An ongoing discussion is found in medical literature about the reasons for changes in thyroid carcinoma incidence patterns over the last decades.
ObjectiveTo analyze the clinical and pathological characteristics of thyroid carcinoma cases over a decade.
MethodsCross-sectional study over an historical cohort. Medical records of 628 thyroid cancer cases in a single center were reviewed. 597 patients were included. Microcarcinoma cases were selected for a qualitative analysis phase, in which medical records were reviewed for better understanding of thyroid nodule and thyroid cancer diagnosis process.
ResultsAn increase in the proportion of cases with thyroid cancer diagnosis was observed throughout the decade; new cases were predominantly tumors of less than 2cm, with histopathological signs of low aggressiveness. There was an increase in proportion of cases with malignant cytological results among microcarcinomas.
ConclusionThere is a trend for increase in thyroidectomies due to cancer in this institution, with proportional increment of cases with histopathological characteristics indicative of early disease. Among microcarcinomas, there is an increasing group represented by cancer cases that were not incidentally diagnosed, related to an enhancement in preoperative diagnostic methods.
Persiste uma discussão na literatura sobre as razões para as mudanças no padrão de incidência do carcinoma de tireoide nas últimas décadas.
ObjetivoAnalisar as características clinicopatológicas dos casos de carcinoma de tireoide ao longo de uma década.
MétodoEstudo transversal sobre uma coorte histórica. Os registros médicos de 628 casos de câncer de tireoide de um único centro foram revisados. Foram incluídos 597 pacientes. Os casos de microcarcinoma foram selecionados para uma fase de análise qualitativa, na qual os registros médicos foram revisados para melhor entendimento do processo de diagnóstico do nódulo e do câncer.
ResultadosObservamos um aumento na proporção de casos com diagnóstico de câncer de tireoide ao longo da década; os novos casos foram predominantemente de tumores <2 cm, com sinais histopatológicos de baixa agressividade. Houve aumento na proporção de casos com resultado citológico maligno entre os microcarcinomas.
ConclusãoHá uma tendência de crescimento nas tireoidectomias por câncer na nossa instituição, com incremento proporcional de casos com características histopatológicas indicativas de doença precoce. Entre os microcarcinomas, há um grupo em ascensão representado por casos com diagnóstico não-ocasional de câncer, relacionados à melhora dos métodos diagnósticos pré-operatórios.
By far, thyroid carcinoma is the most common type of endocrine cancer.1,2 Papillary carcinoma (PC) is the most common subtype of thyroid carcinoma. Although malignant neoplasms of the thyroid correspond to only 1% of all cancers and to 0.5% of all deaths caused by cancer in the world,3,4 autopsy studies have shown that PC is extremely common and underdiagnosed. One of the best-conducted studies from a methodological point of view was that by Harack et al. In their paper, these authors analyzed 101 glands sectioned at 2–3mm intervals. Neoplastic foci were found in 36% of cases, all in individuals with no prior knowledge of thyroid pathology. In most cases the tumors were represented by small microcarcinomas, and many others may have been lost, solely due to the predetermined interval section.5
Although thyroid PC is a disease of low mortality,6,7 it still remains a cause of concern. The growing incidence of a disease with a high cure rate increased its prevalence rates, resulting in significant financial impact on society.8 An epidemiological review among US individuals revealed that the incidence of thyroid cancer has increased more than twice in the last 30 years, making it the tumor with most pronounced increase in incidence between the years 1992 and 2002.9
Most studies have attributed this increased incidence to the greater use and better quality of diagnostic tools, which could lead to an increase of incidental diagnoses of previously hidden carcinomas.10 Other studies have produced results opposed to this hypothesis, as they also showed an increase in the incidence of tumors larger than 1cm, leading their authors to believe that this increased incidence may also be occurring among tumors that were not diagnosed occasionally.11 These results are based on inferences from data from preoperative cytological studies and from tumor diameters. Although to date there is no strong evidence of a global and uniform increase in exposure to risk factors historically known for this disease, it still remains uncertain whether the increase of new cases of thyroid cancer reflects a higher risk of developing this neoplasia, or whether this is only an artificial result related to diagnostic procedures.
