis de dor e de obstrução nasal.
ResultadosNenhuma diferença significante foi encontrada na taxa de colonização bacteriana entre os diferentes grupos. Diminuições da formação de crostas na mucosa e de sinéquias foram detectadas com tempos mais longos de uso de splints de silicone. A dor e a obstrução nasal também diminuíram no terceiro dia de pós-operatório.
ConclusõesO uso de splints de silicone foi bem tolerado pelos pacientes, e seus efeitos negativos sobre o conforto do paciente no pós-operatório foram limitados. De fato, o tempo prolongado de uso teve um efeito redutor sobre as complicações tardias. O uso prolongado de splint nasal de silicone é um método confiável, eficaz e pouco desconfortável em pacientes com lesão excessiva da mucosa e naqueles cuja estabilização óssea e cartilaginosa do septo a longo prazo é essencial.
Surgical interventions directed at the nasal septum are frequently applied in the daily practices of Ear, Nose, and Throat (ENT) specialists. Septal surgery for functional and esthetic purposes is commonly performed. The methods and materials used in nasal packing are numerous in septoplasty. Various materials including cotton tape, gauze, paraffin gauze, Tefla, Merocel, sponges, and silicone nasal splints have been recommended for this purpose.1
Although these materials have been employed primarily to prevent possible hemorrhage following several interventions, they are also expected to contribute to the stabilization of the nasal cartilaginous bony skeleton at the midline and promote mucosal healing.2,3 Additionally, nasal packing is used to prevent synechiae or restenosis, particularly after surgery.2,3 Recently, silicone nasal splints have been used after both functional interventions directed at the septum and after esthetic procedures. Nasal obstruction is less frequent when appropriate nasal lavages are performed and silicone splints aid hemostasis as much as other materials.1,2 However, the support they provide to assist in maintaining the septum in the midline and their facilitating effect on mucosal healing in cases of possible mucosal injury are the main reasons for the selection of silicone nasal splints.2–4
Recently, silicone splints have become more preferable in septum surgery compared to the other materials. Silicone splints have the advantage of being safely and comfortably retained intranasally longer than other materials. This interval can be lengthened up to 10 days in some cases. However, some local and rare systemic complications (e.g., tissue necrosis, infections, etc.) may arise during intranasal tampon applications.5–11
Unfortunately, there is no information in the literature concerning how long these splints can be retained intranasally without increasing the risk of complications. Also, studies are limited concerning the effects of splint usage intervals on patient discomfort and complications, such as mucosal crusting and synechia. The current study aimed to evaluate the association of intranasal splinting intervals with bacterial colonization, early and late complications (tissue necrosis, mucosal crusting, and synechia), and patient discomfort. Another goal was to determine the optimal intranasal retention time for silicone splints after surgery.
MethodsSubjectsThis was a prospective randomized clinical trial. Patients who had undergone septoplasty and functional septorhinoplasty between February 2014 and September 2014 at the Haseki Training and Research Hospital were included in the study. The patients were chosen by sealed envelope and randomly assigned into one of three groups (Groups 1–3). All patients underwent a detailed examination including nasal endoscopy, anterior rhinoscopy, and computed tomography (CT) scan, if necessary, in order to exclude other sinonasal pathologies. The patients receiving operations other than septoplasty, such as turbinate surgery, sinus surgery, and revision cases, were excluded from this study. Patients who required a rhinoplasty and osteotomy were also excluded. However, patients who had a high dorsal septal deviation and required open septoplasty were admitted to the study. These patients were preoperatively equally distributed to all groups. Patients with systemic diseases or immunosuppression were also excluded. Patients who failed to follow postoperative instructions and take medications properly were excluded in the evaluation phase.
