Obstructive sleep apnea syndrome has multifactorial causes. Although indications for surgery are evaluated by well-known diagnostic tests in the awake state, these do not always correlate with satisfactory surgical results.
ObjectiveTo undertake a systematic review on endoscopy during sleep, as one element of the diagnosis routine, aiming to identify upper airway obstruction sites in adult patients with OSAS.
MethodsBy means of electronic databases, a systematic review was performed of studies using drug-induced sleep endoscopy to identify obstruction sites in patients with OSAS.
ResultsTen articles were selected that demonstrated the importance of identifying multilevel obstruction, especially in relation to retrolingual and laryngeal collapse in OSAS.
ConclusionDISE is an additional method to reveal obstruction sites that have not been detected in awake patients.
A síndrome de apneia obstrutiva do sono (SAOS) apresenta causas multifatoriais com indicação cirúrgica avaliada por meio dos exames diagnósticos consagrados em vigília, que podem, porém, não assegurar resultados cirúrgicos satisfatórios.
ObjetivoRealizar uma revisão sistemática sobre a endoscopia do sono, como parte da rotina diagnóstica, em pacientes adultos com SAOS a fim de identificar os sítios de obstrução da via aérea superior.
MétodoRevisão sistemática da literatura (RSL), a partir de bases de dados eletrônicas, dos estudos que identificaram os sítios de obstrução em pacientes com SAOS a partir da endoscopia do sono induzido por droga (DISE).
ResultadosForam selecionados dez artigos que demonstraram relevância na identificação dos multiníveis de obstrução, principalmente em relação ao colapso retro-lingual e laríngeo na SAOS.
ConclusãoDISE é um método adicional na identificação de sítios de obstrução não detectáveis no paciente em vigília.
Obstructive sleep apnea syndrome (OSAS) is characterized by periods of cessation (apnea) and reduction (hypopnea) of oronasal airflow during sleep accompanied by oxyhemoglobin desaturation. This breathing disorder is a result of abnormal anatomy superimposed on physiological or excessive reduction of muscle tone during sleep.1,2
It affects approximately 2% of females and 4% of males, with a peak incidence between 40 and 60 years of age in both sexes. It has high rates of morbidity and mortality, and is considered a public health problem due to cardiovascular outcome, the risk of occupational and automobile accidents, as well as the poor quality of life, with neurocognitive impairment.
Clinical symptoms are snoring, restless sleep, daytime fatigue, decreased intellectual capacity, and personality changes. Between 80% and 90% of individuals with OSAS are unaware of their diagnosis, which can be attained more accurately and effectively with the identification and individualized analysis of obstruction sites.3–6
The disease has multifactorial causes, and patients with OSAS who receive recommendations for surgical intervention, by reputable diagnostic tests such as clinical examination, video examinations (nasal endoscopy, laryngoscopy, nasofibrolaryngoscopy), cephalometry, computed tomography, and magnetic resonance imaging, do not necessarily obtain a satisfactory and definitive result from surgery. Nasofibrolaryngoscopy (NFL) under sedation, also known as drug-induced sleep endoscopy (DISE), may be an important tool in locating the obstruction site in these patients, and thus allowing the best clinical and/or surgical approach, thereby improving the qualitative and quantitative results of treatment. Moreover, it could help prevent unrealistic expectations regarding the available treatment for each patient.
Therefore, the objective of this study was to perform a systematic literature review (SLR) on sleep endoscopy as a diagnostic tool in adult patients with OSAS, aiming to identify upper airway obstruction sites.
MethodsBetween October 20th and 30th of 2013, articles indexed in the electronic databases of the Medical Literature Analysis and Retrieval System Online (MEDLINE), the Latin American and Caribbean Health Sciences Literature (LILACS), the Cochrane Central Register of Controlled Trials (CENTRAL), and the Spanish Bibliographic Index of Health Sciences (IBECS) were searched at the Regional Library of Medicine (BIREME). Additionally, a review of references from the selected articles was performed to identify other potentially relevant studies.
The descriptors used were: obstructive sleep apnea AND endoscopy AND sleep, obtained from the descriptors in health sciences (DeCS). Other searches were also performed, including the descriptors in English (MeSH terms: Sleep Apnea Syndromes, Sleep Disorders, Sleep Apnea, Obstructive, Endoscopy, Sleep) but it was observed that the above search repeated all the studies that were present in the first.