A great number of international studies are based on regional or national statistics. Only a few institutional papers studied features associated with the diagnosis process, and none of them with a qualitative approach. The authors’ aim was to analyze the pattern of occurrence of thyroid cancer over a decade, in a quantitative and qualitative documentary study based on an institutional historical series, with a detailed description of clinical, epidemiological, and histopathological data, and with information regarding the diagnostic process for nodules and cancers.
MethodsPatientsAfter approval by the Institutional Review Board (Project No. 3483/11), a documentary study with quantitative and qualitative phases was developed. In the quantitative phase of this work, a cross-sectional study was designed involving all patients who underwent thyroidectomy in this institution, with a final diagnosis of cancer, between January of 2001 and December of 2010. The patients were treated by one of the surgeons of the clinical staff of this hospital, mostly members of the head and neck surgery team. Age, gender, fine-needle aspiration biopsy (FNAB) results, histopathology findings, staging and total number of thyroidectomies performed in the same period were introduced in a specific database. All data were collected by the same investigator (Girardi FM). Carcinomas were classified according to their major groups: papillary, follicular, medullary, poorly differentiated, and undifferentiated or anaplastic tumors. Patients treated at other institutions, patients with a diagnosis different from carcinoma, cases of concomitant carcinomas with different histology in the same gland, cases of unresectable tumors, and cases without tumor diameter information were excluded from this study.
Among the cases included, a convenience sample containing all patients diagnosed with microcarcinoma and whose preoperative consultation had occurred at this institution was selected for the qualitative phase of the study. At this stage, it was decided to analyze only cases of microcarcinoma, simply to determine whether it can be generalized that small diameter tumors usually represent nodes or cancers of incidental diagnosis. In this part of the study, the diagnostic process of thyroid nodules and cancers was evaluated. For this purpose, a content analysis was completed after reading and interpreting clinic, epidemiological and histopathological data, as well as analyzing admission notes, anamnesis, medical evolutions, surgical descriptions, ultrasonographic reports and clinical impressions described in the patients’ medical records. According to Bardin (1977), the analysis was divided into three stages: (1) pre-analysis, which included a “floating” reading and the delimitation of documents for further analysis; (2) evaluation and classification of the material and aggregation to the content analysis, in order to allow the emergence of hypotheses and the classification of the units; and (3) interpretation of the obtained results.12 The units and subunits derived from this stage of the study can be found in Table 1. After sorting of results in units and subunits, the chi-squared test was used to compare proportions between the halves of the decade. Incidentally diagnosed nodules were defined as those diagnosed incidentally in clinical examinations, imaging studies, or during neck exploration by other causes unrelated to thyroid disease. Incidentally diagnosed cancers were defined as those whose diagnosis occurred without suspicion or confirmation of malignancy in preoperative tests and evaluations.
