Adenoid hypertrophy may play a role in velopharyngeal closure especially in patients with palatal abnormality; adenoidectomy may lead to velopharyngeal insufficiency and hyper nasal speech. Patients with cleft palate even after repair should not undergo adenoidectomy unless absolutely needed, and in such situations, conservative or partial adenoidectomy is performed to avoid the occurrence of velopharyngeal insufficiency. Trans-oral endoscopic adenoidectomy enables the surgeon to inspect the velopharyngeal valve during the procedure.
ObjectiveThe aim of this study was to assess the effect of transoral endoscopic partial adenoidectomy on the speech of children with repaired cleft palate.
MethodsTwenty children with repaired cleft palate underwent transoral endoscopic partial adenoidectomy to relieve their airway obstruction. The procedure was completely visualized with the use of a 70° 4mm nasal endoscope; the upper part of the adenoid was removed using adenoid curette and St. Claire Thompson forceps, while the lower part was retained to maintain the velopharyngeal competence. Preoperative and postoperative evaluation of speech was performed, subjectively by auditory perceptual assessment, and objectively by nasometric assessment.
ResultsSpeech was not adversely affected after surgery. The difference between preoperative and postoperative auditory perceptual assessment and nasalance scores for nasal and oral sentences was insignificant (p=0.231, 0.442, 0.118 respectively).
ConclusionsTransoral endoscopic partial adenoidectomy is a safe method; it does not worsen the speech of repaired cleft palate patients. It enables the surgeon to strictly inspect the velopharyngeal valve during the procedure with better determination of the adenoidal part that may contribute in velopharyngeal closure.
A hipertrofia da adenoide pode desempenhar um papel no fechamento velofaríngeo, especialmente em pacientes com anormalidade palatal; a adenoidectomia pode levar à insuficiência velofaríngea e fala hipernasal. Os pacientes com fenda palatina, mesmo após a correção, não devem ser submetidos a adenoidectomia, exceto quando absolutamente necessário e, em tais situações, a forma conservadora ou parcial é realizada para evitar a ocorrência de insuficiência velofaríngea. A adenoidectomia endoscópica transoral permite ao cirurgião inspecionar a válvula velofaríngea durante o procedimento.
ObjetivoO objetivo deste estudo foi avaliar o efeito da adenoidectomia parcial endoscópica transoral na fala de crianças submetidas à correção de fenda palatina.
MétodoUm total de 20 crianças com fenda palatina previamente corrigida, foi submetida a adenoidectomia parcial endoscópica transoral, para desobstrução das vias aéreas,. O procedimento foi completamente visualizado com o uso de um endoscópio de 4mm e ângulo de 70°; a parte superior da adenoide foi removida com uma cureta para adenoide e fórceps St. Claire Thompson, enquanto a parte inferior foi conservada para manter a competência velofaríngea. Avaliações da fala foram realizadas nos períodos pré e pós-operatório, de forma subjetiva pela avaliação perceptivo-auditiva, e objetiva pela avaliação nasométrica.
ResultadosA fala não foi prejudicada após a cirurgia. A diferença entre os escores da avaliação perceptivo-auditiva e nasalância para as sentenças nasais e orais nos períodos pré e pós-operatório foi insignificante (p=0,231, 0,442, 0,118, respectivamente).
ConclusõesA adenoidectomia parcial endoscópica transoral é um método seguro, e não piora a fala dos pacientes com fenda palatina operada. Ela permite que o cirurgião inspecione rigorosamente a válvula velofaríngea durante o procedimento, com melhor determinação da parte adenoide que pode contribuir para o fechamento velofaríngeo.
