Transcanal myringoplasty has the advantages of demanding lower operative time and minimal external incisions. It can be performed using the microscopic or endoscopic approach. In the last decade, the use of endoscopes in ear surgery has increased significantly. This technique may allow “around the corner” visualization of small recesses, through narrow spaces, without the aid of canalplasty in unfavorable ear canals.
ObjectiveTo describe a case series of transcanal endoscopic myringoplasty performed in a university service. The characteristics, advantages, and disadvantages of this technique are also discussed.
MethodsA case series study, based on the chart review of patients submitted to transcanal endoscopic myringoplasty in the period from January of 2012 to October of 2014.
ResultsData from 22 patients were analyzed. Tympanic perforation closure three months after surgery was observed in 86.4% of all patients. There was statistically significant improvement in pure tone average thresholds after surgery (p<0.001).
ConclusionTranscanal endoscopic myringoplasty is a feasible, safe, and effective procedure; it can be an alternative to microscopic surgery.
A miringoplastia realizada por via transcanal possui como vantagens a maior rapidez do procedimento e menor incisão externa, podendo ser realizada com auxílio de microscópio ou endoscópio. Na última década tem sido observado um aumento do uso de endoscópios na cirurgia otológica. Essa técnica pode permitir melhor visibilização de espaços encobertos e estreitos, sem necessidade canaloplastia em meatos desfavoráveis.
ObjetivoDescrever uma série de casos de miringoplastia endoscópica transcanal, em um serviço universitário, discutindo suas particularidades, vantagens e desvantagens.
MétodoEstudo de série de casos, baseado na revisão de prontuários dos pacientes submetidos a miringoplastia com uso exclusivo de endoscópio rígido, no período de Janeiro de 2012 a Outubro de 2014.
ResultadosForam analisados os dados de 22 pacientes. Na otoscopia pós-operatória, foi observado fechamento da perfuração timpânica em 86,4% dos pacientes, após 3 meses da intervenção. Para a amostra estudada, foi observada melhora funcional estatisticamente significante da média dos limiares tonais (PTA) após a cirurgia (p<0,001).
ConclusãoA miringoplastia endoscópica transcanal é um procedimento seguro, factível e efetivo, podendo ser realizado como alternativa à cirurgia microscópica.
Myringoplasty (tympanoplasty type I) is usually the treatment of choice for tympanic perforations, whether or not associated with non-suppurative chronic otitis media (COM).1,2 The surgical goal is the total closure of the perforation and, secondly, an improvement of auditory thresholds.2,3 Transcanal myringoplasty has advantages: it demands lower operative time and minimal external incision.2,3 When performed with the aid of a surgical microscope, the transcanal procedure depends on a wide external auditory canal (EAC) and on a favorable angle for proper observation of all borders of the tympanic perforation.3 Conventional myringoplasty with retroauricular incision, with or without canalplasty, is the classic alternative for cases of unfavorable EAC in transcanal approaches with microscope.
In the last decade, there has been an increase in the use of endoscopes in otologic surgery, not just as an adjunct method, but exclusively.3,4 This approach has the potential to allow “around the corner” visualization of small recesses, through narrow spaces, without the need for canalplasty, even in cases of unfavorable EAC.5,6
The teaching of otologic surgeries during the otolaryngologist's training period is traditionally done with the use of microscopes. Despite recent reports of several authors, who describe the performance of myringoplasty with the use of optical fiber,3,5 there is a scarcity of studies in Brazil assessing the results of endoscopic techniques in the context of university hospitals.
The aim of this study is to describe a case series of transcanal myringoplasty using a rigid endoscope, evaluating surgical outcomes in a university service. Aspects specifically associated with the use of endoscopes in otology and particularities related to surgical teaching will be further discussed.
MethodsA case series, cross-sectional historical cohort study was conducted, based on the analysis of medical records of patients submitted to myringoplasty with exclusive use of rigid endoscope in a university service with a medical residency program in otorhinolaryngology from January 2012 to October 2014.
All patients older than 12 years with a diagnosis of non-suppurative, non-cholesteatomatous COM sequela, or with traumatic perforations without spontaneous resolution for more than three months, were included in the study. The diagnosis was based on anamnesis, physical examination, audiometry, and impedance audiometry.
Medical records with incomplete data, without pre- and/or postoperative audiometry, and patients lost to follow-up were excluded from the study.