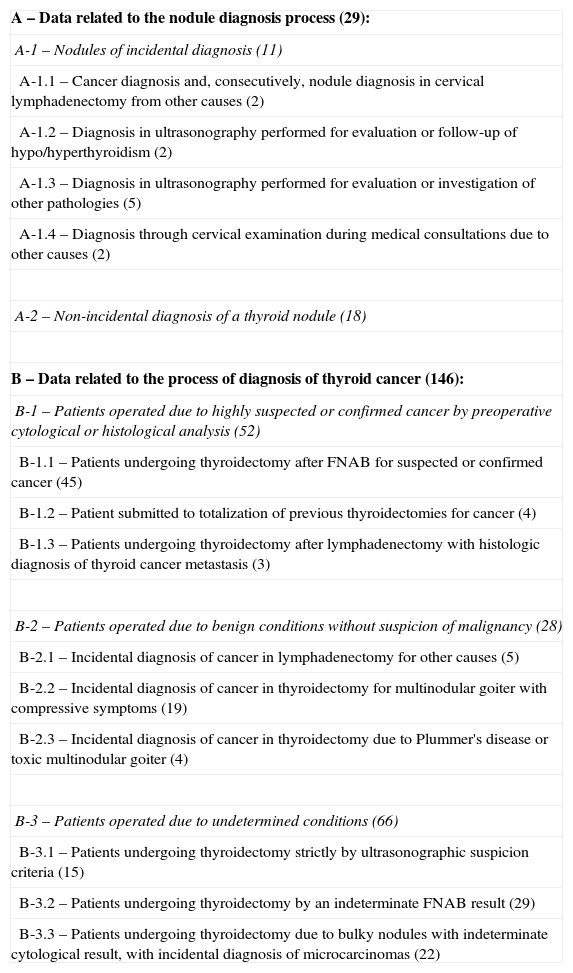
Content analysis: categorization and codification of the diagnostic process of nodules and of thyroid cancer cases among thyroid microcarcinomas.
| A – Data related to the nodule diagnosis process (29): |
| A-1 – Nodules of incidental diagnosis (11) |
| A-1.1 – Cancer diagnosis and, consecutively, nodule diagnosis in cervical lymphadenectomy from other causes (2) |
| A-1.2 – Diagnosis in ultrasonography performed for evaluation or follow-up of hypo/hyperthyroidism (2) |
| A-1.3 – Diagnosis in ultrasonography performed for evaluation or investigation of other pathologies (5) |
| A-1.4 – Diagnosis through cervical examination during medical consultations due to other causes (2) |
| A-2 – Non-incidental diagnosis of a thyroid nodule (18) |
| B – Data related to the process of diagnosis of thyroid cancer (146): |
| B-1 – Patients operated due to highly suspected or confirmed cancer by preoperative cytological or histological analysis (52) |
| B-1.1 – Patients undergoing thyroidectomy after FNAB for suspected or confirmed cancer (45) |
| B-1.2 – Patient submitted to totalization of previous thyroidectomies for cancer (4) |
| B-1.3 – Patients undergoing thyroidectomy after lymphadenectomy with histologic diagnosis of thyroid cancer metastasis (3) |
| B-2 – Patients operated due to benign conditions without suspicion of malignancy (28) |
| B-2.1 – Incidental diagnosis of cancer in lymphadenectomy for other causes (5) |
| B-2.2 – Incidental diagnosis of cancer in thyroidectomy for multinodular goiter with compressive symptoms (19) |
| B-2.3 – Incidental diagnosis of cancer in thyroidectomy due to Plummer's disease or toxic multinodular goiter (4) |
| B-3 – Patients operated due to undetermined conditions (66) |
| B-3.1 – Patients undergoing thyroidectomy strictly by ultrasonographic suspicion criteria (15) |
| B-3.2 – Patients undergoing thyroidectomy by an indeterminate FNAB result (29) |
| B-3.3 – Patients undergoing thyroidectomy due to bulky nodules with indeterminate cytological result, with incidental diagnosis of microcarcinomas (22) |
The absolute frequencies of each category are indicated in brackets.
FNAB, fine-needle aspiration biopsy.
Descriptive analysis was used to summarize the data. The Kolmogorov–Smirnov test was used to assess the normality of continuous variables. Continuous variables with normal distribution were expressed as mean and standard deviation; those without normal distribution were expressed as median and minimum and maximum values. Categorical variables were expressed as absolute and relative frequency. Student's t-test was used to compare means of age; the Mann–Whitney U-test was used for diameter analysis, and the non-parametric chi-squared test was used to compare categorical variables. Statistical analysis was performed using EpiInfo software, version 3.4.3 (2007). All tests considered a significance level of 5%.