Adenoid hypertrophy is a common cause of airway obstruction in children; it may lead to mouth breathing, nasal discharge, snoring, sleep apnea, and hyponasal speech. It also contributes to the pathogenesis of rhinosinusitis and recurrent otitis media.1 However, the adenoid lies in the posterior pharyngeal wall and may act as a pad against the palate facilitating velopharyngeal closure, especially in patients with palatal abnormality. Its presence can compensate for a short or a poorly mobile palate, a condition that may follow cleft palate repair. Following adenoidectomy, compensation is eliminated and velopharyngeal insufficiency (VPI) may result.2 Therefore, patients with cleft palate – even after repair – should not undergo adenoidectomy unless absolutely necessary, and in such situations conservative or partial adenoidectomy is performed.3,4
Patients with adenoid hypertrophy may need partial adenoidectomy if they are prone to develop VPI after the operation. The procedure entails removal of the upper part that obstructs the choanae and preservation of the lower part that assists in velopharyngeal closure.2,5,6 Several methods for adenoid removal have been previously described in the literature. Adenoid curette guided by an indirect trans-oral mirror and a headlight is a simple and quick procedure that has already been in use for a long time, but the indirect visualization of the adenoidal tissue may make the surgeon unable to completely clear the choanae, especially if partial removal is the intended procedure.7 Transnasal endoscopic partial adenoidectomy has been used with the ability to clear the choanae precisely,6,8 but this method may make the surgeon unable to completely inspect the velopharyngeal valve that is usually hidden by the residual adenoidal tissue left to maintain velopharyngeal competence. The aim of this study was to assess the effect of transoral endoscopic partial adenoidectomy on the speech of children with repaired cleft palate.
MethodsTwenty patients with adenoid hypertrophy were included in this case series study. All patients have repaired cleft palate. They were 13 males and seven females; their ages ranged between 4 and 9 years with a mean age of 6 years. Eight patients had bilateral complete cleft lip and palate, seven patients had unilateral complete cleft lip and palate, and five patients had cleft soft palate. The patients were subjected to partial adenoidectomy in the period from January 2008 to July 2013. The indication for surgery was hypertrophied adenoid causing obstructive sleep apnea (OSA) that was diagnosed by polysomnography; however, sleep apnea was not the objective issue of the study. Patients who underwent secondary corrective surgery for VPI, and who presented with craniofacial anomalies, were excluded. To exclude tonsillar hypertrophy as a cause of airway obstruction, children with tonsillar size more than grade 2 on Brodsky grading scale were excluded.9 Informed consents were obtained from the parents of the patients, and the principles outlined in the Declaration of Helsinki were followed. In addition, the research protocol was approved by the research ethics committee of our institute (N-23-2008).
All patients were subjected to the following.
Otolaryngologic examinationFull ear, nose and throat, and head and neck examinations were performed. Ear examination, including tympanometry, was performed for detection of middle ear effusion, as well as oral examination to assess the condition of the palate and size of the tonsils, and to exclude any other cause of airway obstruction. Also, nasal examination was performed to exclude any other cause of nasal obstruction.
Lateral neck radiographyAn X-ray of the nasopharyngeal air column was performed. Only patients with completely obliterated nasopharyngeal air column with adenoidal tissue were included in the study.
Preoperative assessment of speechPatients underwent auditory perceptual assessment of speech (APA) and nasometric assessment. Due to the difficulty to see the velopharyngeal valve in patients with obstructed choanae caused by adenoid hypertrophy, flexible nasopharyngoscopy was not used.
Auditory perceptual assessment of speechHypernasality, nasal emission of air, and weak pressure consonants were analyzed in each patient. Parameters were graded on a five-point scale (0–4) in which 0 indicates normal and 4 indicates severe hypernasality, with a total score of 12 on the three elements. A lower score on this scale indicates less dysfunction.
Nasometric assessmentAssessment of nasalance was performed using a nasometer (Model 6200; Kay Elemetrics Corp., Lincoln Park, NJ), which provides an acoustic measure of movement of the vibrational energy through the vocal tract. Nasometric data were obtained while the patients read or repeated standardized Arabic nasal and oral sentences.