Three patient groups were created according to the removal time of the silicone splints. The splints were removed on the fifth, seventh, and tenth postoperative days in Groups 1, 2, and 3, respectively. The number of patients in Groups 1, 2, and 3 were 32, 33, and 30, respectively. Group 1 consisted of 24 male and eight female patients with a mean age of 30.0±8.1 years (range: 19–47 years); Group 2 consisted of 25 male and eight female patients with a mean age of 29.7±8.1 years (range: 19–47 years); and Group 3 consisted of 20 male and ten female patients with a mean age of 29.0±7.14 years (range: 18–42 years). The mean ages of the three groups were not different from each other (p=0.890). All subjects were volunteers and written informed consent was obtained once the patients were fully apprised of the design, aim, and clinical implications of the study.
Surgical proceduresAll procedures were performed under general anesthesia by the same surgeon. Either an open approach or Killian's method was chosen for the septoplasty technique according to the septal pathology. Polyglactin 910 suture (Vicryl Rapide™; Ethicon – CA, United States) was used in Killian's method and polypropylene suture (Prolene®; Ethicon – CA, United States) was used in the open approach. These suture materials were only used for closing at the initial incision lines. Transseptal sutures were not used in any patients. Silicone splints with airway tubes (Doyle™ Intranasal Airway Splint; Medtronic – MN, United States) were inserted in each nasal cavity after the surgery. Preoperative intravenous antibiotic prophylaxis with sulbactam–ampicillin was administered to all patients. Postoperative oral antibiotic treatments were administered until the removal of the silicone splints, in accordance with the routine practice in this clinic. In the current study, cefdinir tablets (300mg) were administered postoperatively two times per day. Cefdinir was preferred for its Gram-positive and Gram-negative efficacy.12–14 Additionally, nasal lavage with saline solution was prescribed four times per day.
Patient discomfortPostoperative patient discomfort was evaluated by visual analog scale (VAS) scoring of nasal obstruction and pain. VAS scores for postoperative pain measurements (0–10; 0: no pain, 10: unacceptable pain) were noted by the patients every morning before taking analgesics from the first postoperative day until the splints were removed. Postoperative nasal obstruction was also evaluated by VAS scoring (0 to 10; 0: no obstruction, 10: full obstruction) every morning after nasal lavage.
ComplicationsComplications were evaluated in two categories, which included bacterial colonization/infection related to early complications and late complications (mucosal crusting and synechia).
At the control examination, all patients were observed and evaluated for pressure tissue necrosis and local and systemic infection signs (e.g., nasal vestibular hyperemia, tenderness, purulent discharge, septal hematoma, septal abscess, fever, and general poor health in the postoperative period).
Mucosal crusting and synechia were evaluated by nasal endoscopy on the tenth and 20th days after the removal of the splints. On the tenth day nasal endoscopic inspection, crusts covering more than 25% of the nasal septum area or causing a disruption of the nasal airflow were defined as prolonged mucosal crusting. All of these analyses were performed by the same person. The surgeon who performed the operations did not participate in this evaluation.
Microbiological proceduresMaterial removed from the right nasal cavity was included in the study in all patients. Tryptic soy broth (2mL) was poured on the splints, which were then sent to the microbiology laboratory to be incubated for 2h at 37°C. A 0.01mL sample from the fluid samples containing the splints was obtained and cultivated in chocolate agar and McConkey agar. Plaques kept in the incubator were evaluated after 24 and 48h and colony counts were performed. Bacterial identification was performed for each colony using conventional methods.
Statistical analysisRate and frequency values were used in the descriptive statistics. The chi-squared test and Fischer's test (when chi-squared test conditions were not met) were used in the analysis of categorical data. SPSS 22.0 software (SPSS Inc. – Chicago, IL, United States) was used for statistical analysis.
Ethical approval for the study was obtained from the Haseki Training and Research Hospital Ethics Committee on February 5, 2014 (Protocol No. 38).
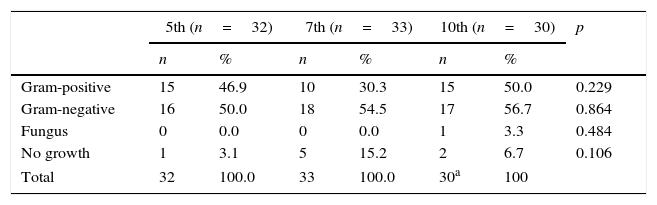
ResultsBacterial colonization and infection-related early complicationsNo significant differences between the three groups regarding bacterial colonization rates of Gram-positive and Gram-negative bacteria (p=0.229), fungi (p=0.864), or other microorganisms (p=0.484), and no growth (p=0.106) were found (Table 1).