Studies that used the evaluation of upper airway obstruction sites in patients with OSAS as the outcome were selected, although some had other associated outcomes. The search was restricted to articles in adult humans, written in Portuguese, English, and Spanish, and performed by a researcher, based on the titles recovered from the databases, then abstracts, and finally full published articles.
These were evaluated independently. The selected articles were submitted to the procedures specified by STROBE (Strengthening the Reporting of Observational Studies in Epidemiology), an initiative of 2007, in the version translated into Portuguese in 2010.7 STROBE provides a recommendation on how to report an observational study more adequately without any reference to the study quality. For that purpose, the authors used the strength of recommendation and level of evidence of diagnostic studies based on the study design, according to the “Oxford Center For Evidence-based Medicine” – last updated in 2011.8
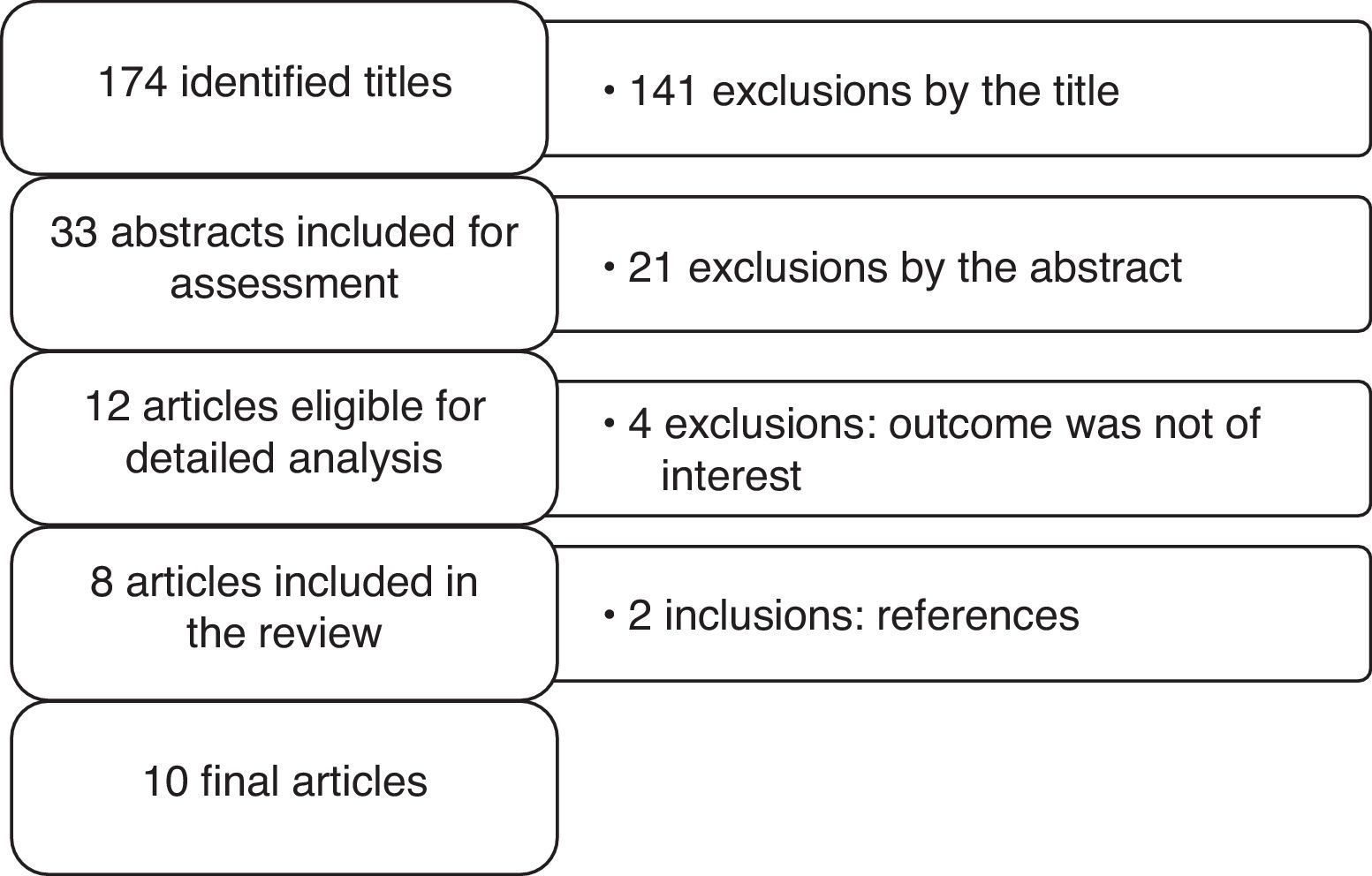
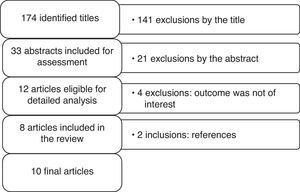
A total of 174 titles were identified in the following databases: MEDLINE (160), LILACS (7), CENTRAL (4), and IBECS (3). Fig. 1 shows the flowchart of article selection included in this review. Looking for studies that had as outcome upper airway obstruction sites in patients with OSAS based on sleep endoscopy results, using midazolam and/or propofol, the articles were initially analyzed by title and those selected were evaluated based on the abstract in the next phase and subsequently, the full texts.