The surgeries were performed under hypotensive general anesthesia, with patients placed in the conventional position for otologic surgery performed with a microscope. Surgical procedures were performed by resident physicians of the third year and/or graduate students of the otorhinolaryngology department of the service.
Before surgery, patients were informed about the possible need for surgical conversion to retroauricular access. For the procedure, a rack containing a Storz Telecam SL-NTSC camera (Karl Storz GmbH & Co. KG – Tuttlingen, Germany), connected to a Sony Trinitron PVM-20M2DE monitor (Sony Corp. of America – New York, United States), was positioned in front of the surgeon. The technique and the surgical instruments used were the same as in routine surgeries with microscope, except for the non-use of the microscope and otologic speculum, and the use of the Storz rigid endoscopes, 4-mm diameter and 18-cm long, at 0˚ angulation (Karl Storz GmbH & Co. KG – Tuttlingen, Germany).
Cotton pads soaked in epinephrine 1:1000 were placed in the EAC in case of bleeding that would make operative field visualization difficult. Regardless of which was the surgeon's dominant hand or the laterality of the ear to be operated upon, the rigid endoscope was used with the non-dominant hand and the instruments (stylus, delicate tissue forceps, and suction cannulas) in the dominant hand.
In all cases, the procedure was performed by transcanal endoscopic approach. The tympanic reconstruction technique used was inlay tragus cartilage myringoplasty, previously described by other authors,7,8 but adapted for exclusive endoscopic approach.
Initially, the perforation borders were scarified with a straight and/or curved tip stylus. Then, the perforation size was measured for correct preparation of the cartilage graft. A tragus fragment was obtained, maintaining the perichondrium of both sides of the cartilage. After measurement, the cartilage was shaped and incised around its perimeter to create a groove allowing the graft fitting into the perforation. The graft was then positioned and the perforation was closed.
Prophylactic postoperative antibiotic therapy was prescribed to all patients, using first-generation cephalosporin (cephalexin or cefadroxil), for seven days. The patients were discharged on the day after the procedure and followed at regular outpatient follow-up.
The following data were collected and analyzed: age, gender, pre- and postoperative audiometry, and pure tone average (PTA) thresholds at 500, 1000, and 2000Hz. Patients were examined at one, four, and 12 weeks postoperatively, and the incorporation (or not) of the graft and/or the presence of residual perforation were observed. The final postoperative audiometry was carried out between two and three months after the procedure.
Statistical analyses were performed using SPSS v. 17, Minitab v. 16, and Excel Office 2010. Non-parametric tests were used due to the small sample size (<30 individuals). The hypothesis tests utilized in this study considered a significance of 5%, i.e., the null hypothesis was rejected when the p-value was ≤0.05.
The project was submitted to and approved by the Research Ethics Committee of the institution of origin, under No. 936.194 (CAAE 40682114.7.0000.5505).
ResultsDuring the study period, 22 patients were assessed. The mean age of patients was 32.2±6.0 years. Thirteen (59.1%) patients were females and nine (40.1%) were males. As for the laterality, in 13 (59.0%) patients the perforation was located on the left, in eight (36.3%) patients the perforation was located on the right, and one (4.5%) patient had bilateral perforations.
Most patients were undergoing surgery for the first time; patients undergoing reoperation accounted for 9.1% of cases (n=2). There were no cases that required surgical conversion to retroauricular approach or use of the microscope in this series.