Culture results according to the groups.
| 5th (n=32) | 7th (n=33) | 10th (n=30) | p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Gram-positive | 15 | 46.9 | 10 | 30.3 | 15 | 50.0 | 0.229 |
| Gram-negative | 16 | 50.0 | 18 | 54.5 | 17 | 56.7 | 0.864 |
| Fungus | 0 | 0.0 | 0 | 0.0 | 1 | 3.3 | 0.484 |
| No growth | 1 | 3.1 | 5 | 15.2 | 2 | 6.7 | 0.106 |
| Total | 32 | 100.0 | 33 | 100.0 | 30a | 100 | |
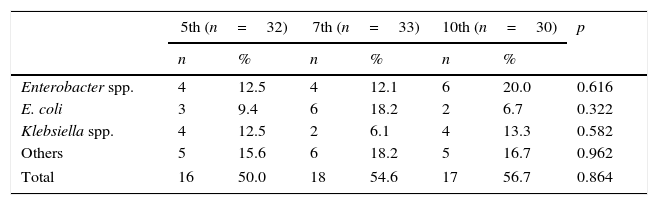
When Gram-negative bacterial colonization was evaluated according to the intranasal splint retention interval, the growth rate of the main pathogenic species (Enterobacter spp., Escherichia coli, and Klebsiella spp.) and other species were not significantly different among Groups 1–3 (p=0.616, p=0.322, p=0.582, and p=0.962, respectively; Table 2).
Distribution of the main Gram-negative pathogen bacteria among the groups.
| 5th (n=32) | 7th (n=33) | 10th (n=30) | p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Enterobacter spp. | 4 | 12.5 | 4 | 12.1 | 6 | 20.0 | 0.616 |
| E. coli | 3 | 9.4 | 6 | 18.2 | 2 | 6.7 | 0.322 |
| Klebsiella spp. | 4 | 12.5 | 2 | 6.1 | 4 | 13.3 | 0.582 |
| Others | 5 | 15.6 | 6 | 18.2 | 5 | 16.7 | 0.962 |
| Total | 16 | 50.0 | 18 | 54.6 | 17 | 56.7 | 0.864 |
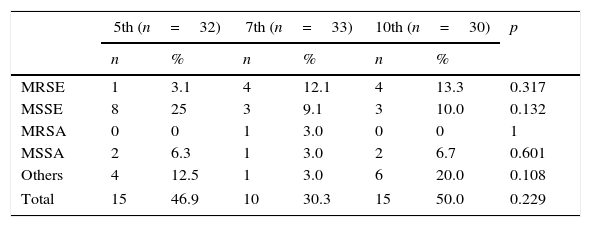
When Gram-positive bacterial colonization was evaluated according to the intranasal splint retention interval, the growth rate of methicillin-resistant Staphylococcus epidermidis (MRSE), methicillin sensitive S. epidermidis (MSSE), methicillin-resistant Staphylococcus aureus (MRSA), methicillin-sensitive S. aureus (MSSA), and other types of species were not significantly different among Groups 1–3 (p=0.317, p=0.132, p=1, p=0.601, and p=0.108, respectively; Table 3).
Distribution of Gram-positive bacteria among the groups.
| 5th (n=32) | 7th (n=33) | 10th (n=30) | p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| MRSE | 1 | 3.1 | 4 | 12.1 | 4 | 13.3 | 0.317 |
| MSSE | 8 | 25 | 3 | 9.1 | 3 | 10.0 | 0.132 |
| MRSA | 0 | 0 | 1 | 3.0 | 0 | 0 | 1 |
| MSSA | 2 | 6.3 | 1 | 3.0 | 2 | 6.7 | 0.601 |
| Others | 4 | 12.5 | 1 | 3.0 | 6 | 20.0 | 0.108 |
| Total | 15 | 46.9 | 10 | 30.3 | 15 | 50.0 | 0.229 |
MRSE, methicillin resistant Staphylococcus epidermidis; MSSE, methicillin sensitive Staphylococcus epidermidis; MRSA, methicillin resistant Staphylococcus aureus; MSSA, methicillin sensitive Staphylococcus aureus.