PathologyDuring the study period, the surgical specimens of total and partial thyroidectomy were reviewed by one of the 11 pathologists of this medical service. In 93.2% of cases, the histopathological analysis was performed by the same professional, a medical pathologist with training in head and neck pathology and with special dedication to thyroid gland diseases. The pathological staging was performed according to the seventh edition of the American Joint Committee on Cancer pTNM staging system.13 Tumors were considered multifocal when two or more foci were found in one or both lobes. Hashimoto's thyroiditis was suggested based on histopathological findings. Microcarcinomas were defined as tumors of diameter equal to or less than 1cm in the histological examination. Lymph node status was defined based on evidence of metastases in lymph nodes removed. Invasion or extraglandular involvement was defined based on evidence of tumor cells infiltrating beyond the glandular capsule on microscopic examination. The term follicular lesion was used only for benign tumors with follicular cell groups arranged in thyroid follicles, excluding follicular carcinoma and the follicular variant of thyroid PC.14 The cytological diagnosis was made according to Bethesda criteria prior to 2007, in which the lesions were classified into five categories: Unsatisfactory (I), Benign (II), Undetermined (III), Suspect for malignancy (IV), and Malignant (V).15
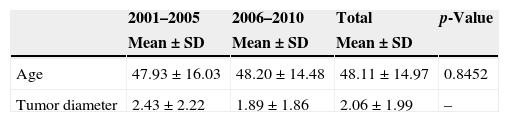
ResultsQuantitative phaseBetween January 1st, 2001 and December 31st, 2010, 3536 thyroidectomy procedures were performed at this institution, 628 (17.7%) of them due to cancer. Seventeen cases were excluded for being malignant neoplasms of other histological subtypes (thyroid lymphomas, sarcomas, and metastases to the thyroid gland), two cases were excluded for having been treated outside of this institution (one follicular carcinoma and one medullary carcinoma), four for being unresectable cases (all anaplastic carcinomas), five cases for having more than one concomitant tumor subtype in the same gland, and three cases due to lack of diameter information (two PC and one follicular carcinoma). A total of 597 patients met the inclusion criteria. The male/female ratio was 1:3.9. The average age was 48.11±14.97 years (range: 12–91 years). The average tumor diameter was 2.6±1.99cm (range: 0.04–5cm). In this universe of 597 patients, 549 (91.9%) underwent total thyroidectomy, while the remaining were treated with partial or subtotal thyroidectomy. Between 2001 and 2010, the number of thyroidectomy operations from all causes increased 1.52-fold. In the same period, an increase of 2.15-fold was observed in surgeries for thyroid cancer (p=0.0002) at this institution. There were 189 cases operated on in the first half of the decade, and 408 cases in the second half.
There were no differences between gender and age in the comparison between the two halves of the decade, even considering groups over/under 45 years. Over the years, greater participation of the head and neck surgery team was observed for thyroidectomy operations due to cancer. Thyroid PC remained the predominant tumor in both periods. The percentage of cases with signs of multifocal disease increased in the second half of the decade. Conversely, a decrease in capsular invasion and in extraglandular involvement rates was observed in the same period, as well as a reduction in tumor size. An increasing proportion of cases in an early stage of disease over the years was also observed, although with marginal significance (x2=3.811; p=0.0509). In addition, an increase in the percentage of cases of microcarcinoma associated with follicular lesions between the analyzed periods (26.4% vs. 33.3%, respectively) was found, although without statistical significance (p=0.1112). The mean diameter of nodules differed between patients with concomitant follicular lesions vs. patients with glands with usual characteristics, except for the presence of carcinoma (U=132,654.0; p=0.0182). Other data are summarized in Table 2.