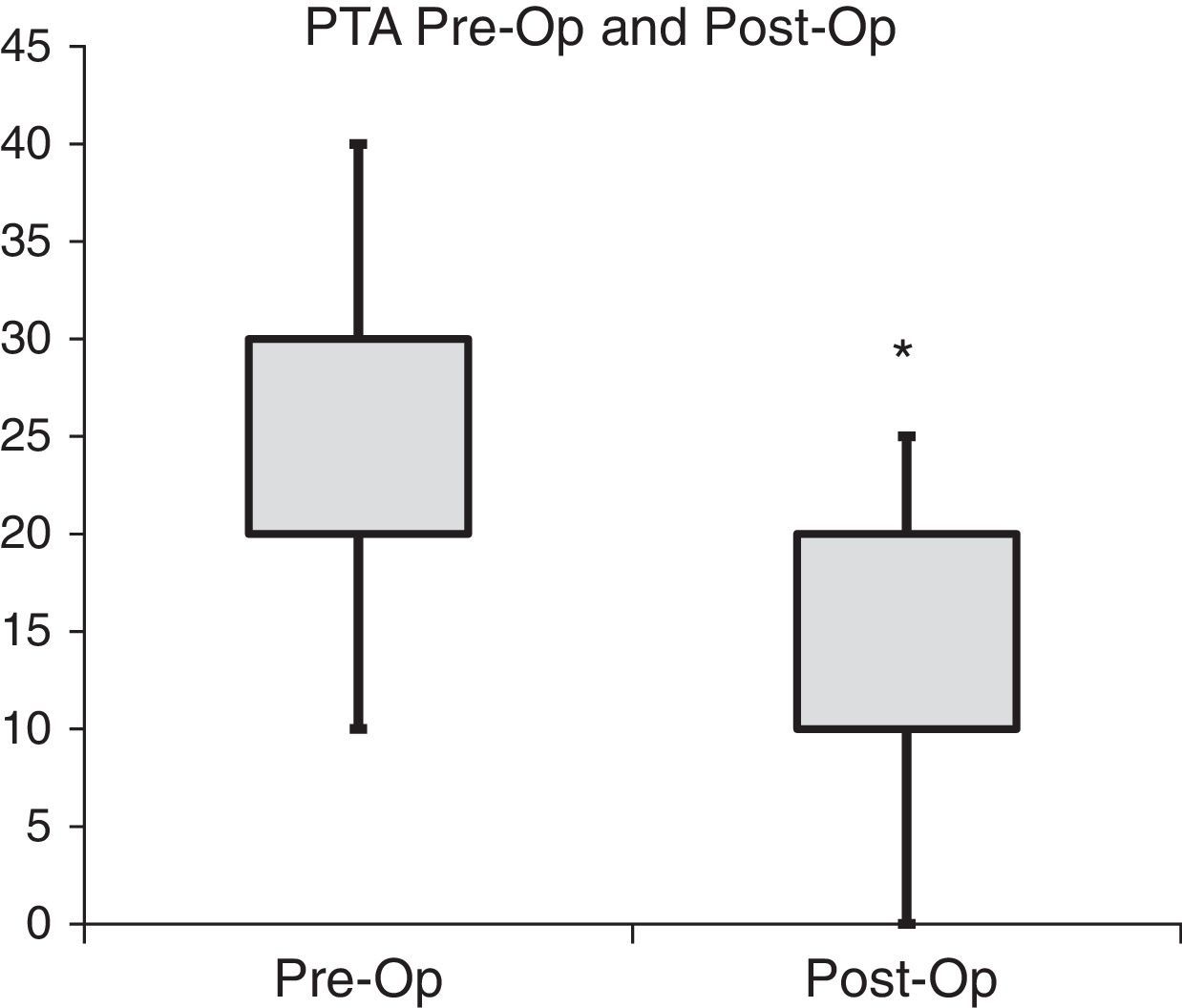
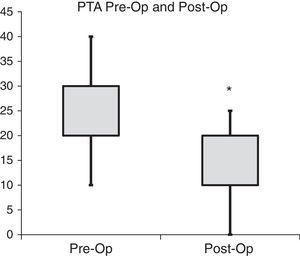
Audiometrically, an improvement in the pure tone average (PTA) hearing thresholds was observed from the preoperative to the postoperative period (Table 1 and Fig. 1). This difference was statistically significant (p<0.001). One of the patients had pre and postoperative anacusis; this subject was excluded from PTA calculation (n=21).
Descriptive comparison between pre- and postoperative PTA values.
| PTA | Pre | Post |
|---|---|---|
| Mean (dB) | 23.3 | 13.6 |
| Median (dB) | 20.0 | 10.0 |
| Standard deviation | 7.6 | 7.1 |
| Minimum (dB) | 10 | 0 |
| Maximum (dB) | 40 | 25 |
| n | 21 | 21 |
| p-Value | <0.001a |
PTA, pure tone average – average auditory thresholds at 500, 1000, and 2000Hz; Pre, pre-operative PTA; Post, post-operative PTA.
As for the surgical outcome at postoperative otoscopy, complete closure of the perforation was observed in 86.4% (n=19) of patients three months after intervention.
