Pyriform sinus fistula (PSF) is a rare congenital disease that causes neck abscess and/or suppurative thyroiditis.1 Complete excision of the fistula is the most common treatment.2 However, in the last decade, endoscopic cauterization of the opening of the fistula has been reported as a minimally invasive surgery for PSF.3,4 Although some studies have suggested that the latter option is reliable and minimally invasive, it requires repetitive procedures in some cases.4 Moreover, two cases with temporal complications in the postoperative course have been reported.5 Thus, it is worth seeking another option that is both safe and effective for treating PSF. This case report details two patients who underwent successful suture closure of the sinus opening of the PSF to reduce the risk of complications and neck infection.
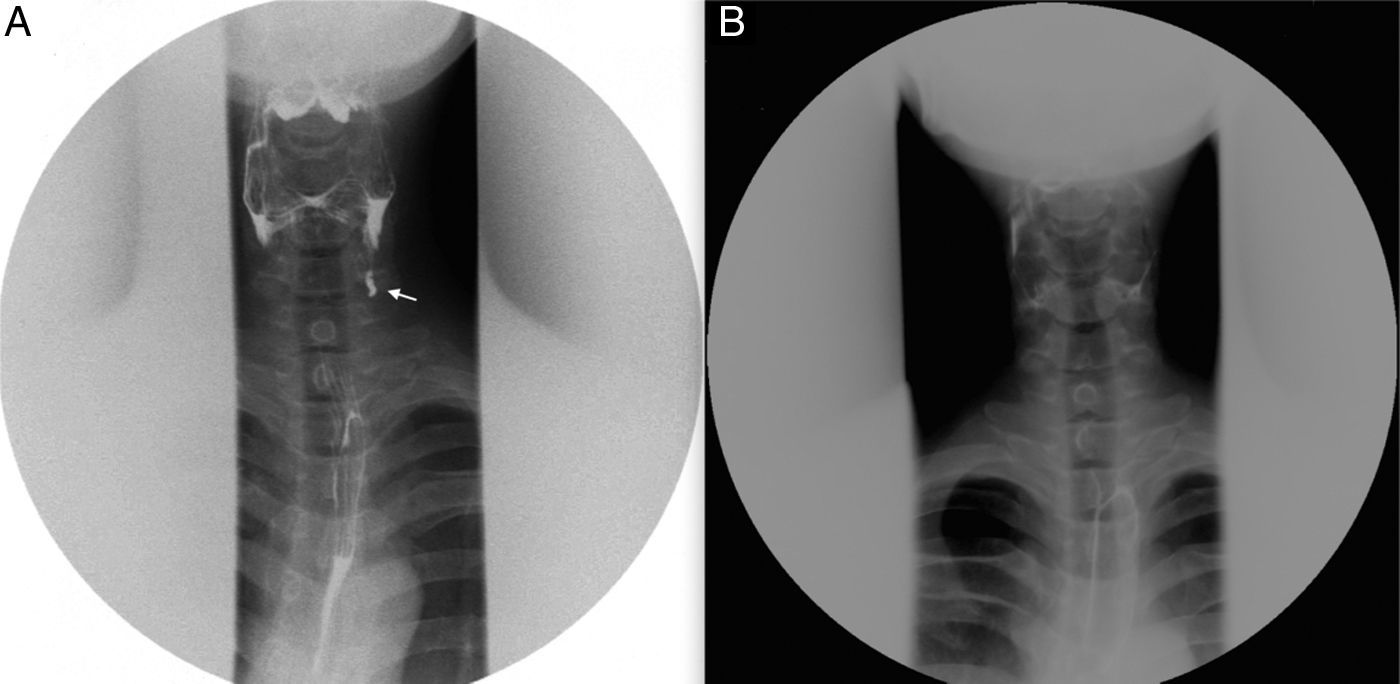
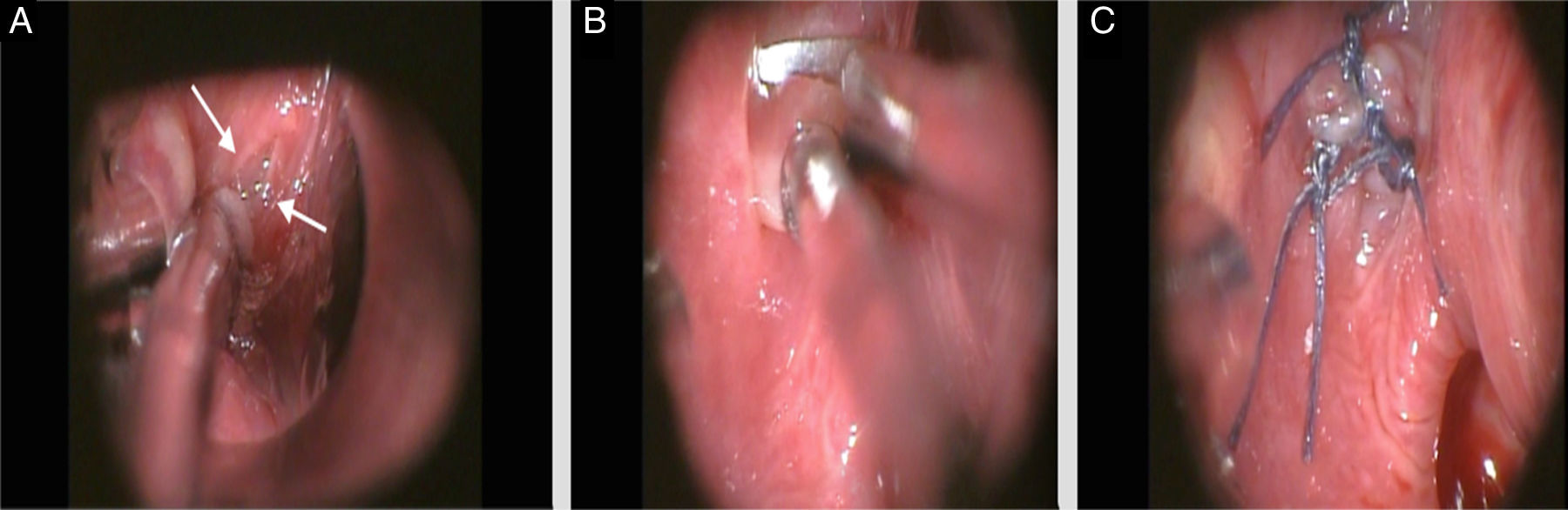
Case reportsCase 1A 26 year-old man complaining of neck pain in the left side visited this institution. He had experienced a neck abscess in the left side approximately ten years earlier. The cause of the previous neck abscess was diagnosed as an infection of the PSF in another institution. The pain disappeared after five days of antibiotics administration. Esophagography was performed two months after disappearance of the pain and revealed a left-sided PSF (Fig. 1A). Surgery was performed under general anesthesia, as follows: the procedure began with identification of the fistula opening in the left pyriform fossa through direct laryngoscopy. The fistula opening was found adjacent to the esophageal orifice (Fig. 2A). Subsequently, after being pulled out with a grasper forceps, the internal surface of the fistula was partially resected to make a fresh wound (Fig. 2B). The wound was sutured with 5-0 Vicryl polydioxanone suture (Ethicon – United States; Fig. 2C). In the postoperative course, the patient started food intake the day after surgery. The esophagography revealed no fistula two months after the surgery (Fig. 1B).
Two years after the surgery, no complication or infection in the neck was observed.
Case 2A 9 year-old girl had experienced a lower neck abscess with upper respiratory infection every two years. Suspecting the presence of a PSF, esophagography was performed, which revealed a fistula in the left pyriform sinus. The same surgical procedure and postoperative management applied to Case 1 were applied for this patient. No fistula was observed upon esophagography one month after the surgery. One year after the surgery, no complication or abscess was observed, though the fistula tract was palpable on neck examination.
DiscussionThe clinical courses of these two cases raise two important points. First, suture closure of the opening of the sinus fistula represents an alternative, less invasive, safe endoscopic surgery as a treatment option for patients with PSF. Second, the opening of the fistula may be the main gate of neck infection among these patients.