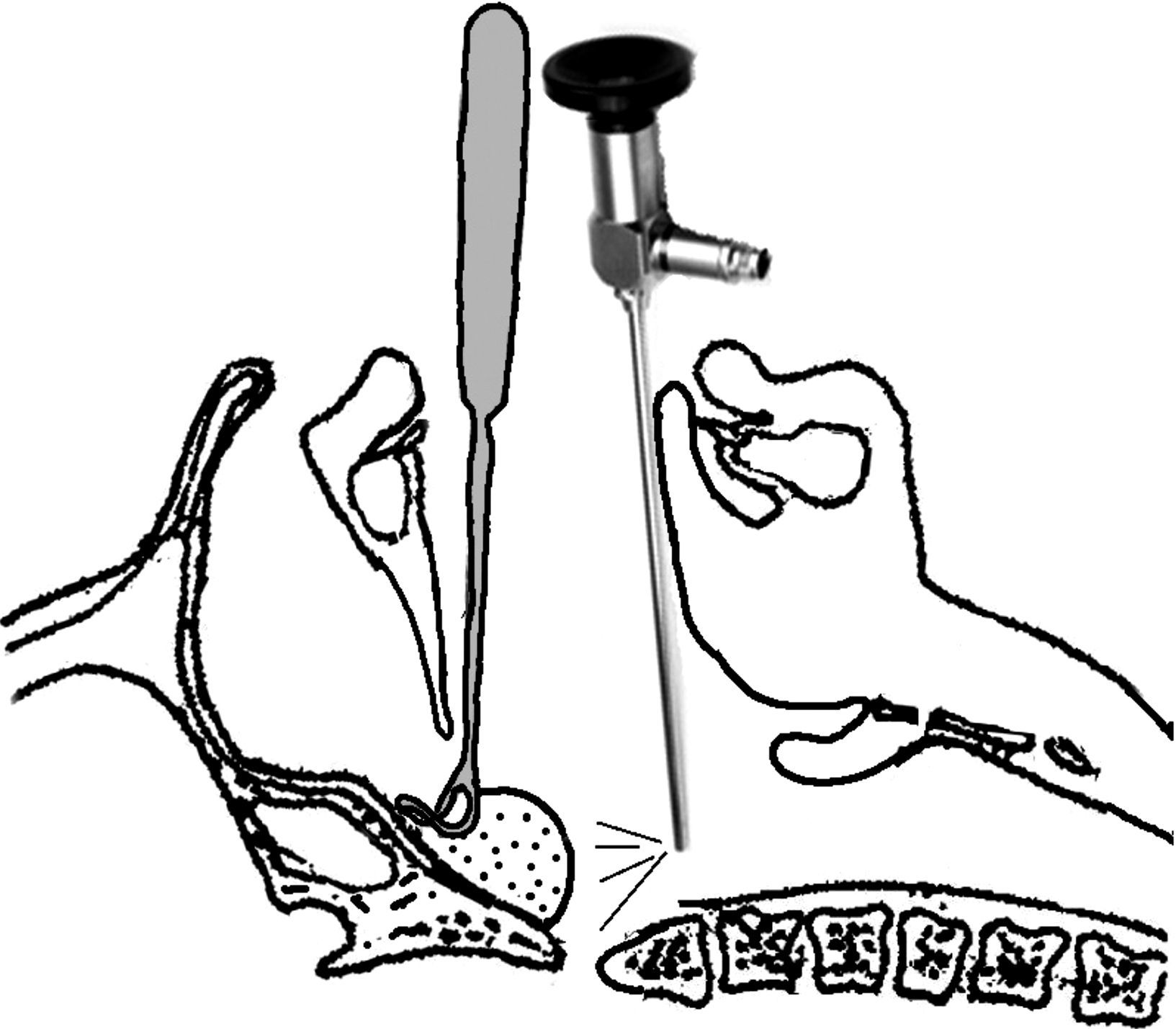
Operative procedureUnder general anesthesia with oral endotracheal intubation, a Boyle–Davis mouth gag was used to open the mouth. After retraction of the soft palate with two rubber catheters, a 70° Hopkins 4mm nasal endoscope was introduced through the mouth (Fig. 1). A camera (Karl Storz GmbH & Co KG; Tuttlingen, Germany) was mounted on the endoscope and the endoscopic view was projected on a monitor. Transoral endoscopic partial adenoidectomy was performed, in which the upper part of the adenoid was removed using adenoid curette and St. Claire Thompson forceps, while the lower part was retained to maintain the velopharyngeal competence.10 Coagulation diathermy was used for hemostasis. The technique was standardized for all patients and it was performed by the first five authors. After partial adenoidectomy and insertion of nasopharyngeal pack, patients with middle ear effusion underwent myringotomy and insertion of ventilation tubes. Upon awakening, patients were extubated and placed in the lateral position, and then transferred to the post anesthesia care unit for observation of respiration and oxygen saturation.