DiscussionThe present study assessed the feasibility and surgical outcomes of 22 transcanal endoscopic myringoplasty procedures using tragus cartilage, in a university service with a residency program in otorhinolaryngology. The procedure proved to be a possible alternative to myringoplasty under microscopic visualization, considering the surgical results (perforation closure) and the proportion of audiometric improvement at three months of follow-up.
COM is a heterogeneous disease, with a wide, varied clinical and pathological spectrum. This heterogeneity is apparently determined by the combination of different cytokines and inflammatory mediators.9 In non-suppurative, non-cholesteatomatous COM, also called “simple COM”, the inflammatory process in the tympanic cavity is minimal or absent.9 Therefore, it is important to note that surgical outcomes tend to be good, regardless of the surgical technique employed, and are not dramatically affected by changes in the surgical visualization mode, providing the basic technical principles are maintained. In fact, studies show that hearing threshold improvement after myringoplasty essentially depends on graft incorporation to the tympanic membrane, the integrity of the ossicular chain, the absence of residual perforation, and graft lateralization or medialization. Therefore, the approach, whether it is the traditional microscopic or the endoscopic method, would have little influence on functional and surgical outcomes.10
For decades the use of endoscopes in otology was primarily for anatomical studies of the middle ear and use in humans was limited, to simple observations of the tympanic cavity from pre-existing perforations or as an adjunctive method to aid traditional microscopic procedures.4,11 However, in the last two decades it has been used as an exclusive technique for otologic surgery in procedures classically performed only with a microscope including: myringoplasties, ossiculoplasties, stapedotomies, and surgeries to treat COM.11–13 The exploration of covered recesses, which are difficult to visualize microscopically – such as the tympanic sinus, the protympanum, and the anterior epitympanic recess – is facilitated by the use of endoscope.4,14
In a study comparing endoscopic with microscopic myringoplasty, Dündar et al. evaluated 60 pediatric patients undergoing type 1 tympanoplasty using a condro-perichondral graft, reporting a decrease in the air-bone gap in both groups and graft incorporation rate of 87.5% (28 of 32 patients in the endoscopic group).15 This rate is similar to that found in the present study (86.4%). The same authors found no statistically significant differences between the groups regarding the audiometric gain and/or graft incorporation. However, a shorter operative time was reported with the use of the endoscope.15 Ayache et al., in turn, reported a success rate of 96% for cartilage graft incorporation, placed with the aid of the rigid endoscope, considering the procedure as minimally invasive, safe, and effective.3
The microscope characteristically allows a broad and excellent image quality, with a direct and stereoscopic visualization.10 However, there are inherent limitations to the equipment, such as: decrease of brightness proportional to the magnification; limitation of the surgical field-of-view, especially in narrow spaces such as the EAC and the middle ear. Endoscopes, in turn, provide in-depth images in narrow recesses, while maintaining brightness and allowing different visualization angles.6
Disadvantages associated with the endoscope involve working with only one hand and the absence of stereoscopic view, which many authors consider crucial for otologic surgery.4,6,11,14 Other criticisms of endoscope use in otologic surgery refer to the delicate nature of the surrounding structures, with potential risk of mechanical and thermal trauma, and the space conflict in the surgical field between optical fiber and the surgical instrument. The learning curve is another determining factor of surgical outcomes with the use of endoscopes, as observed in sinonasal and skull base surgery.16
This study has the intention to describe the initial surgical outcomes of a university service with a residency program in relation to a new technique in otology. However, there are limitations. Due to materials unavailability, the 4-mm diameter, 0° angle, 18-cm long endoscope (usually used in sinonasal endoscopic surgery) was the only one used. Unfortunately, it was not possible to use optical fibers of different angles, diameters, and/or lengths for comparisons of easy handling of the instrumental and visualization of the surgical field.
There was no need for surgical conversion to the retroauricular approach or microscope use, or other intraoperative complications in any of the studied cases. However, further studies with larger samples of patients are needed for proper comparison of these two tympanic membrane reconstruction techniques.
ConclusionTranscanal endoscopic myringoplasty is a safe and feasible procedure, with good success rates for tympanic perforation closure and recovery of hearing thresholds. It can be performed and taught in academic services with a residency program in otorhinolaryngology, in addition to conventional surgery using a microscope.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Garcia LB, Moussalem GF, de Andrade JSC, Mangussi-Gomes J, Cruz OLM, Penido NO, et al. Transcanal endoscopic myringoplasty: a case series in a university center. Braz J Otorhinolaryngol. 2016;82:321–5.