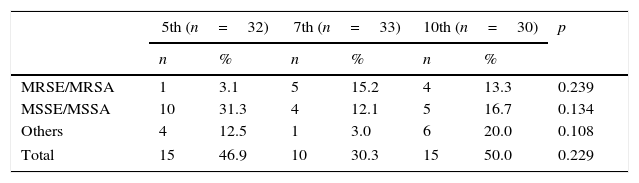
When the staphylococci with and without methicillin-resistance were analyzed together, the growth rate of MRSE/MRSA (major pathogenic species), MSSE/MSSA (can be found in nasal flora), and other species in Groups 1–3 were not significantly different (p=0.239, p=0.134, and p=0.108, respectively; Table 4).
Distribution of Gram-positive bacteria among the groups according to the methicillin resistance.
| 5th (n=32) | 7th (n=33) | 10th (n=30) | p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| MRSE/MRSA | 1 | 3.1 | 5 | 15.2 | 4 | 13.3 | 0.239 |
| MSSE/MSSA | 10 | 31.3 | 4 | 12.1 | 5 | 16.7 | 0.134 |
| Others | 4 | 12.5 | 1 | 3.0 | 6 | 20.0 | 0.108 |
| Total | 15 | 46.9 | 10 | 30.3 | 15 | 50.0 | 0.229 |
MRSE, methicillin resistant Staphylococcus epidermidis, MSSE, methicillin sensitive Staphylococcus epidermidis; MRSA, methicillin resistant Staphylococcus aureus; MSSA, methicillin sensitive Staphylococcus aureus.
All patients were observed and evaluated for infection related to early local and systemic complications (e.g., pressure tissue necrosis, nasal vestibular hyperemia, tenderness, purulent discharge, septal hematoma, abscess, fever, and general poor health). No local or systemic complications in the postoperative period were detected.
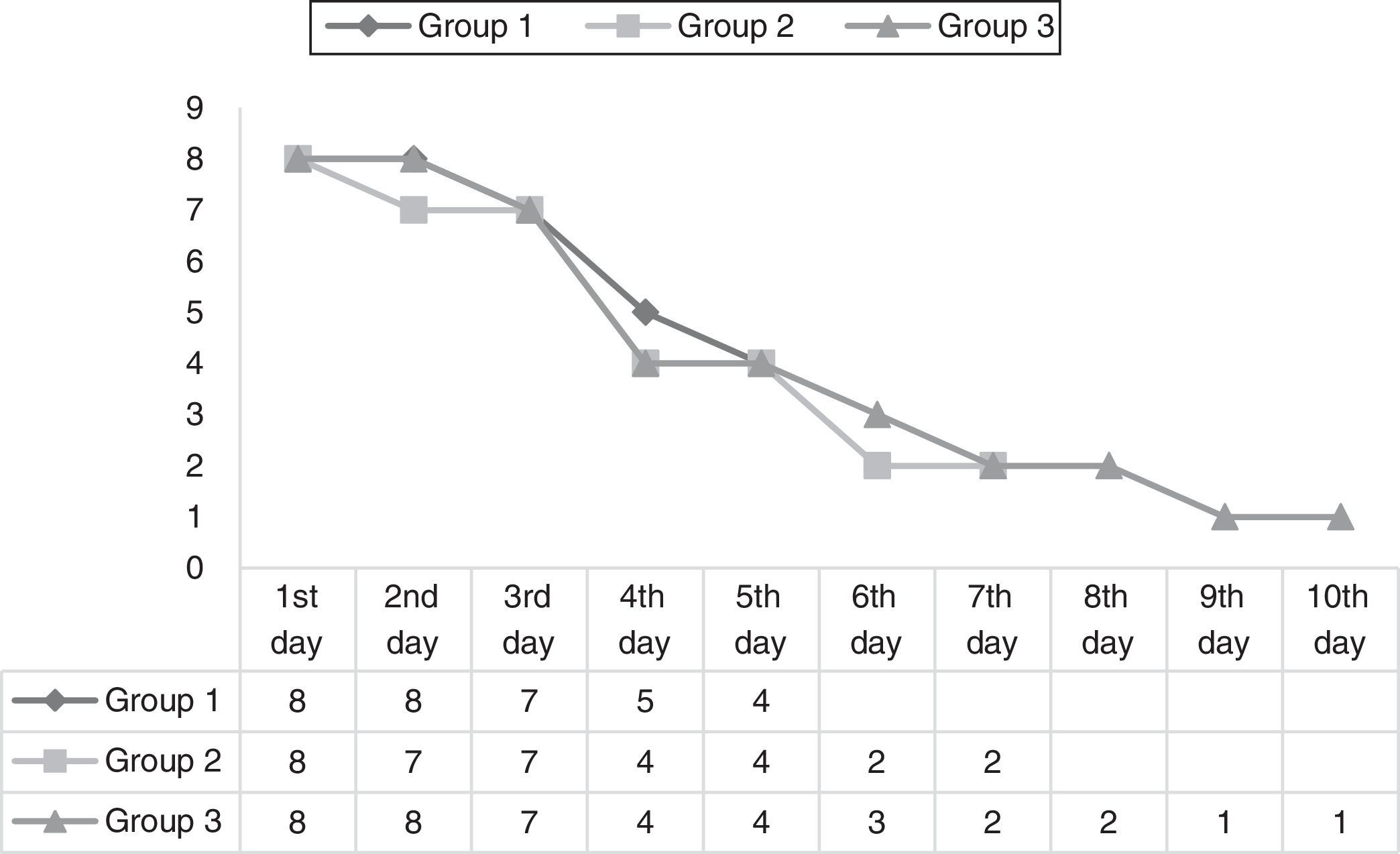
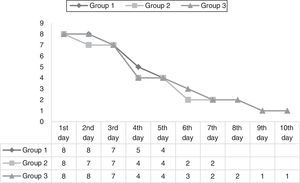