Postoperative assessment of velopharyngeal functionFollowing routine postoperative instructions and follow up, patients were directed to return after six months for APA and nasometric assessment using the same parameters employed preoperatively.
Statistical methodsData were coded and summarized using Statistical Package for Social Sciences version 17.0 for Windows (SPSS Inc., Chicago, IL). Quantitative variables are presented as mean±standard deviation. Comparison of preoperative and postoperative results of auditory perceptual assessment and nasometric assessment was done using paired two-sample t test. p<0.05 was considered statistically significant.
ResultsTwenty children with repaired cleft palate and adenoid hypertrophy were enrolled in the study. Partial adenoidectomy was performed to relieve the airway obstruction; the procedure was done endoscopically through the mouth under complete visualization. Middle ear effusion was detected bilaterally in six patients who were treated with myringotomy and insertion of ventilation tubes. No intraoperative or postoperative complications were encountered.
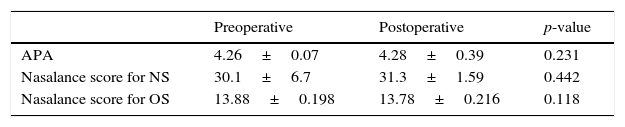
Speech was not adversely affected after surgery (Table 1). The mean preoperative baseline of auditory perceptual assessment was 4.26±0.07, whereas postoperatively it was 4.28±0.39. The difference between preoperative and postoperative scores was insignificant. Also, nasalance was not worsened after surgery. The preoperative scores were 30.1±6.7 for the nasal sentences and 13.88±0.198 for the oral sentences, whereas postoperative scores were 31.3±1.59 for the nasal sentences and 13.78±0.216 for the oral sentences. The changes were statistically insignificant for both nasal and oral sentences.
Pre- and postoperative assessment of speech parameters.
| Preoperative | Postoperative | p-value | |
|---|---|---|---|
| APA | 4.26±0.07 | 4.28±0.39 | 0.231 |
| Nasalance score for NS | 30.1±6.7 | 31.3±1.59 | 0.442 |
| Nasalance score for OS | 13.88±0.198 | 13.78±0.216 | 0.118 |
APA, auditory perceptual assessment; NS, nasal sentences; OS, oral sentences.
Patients with cleft palate may have narrow airway space when compared with non-cleft palate patients, although there are no differences in the size of the tonsils and adenoids between both groups.11 After palatoplasty, the narrowing is increased, which may lead to OSA in some patients.12,13 However, conventional adenoidectomy is contraindicated in cleft palate patients even after repair, as it may lead to VPI, with consequent hypernasal speech. Hypertrophied adenoidal tissue may facilitate velopharyngeal closure especially in patients with palatal abnormalities, and its removal may uncover the problem.2,3 To avoid postoperative VPI in those patients, partial adenoidectomy is recommended, in which the upper part that obstructs the choanae is removed, and the lower part that may share in velopharyngeal closure is retained.2,8
Many authors have discussed partial adenoidectomy in submucous cleft palate patients.4–6 A condition that is characterized by deficiency of muscles in the midline of the soft palate, it leaves a central gap on velopharyngeal closure. In patients with adenoid hypertrophy, the disease is usually asymptomatic, as the gap may be occupied by the adenoidal tissue. So, partial adenoidectomy is recommended for adenoid hypertrophy of those patients.6,8 Although patients with repaired cleft palate are prone to develop post-adenoidectomy VPI, little is mentioned in the literature about partial adenoidectomy after cleft palate repair. The palatal muscles of the cleft palate patients are usually hypoplastic and weaker than normal, a problem that is not corrected by repair.2,4 For this reason, the adenoid hypertrophy of repaired cleft palate patients should be managed like those of patients with submucous cleft palate.