Suture closure of the opening of the sinus fistula can be considered as an alternative endoscopic surgery for patients with PSF, and is both safe and simple. Surgical excision of the whole fistula tract has been typically chosen as the first-line treatment. However, it is accompanied with an unavoidable surgical neck scar and the risk of nerve injury.2 Contrastingly, chemocauterization of the opening of the fistula through a laryngoscope has been reported as a minimally invasive treatment option.4 Although the endoscopic procedure can avoid the surgical neck scar, two previously reported cases showed vocal fold immobility after the operation.5 It is possible that trichloroacetic acid, which was used for chemocauterization in this previous report, might affect the recurrent laryngeal nerve, which was adjacent to the fistulae.5 Moreover, their methods required repeated procedures in two of 16 patients, because it failed to obliterate the internal opening of the fistula.5 In the present two cases, the opening of the fistula was sutured through direct laryngoscopy, without manipulating the deeper fistula tract. The authors believe that this method can close the opening of the fistula more certainly and safely than chemocauterization of the PSF. Kamide et al. proposed another endoscopic surgical procedure that resects the PSF tract using transoral videolaryngoscopy.6 The possibility of complete resection of the fistula tract is a major advantage of their method. However, it requires special machine settings and techniques. On the other hand, the authors’ endoscopic surgery can be performed using conventional tools and simple techniques.
The other point to consider is that the opening of the fistula may be the main gate of neck infection among patients with PSF. In the present two cases, the frequency of neck infection decreased by closing the opening of the fistula through direct laryngoscopy, even though a residual tract still exists after the surgery. Two previous reports described the treatment benefit of endoscopic cauterization of the internal opening of PSF; the success rates of prevention for neck infection were reported by Cha et al. and Kim et al. as 34/44 and 12/16, respectively.3,4 Kim et al. assumed that the cause of neck infection was contamination from pharyngeal secretions,4 and the clinical courses of the two present cases support this assumption. Considering these previous reports and the present cases, the authors believe that the key to controlling the infection of the PSF is to shut the main gate of infection, i.e., the opening of the sinus fistula.
This method has one major limitation, which is the risk of recurrence of infection from the residual fistula tract. Although neither neck abscess nor thyroiditis was found after the procedure in the present cases, the risk should not be ignored. In that situation, complete resection of the residual tract would work as a second-line treatment. In fact, Kim et al. reported that four of 16 patients who had undergone chemocauterization for PSF showed recurrence of the neck abscess.4 In some reports, complete fistulectomy could be performed for patients with PSF showing recurrent neck infection after chemocauterization.4,7
ConclusionSuture closure of the opening of the pyriform sinus fistula may represent an alternative treatment option as an endoscopic procedure for patients with PSF. This approach can decrease the risk of neck infection by closing the infectious route.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Matsuzaki H, Makiyama K, Suzuki H, Ohshima T. Prevention of neck infection by endoscopic suture closure of pyriform sinus fistulae: a report of two cases. Braz J Otorhinolaryngol. 2018;84:257–9.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.