Over the ten years of study, 220 cases of thyroid microcarcinomas were diagnosed and underwent surgery; 179 of them were women (81.3%) with mean age of 48.91±12.31 years. Of these cases, 89% (196 cases) underwent total thyroidectomy as definitive treatment. In 214 cases (97.2%), the histopathological diagnosis revealed PC; five (2.2%) were medullary carcinomas; and only one (0.4%) was diagnosed with a follicular thyroid carcinoma. The mean tumor diameter was 0.58±0.26cm. Among microcarcinomas, 146 (66.3%) met criteria for inclusion in the qualitative phase of the study, 28 belonging to the first half of the decade and 118 to the second. The analysis was divided into two parts: data associated with the diagnostic process for nodules; and data associated with the diagnostic process for cancers. Any other subunit was organized and coded. The descriptive data and comparisons between the halves of the decade are summarized in Tables 2 and 3.
Comparative analysis of clinical and histopathological data between the two halves of the decade.
| 2001–2005 | 2006–2010 | Total | p-Value | |
|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | ||
| Age | 47.93±16.03 | 48.20±14.48 | 48.11±14.97 | 0.8452 |
| Tumor diameter | 2.43±2.22 | 1.89±1.86 | 2.06±1.99 | – |
| 2001–2005 | 2006–2010 | Total | p-Value | |
|---|---|---|---|---|
| Median (Min–Max) | Median (Min–Max) | Median (Min–Max) | ||
| Tumor diameter | 1.7 (0.04–10) | 1.2 (0.1–15) | 1.3 (0.04–15) | 0.0412 |
| 2001–2005 | 2006–2010 | Total | p-Value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Thyroidectomies | 1403 | 39.6 | 2133 | 60.3 | 3536 | 100 | 0.0002 |
| Thyroidectomies due to cancer | 189 | 13.4 | 408 | 19.1 | 597 | 16.8 | |
| Gender | 0.1752 | ||||||
| Male | 45 | 23.8 | 76 | 18.6 | 121 | 20.2 | |
| Female | 144 | 76.1 | 332 | 81.3 | 476 | 79.7 | |
| Age (categories) | 0.8806 | ||||||
| <45 years | 77 | 40.7 | 162 | 39.7 | 239 | 40.0 | |
| >45 years | 112 | 59.2 | 246 | 60.2 | 358 | 59.9 | |
| HN Surgical Team | 116 | 61.3 | 323 | 79.1 | 439 | 73.5 | 0.0001 |
| MBB, Pathologist | 173 | 91.5 | 384 | 94.1 | 557 | 93.2 | 0.3181 |
| Histology (CA) | 0.1875 | ||||||
| Papillary | 160 | 84.6 | 366 | 89.7 | 526 | 88.1 | |
| Follicular | 13 | 6.8 | 19 | 4.6 | 32 | 5.3 | |
| Medullary | 10 | 5.2 | 9 | 2.2 | 19 | 3.1 | |
| PD | 1 | 0.5 | 5 | 1.2 | 6 | 1.0 | |
| Anaplastic | 5 | 2.6 | 9 | 2.2 | 14 | 2.3 | |
| Hashimoto's thyroiditisa | 43 | 22.7 | 116 | 28.4 | 159 | 26.6 | 0.1736 |
| Follicular lesionsa | 50 | 26.4 | 136 | 33.3 | 186 | 31.1 | 0.1112 |
| Lymphovascular or neural invasion | 25 | 13.2 | 51 | 12.5 | 76 | 12.7 | 0.9076 |
| Multifocality | 51 | 26.9 | 151 | 37.0 | 202 | 33.8 | 0.0206 |
| Diameter (categories) | 0.0354 | ||||||
| ≤1.0 | 61 | 32.2 | 163 | 39.9 | 224 | 37.5 | |
| 1.1–2.0 | 49 | 25.9 | 121 | 29.6 | 170 | 28.4 | |
| 2.1–3.0 | 22 | 11.6 | 44 | 10.7 | 66 | 11.0 | |
| 3.1–4.0 | 17 | 8.9 | 31 | 7.5 | 48 | 8.0 | |
| >4.0 | 40 | 21.1 | 49 | 12.0 | 89 | 14.9 | |
| Invasion of glandular capsule | 123 | 65.0 | 210 | 51.4 | 333 | 55.7 | 0.0025 |
| Extraglandular commitment | 73 | 38.6 | 118 | 28.9 | 191 | 31.9 | 0.0232 |
| Positive cervical LNs | 49 | 25.9 | 92 | 22.5 | 141 | 23.6 | 0.4237 |
| LNs committed in lateral compartment | 18 | 9.5 | 38 | 9.3 | 56 | 9.3 | 0.9347 |
| Stage | 0.0509 | ||||||
| I–II | 124 | 65.6 | 301 | 73.7 | 425 | 71.1 | |
| III–IV | 65 | 34.3 | 107 | 26.2 | 172 | 28.8 | |
Variables expressed as absolute (N) and relative (%) frequency, mean (standard deviation), or median (minimum and maximum), as appropriate. LNs, lymph nodes; HN, head and neck surgery; MBB, Dr. Marinez Bizarro Barra; CA, carcinoma; PD, poorly differentiated.