This study was conducted on 20 children with repaired cleft palate and adenoid hypertrophy; transoral endoscopic partial adenoidectomy was performed. The procedure was completely visualized with strict inspection of the velopharyngeal valve. The choanae were cleared out of adenoidal tissues to ensure a patent airway, while the lower part of the adenoid was retained to avoid disruption of the velopharyngeal valve. Auditory perceptual assessment and nasometric assessment were performed pre and postoperatively by the last author; there were no significant changes in both parameters. Flexible nasopharyngoscopy was not performed in the assessment of velopharyngeal function, as the choanae were completely obstructed by adenoid that is seen radiologically, so it would be difficult to perform the maneuver in awake patients who should repeat oral consonants to see the velopharyngeal closure.
Endoscopic partial adenoidectomy for patients who are prone to develop postoperative VPI is a good technique as it helps the surgeon to accomplish his goal, which is relief of nasal obstruction without disruption of the velopharyngeal valve. It was performed transnasally, using the 4mm 0° nasal endoscope, and the adenoidal tissues were removed by a cutting forceps.6,8 However, our patients underwent the procedure transorally, using the 4mm 70° nasal endoscope, and the adenoidal tissue was removed by adenoid curette and St. Claire Thompson forceps. The surgical field is wider with transoral than with the transnasal approach, so our technique facilitates easy clearance of the choanae with good hemostasis if needed and strict inspection of the velopharyngeal valve. In addition, trans-oral adenoidectomy is more familiar to the otolaryngologists.
Transnasal endoscopic partial adenoidectomy has been performed for patients with submucous cleft palate by Finkelstein et al.6; relief of nasal obstruction was achieved in all patients, but two out of ten demonstrated mild hypernasality postoperatively. The development of hypernasality may be attributed to the inability of the surgeon to inspect the velopharyngeal valve transnasally during the procedure, as the valve may be hidden by the retained lower part of the adenoid, with difficulty to freely manipulate the rigid endoscope. However, Stern et al.8 used the same maneuver, and none of their patients developed postoperative VPI. Kakani et al.14 used a St. Clair adenoid forceps for removal of adenoid in patients with palatal abnormality, under indirect vision with a laryngeal mirror. All patients experienced a complete or near-complete resolution of their nasal obstruction, and none developed permanent VPI. Also, Tweedie et al.4 performed transoral partial adenoidectomy using a malleable suction coagulator under indirect vision. They achieved complete relief of nasal obstruction without worsening of patients’ speech. Our method enables the surgeon to completely visualize the whole procedure, and consequently to determine precisely how much adenoidal tissue is needed to be removed, to perform better hemostasis, and to avoid injury of the velopharyngeal area.
It is worth mentioning that we did not use flexible nasopharyngoscopy in the assessment of velopharyngeal function, as our patients had completely obstructed choanae by the hypertrophied adenoidal tissue. Also, we did not present OSA data, because the objective of the study was to assess the effect of partial adenoidectomy on velopharyngeal function. For a strong statistical impact, the study should be applied on a large sample of patients. However, adenoid hypertrophy in patients with repaired cleft palate is not common, so we recommend a larger multicenter study.
ConclusionTransoral endoscopic partial adenoidectomy is a safe method; it does not worsen the speech of repaired cleft palate patients. It enables the surgeon to strictly inspect the velopharyngeal valve during the procedure with better determination of the adenoidal part that may contribute in velopharyngeal closure.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Abdel-Aziz M, Khalifa B, Shawky A, Rashed M, Naguib N, Abdel-Hameed A. Trans-oral endoscopic partial adenoidectomy does not worsen the speech after cleft palate repair. Braz J Otorhinolaryngol. 2016;82:422–6.