Patient discomfortIn all groups, the mean pain VAS scores were higher in the first three days than in the other days. The mean pain VAS scores decreased significantly after the third day in all groups (p<0.05) (Fig. 1).
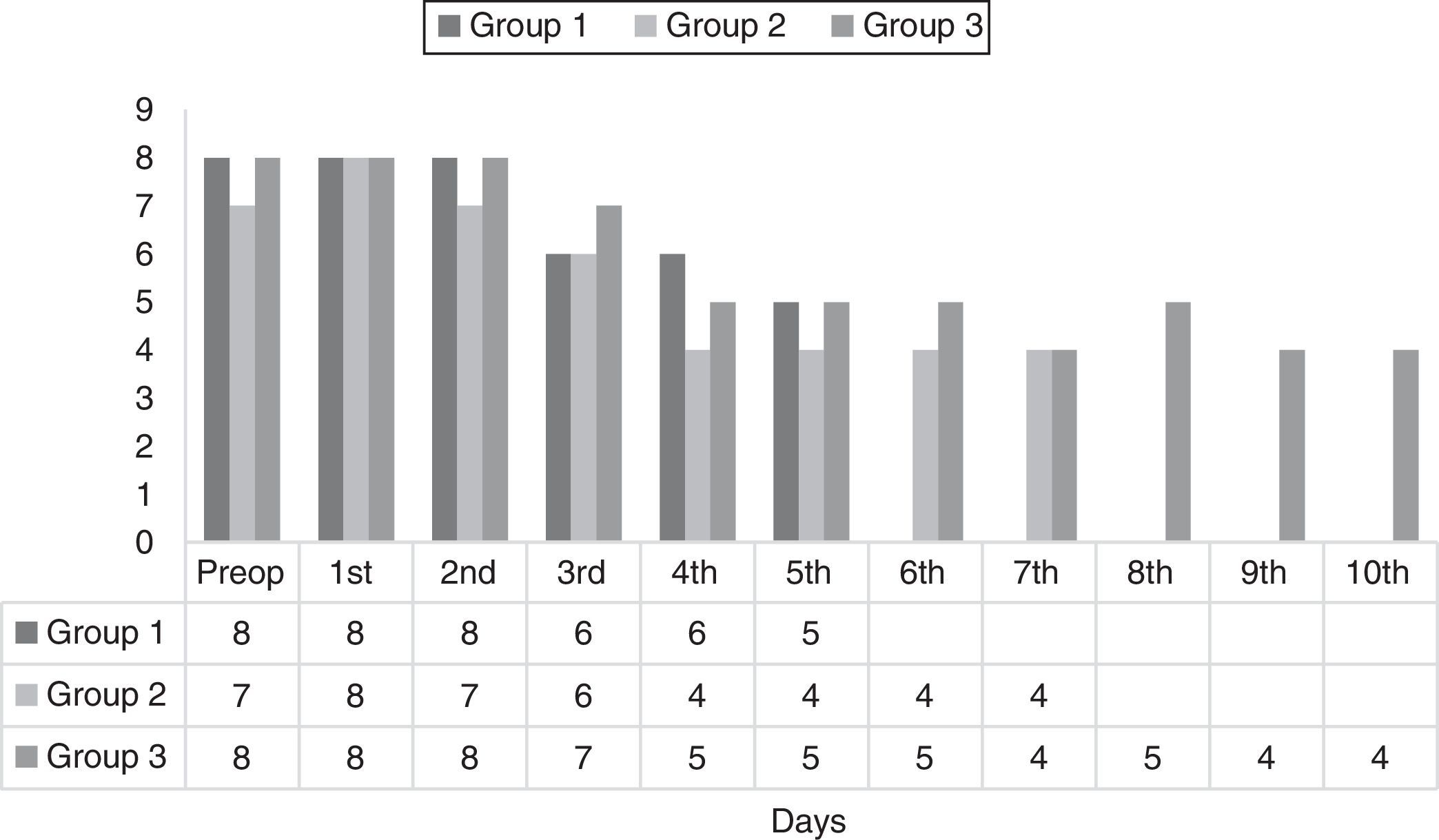
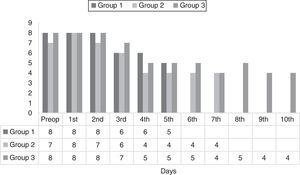
In all groups, the mean nasal obstruction VAS scores were low or similar with preoperative values for all days. Therefore, it could be suggested that there was a tolerable level of nasal obstruction for the patients (Fig. 2).
Late complicationsMucosal crusting: prolonged mucosal crusting was detected in 12 patients in Group 1, six patients in Group 2, and two patients in Group 3. The rate of mucosal crusting was decreased with prolonged intranasal splinting intervals (p=0.0105; Table 5).
Synechiae were found in six patients in Group 1, two patients in Group 2, and no synechiae were found in Group 3. The rate of synechia formation was significantly decreased with prolonged intranasal splinting intervals (p=0.0244; Table 5).
DiscussionNasal packing methods and application intervals are variable after septoplasty operations. Several surgeons do not use any nasal packing materials, preferring transseptal sutures only. Patient discomfort and local or systemic adverse reactions due to nasal packing resulted in different applications concerning the selection of packing materials, postoperative antibiotic therapies, and the duration of nasal packing. The use of antibiotics in patients with nasal packing is controversial. Nasal packing applications have been accepted as a technique that might possibly result in local and even systemic infections including Staphylococcal Toxic Shock Syndrome (STSS).5–11 Therefore, as a routine application in many clinics, oral antibiotics are continued until the tampons are removed. Recommendations for postoperative antibiotherapy are commonly found in classical textbooks.15,16 However, a number of reports have been published recently in the medical literature suggesting that postoperative antibiotherapy is unnecessary after septoplasty or rhinoplasty. Georgiou et al., in their review of antibiotic prophylaxis in rhinoplasty and septoplasty, evaluated the outcomes of 11 different studies.17 These studies confirmed that the risk of infection is very low in elective nasal operations and thus, routine antibiotic prophylaxis is unnecessary. Antibiotic prophylaxis has been recommended in cases of complicated revisions, in patients with a tendency to develop infection, and in patients in whom long-term nasal tampon applications are planned.17,18 However, although there are published reports not recommending postoperative antibiotic prophylaxis, many ENT specialists continue to prescribe oral antibiotics until the removal of the tampons.