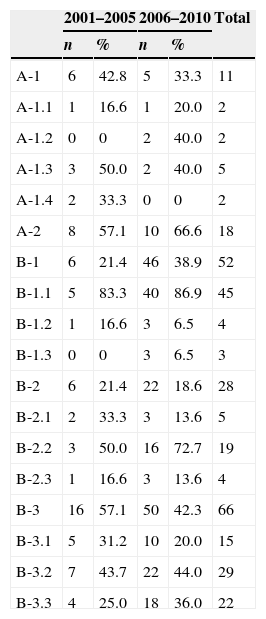
Distribution of absolute and relative frequencies according to the categories generated on content analysis, with a comparison of the two halves of the decade.
| 2001–2005 | 2006–2010 | Total | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| A-1 | 6 | 42.8 | 5 | 33.3 | 11 |
| A-1.1 | 1 | 16.6 | 1 | 20.0 | 2 |
| A-1.2 | 0 | 0 | 2 | 40.0 | 2 |
| A-1.3 | 3 | 50.0 | 2 | 40.0 | 5 |
| A-1.4 | 2 | 33.3 | 0 | 0 | 2 |
| A-2 | 8 | 57.1 | 10 | 66.6 | 18 |
| B-1 | 6 | 21.4 | 46 | 38.9 | 52 |
| B-1.1 | 5 | 83.3 | 40 | 86.9 | 45 |
| B-1.2 | 1 | 16.6 | 3 | 6.5 | 4 |
| B-1.3 | 0 | 0 | 3 | 6.5 | 3 |
| B-2 | 6 | 21.4 | 22 | 18.6 | 28 |
| B-2.1 | 2 | 33.3 | 3 | 13.6 | 5 |
| B-2.2 | 3 | 50.0 | 16 | 72.7 | 19 |
| B-2.3 | 1 | 16.6 | 3 | 13.6 | 4 |
| B-3 | 16 | 57.1 | 50 | 42.3 | 66 |
| B-3.1 | 5 | 31.2 | 10 | 20.0 | 15 |
| B-3.2 | 7 | 43.7 | 22 | 44.0 | 29 |
| B-3.3 | 4 | 25.0 | 18 | 36.0 | 22 |
Variables expressed as absolute (n) and relative (%) frequency.
Data relating to the diagnostic process for nodes (A): from 146 records, 117 (80.1%) did not contain information related to the diagnostic process of thyroid nodules. In the remaining 29 cases (19.8%), two categories emerged: patients with an incidental diagnosis of nodule (A-1) and patients with a non-incidental diagnosis of nodule (A-2). The authors did not find statistically significant differences when comparing the A-1 and A-2 units (χ2=0.279, p=0.579), and the A-1.1, A-1.2, A-1.3, and A-1.4 (the latter not applicable) units between the two halves of the decade.
Data related to the diagnostic process for cancer (B): all 146 medical records contained information related to the diagnostic process for thyroid cancer. Three categories emerged after the analysis of this group: patients operated for confirmation or strong suspicion of malignancy through cytological criteria (Bethesda IV and V) or previous histology (B-1; 52 cases); patients operated due to benign diseases without suspicion of malignancy (B-2; 28 cases); and patients operated for undetermined conditions, either cytopathological or clinical and ultrasonographic criteria, with a variable malignant potential (B-3; 66 cases). The group with an incidental diagnosis of cancer, represented by the B-2.2 subunit; the group undergoing surgery for undetermined conditions, represented by B-3.3 subunit; and the group with a diagnosis or high suspicion of malignancy in the preoperative cytology, represented by B-1.1 subunit, showed increases in the proportion of new cases in the comparison between the two halves of the decade. However, no statistically significant differences were found when comparing B-1, B-2, and B-3 units (χ2=3.14; p=0.208), as well as the B-1.1, B-1.2, and B-1.3 (χ2=1.11; p=0.574); B-2.1, B-2.2, and B-2.3 (χ2=1.41; p=0.493); and B-3.1, B-3.2, and B-3.3 (χ2=1.12; p=0.573) subunits between the two halves of the decade.
DiscussionThe increased incidence of thyroid cancer in the last two decades has been observed in several studies.16–20 Few studies in Brazil analyzed incidence variations in thyroid carcinoma.21,22 Data from various regions of the world have shown an increasing incidence, from 60% to 90%, or even more. Although the present data are based on a single center, this study also observed an increase in the occurrence of thyroid cancer over the years, in proportion to the total number of thyroidectomy procedures performed, a finding which is in line with other institutional series.17,18
Just as observed by other authors,23,24 the proportion of small tumors (<1cm) increased dramatically over the past years in this sample. There was a predominance of histopathological features of low tumor aggressiveness among newly diagnosed cases, suggesting the establishment of earlier diagnoses. In the literature, there is still an ongoing discussion about the reasons for this phenomenon. There is no way to infer the level of impact of each factor on changes in the pattern of disease occurrence. Many studies have related the variations in incidence with the increased use and to the better accuracy of diagnostic tools,16 which would lead to an increase of new cases of incidental diagnosis. However, the parameters for definition of a carcinoma as an incidental event vary significantly. Some studies use the criterion “lack of suspicious or confirmatory cytological results for malignancy”25; others use the incidental finding of cancer in thyroidectomy procedures for multinodular goiter,10 and finally others are based on a nodule found occasionally in imaging studies performed for other causes.26 Most studies do not consider clinical and ultrasonographic data analysis, neither differentiate cases with an incidental diagnosis of nodule vs. cancer. Such information is difficult to measure and may be accessed solely by studies with a qualitative approach.
Some studies support their findings on inferences from preoperative cytology and tumor diameter data. Even among these studies, it is recognized that a review of those clinical circumstances that led to the identification and therapeutic decision in each case should be conducted, with the aim to verify the rate of incidental diagnosis.11 Case studies with an incidental diagnosis of cancer on imaging studies, such as that by Shetty et al.,27 show that the presence of new diagnoses of nodule or cancer among patients with tumors with diameters greater than 1cm does not exclude the possibility that many of these cases may have been diagnosed occasionally.
Burgess et al. analyzed the change in incidence of thyroid cancer in Tasmania between 1988 and 1998. These authors observed an increase in the use of FNA in the preoperative period in patients undergoing thyroidectomy, both for tumors greater than or equal to 1cm, and for tumors less than 1cm; this suggests that more cases are being treated by surgery, thanks to the preoperative suspicion of malignancy, even among patients with microcarcinomas.11 Sosa et al. observed that in the United States, the use of FNAB more than doubled in a period of five years.28 Similar results were found by Busco et al. in Italy.29 In the present study, although no statistically significant differences were found when comparing units and subunits between the two halves of the decade, it was observed that not only is FNAB an increasingly used method in the preoperative period of patients with thyroid nodules, but also that there was a trend for surgical treatment of new cases of microcarcinomas with strong suspicion or cytological confirmation of malignancy. Patients with microcarcinomas diagnosed by cytology in the preoperative period represent an increasing group among the new cases that have been diagnosed, probably reflecting improved accuracy of diagnostic methods.