In a study performed by the American Rhinology Association, the rate of antibiotic prescription of the surgeons after septoplasty was reported as 70%. The rationale for antibiotic use was reported as infection control in 60% of cases, prevention of toxic shock in 31.5% of cases, medico-legal purposes in 4.9% of cases, and preventing foul odors in 3.1% of cases.19 In the current study, cefdinir tablets (300mg) were administered postoperatively two times a day. We found that there were no changes in bacterial colonization properties due to splinting intervals and no infections were related to early complications. However, several pathogenic agents along with normal flora bacteria were isolated in the cultures (Tables 1–4). Therefore, we recommend that postoperative antibiotic prophylaxis should be prescribed until the removal of the nasal splints.
In their literature review, Weber et al. evaluated nasal packing materials (other than silicone splints) according to retention times and side effects. In their study, retention intervals for materials such as Merocel, paraffin gauze, gauze, fingerstalls, and silastic splints ranged from 24 to 72h.20 However, there has been no consensus in retention intervals of silicone nasal splints. In our study, we found that silicone nasal splints might be retained intranasally up to 10 days without increasing infection-related early complication rates.
Postoperative patient discomfort and late complications were the other two criteria which were evaluated in the present study. In the literature, facial pain, headaches, nasal obstruction, xerostomia, and dysphagia due to nasal obstruction are major parameters in the assessment of postoperative patient discomfort.21,22
In our study, postoperative pain scores were higher in the first three days and decreased significantly after the fourth day. Splint usage intervals did not have any increasing effect on the pain scores. With the use of analgesics, pain complaints were sustained at a reasonable level.
Preoperative and postoperative nasal obstruction scores were comparable and VAS scores measured during the use of silicone splints were similar to preoperative values or lower. Therefore, nasal obstruction due to silicone nasal splints was considered acceptable. When the effect of splint usage intervals on pain and nasal obstruction scores was evaluated, long-term use of nasal splints was easily tolerated by the patients and did not have a serious negative effect on patient comfort.
Prolonged mucosal crusting and synechia are two late complications after septoplasty that can obstruct nasal airflow. We found that the longer splint usage interval resulted in decreased mucosal crusting and synechia rates. These findings correlate well with other studies suggesting that silicone splints have a positive effect on healing and epithelization by providing the durability of nasal mucosa.2,3
LimitationsNo significant changes in bacterial colonization properties due to splint usage intervals were detected and no infection-related early complications were observed in this study. However, toxic shock syndrome (TSS) is a rare but very important systemic infection that can result from nasal packing applications (silicone splints and other materials).3–11 The sample size of this study was very small for the assessment of a rare complication such as TSS; therefore, studies with larger sample sizes are needed to obtain a conclusive decision concerning STSS risk.
ConclusionThe use of silicone splints was well tolerated by patients; negative effects on the postoperative patient comfort were limited. In fact, a prolonged splint usage time interval had a reducing effect on later complications such as mucosal crusting and synechia. Long-term silicone nasal splint usage is a reliable, effective, and comfortable method for patients with excessive mucosal damage and in whom long-term stabilization of the bony and cartilaginous septum is essential.
Financial supportFinancial support was provided by the management of the Haseki Training and Research Hospital.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Karatas A, Pehlivanoglu F, Salviz M, Kuvat N, Cebi IT, Dikmen B, et al. The effects of the time of intranasal splinting on bacterial colonization, postoperative complications, and patient discomfort after septoplasty operations. Braz J Otorhinolaryngol. 2016;82:654–61.