In 1993 Martinez et al. observed a relationship between histopathological analysis method and frequency of diagnoses of microcarcinoma.30 According to reports of the present pathologists’ group, the number of histological sections in each surgical specimen has also increased over the years, although the annotation of section thickness in the histopathological report is not routinely performed in all cases. Even the American College of Pathologists (ACP) protocols31 do not mention a section thickness that must be routinely used–a fact that, as is well known, can influence the incidence of occult tumors. Most of the information related to histopathological analysis methods is based on indirect results. In a study by Haymart et al., a higher percentage of incidental microcarcinoma detections was found among patients undergoing surgery for follicular neoplasms, compared to other benign conditions (9% vs. 6%, respectively).25 Similarly, an increasing rate of carcinomas associated with follicular lesions was also observed, when the two halves of the decade were compared, although without statistical significance. Usually, a greater number of histological sections are carried out to differentiate benign follicular lesions vs. carcinomas with a follicular pattern. It was also noted that the mean diameter of the nodules was significantly different among patients with associated follicular lesions and with glands without other features, except for the presence of cancer. Similarly, in the qualitative analysis phase, a rising group represented by patients operated for goiter or ecographically suspicious nodules was noted, with or without previous FNAB, showing follicular lesions or Hashimoto's thyroiditis in nodular form, associated with the presence of microcarcinomas incidentally diagnosed in histological sections.
Based on these results, the authors cannot suggest another reason for the changes in pattern of occurrence observed besides those related to medical behavior, and to the accuracy and dissemination of diagnostic methods. It would be unlikely to observe an increase in the occurrence of disease in such a short period of time, if were not for a relationship to medical practices or to any change in institutional policies, with reference to surgical services in this hospital. The probability of cancer diagnosis among cases undergoing thyroidectomy has increased over the decade. The new cases tend to present with smaller diameters and with less aggressive characteristics. These results suggest a trend toward an earlier diagnosis of the disease, which, as it is believed, may also be related to the availability and accuracy of diagnostic methods. The authors believe that the lack of statistical significance – when the data from the qualitative phase were analyzed – is due to the losses and to the small number of analyzable cases in each unit or subunit, especially in the first half of the decade.
Other factors may have influenced the pattern of occurrence observed in this study, although it is difficult to establish how each of these findings may have affected the final result. Increasingly, the professional responsible by the surgical treatment of thyroid cancer in this institution is the head and neck surgeon. Furthermore, there is a tendency for completion of the histopathological analysis of thyroid specimens by the same pathologist, which also could interfere with variations of occurrence of tumors with borderline characteristics.
ConclusionsMany factors may have influenced the changes in the pattern of occurrence of thyroid cancer in this institution. An increase in the proportion of malignant neoplasms among cases undergoing thyroidectomy was found, as well as a trend to earlier diagnoses over the years of this study. It was observed that it is possible to find small-diameter nodules and neoplasias non-incidentally. Among microcarcinomas, an increase in the proportion of cases with preoperative suspicion of neoplasia was observed, suggesting a trend toward improvement in the accuracy of preoperative diagnostic methods among small tumors. Cases of incidental diagnosis of microcarcinomas in thyroidectomies for benign or indeterminate conditions are also increasingly common, suggesting changes in the analytical method and in histopathological routine. Longitudinal studies can complement these results, reducing losses by improving the quality of registration of data related to the diagnosis process.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Girardi FM, Barra MB, Zettler CG. Analysis of pattern of occurrence of thyroid carcinoma between 2001 and 2010. Braz J Otorhinolaryngol. 2015;81:541–8.
Institution: Santa Rita Hospital – Hospital Complex, Santa Casa de Porto Alegre, Porto Alegre, RS, Brazil.