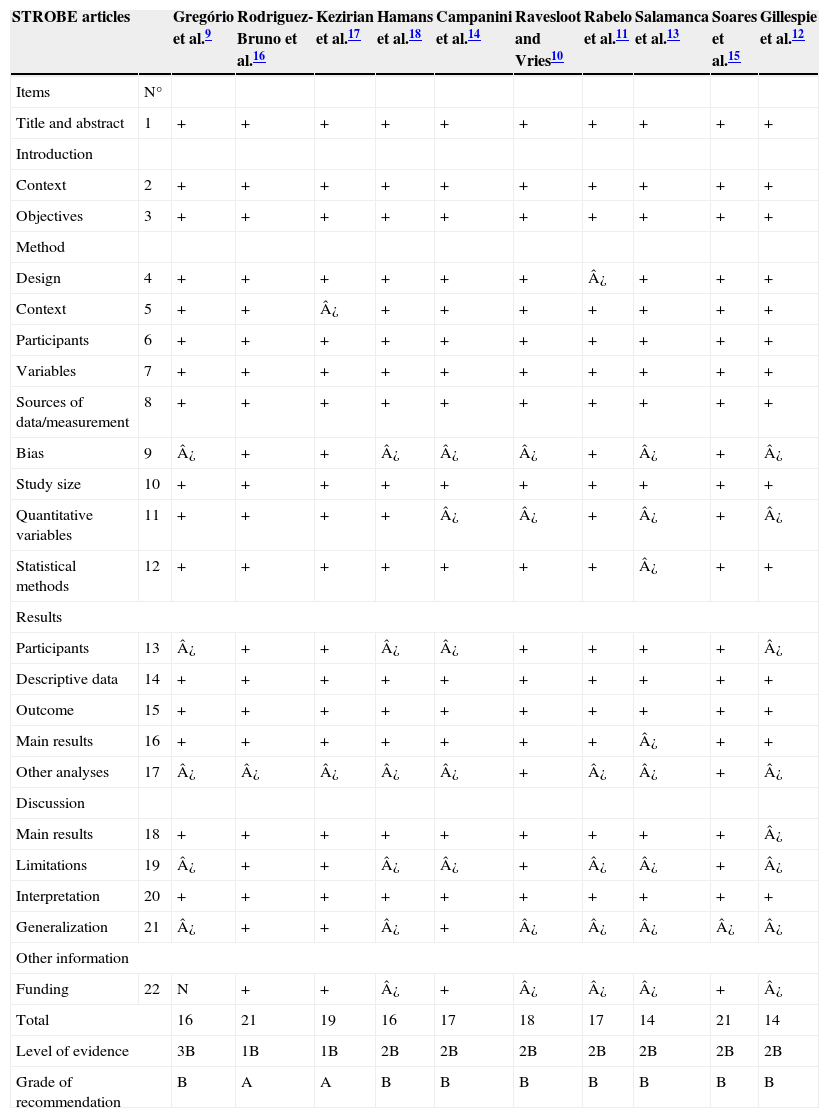
ResultsA total of ten articles were included in this systematic review, published between the years 2007 and 2013, with the number of patients ranging from eight to 614 individuals. The number of essential items identified in the studies, according to STROBE, ranged from 14 to 21, with a median of 17, as shown in Table 1. The degree of recommendations of the studies ranged from A to B. This assignment of qualitative categories to grades of recommendations indicates strong and moderate evidence, respectively.
Analysis of the selected articles according to the STROBE criteria.7
| STROBE articles | Gregório et al.9 | Rodriguez-Bruno et al.16 | Kezirian et al.17 | Hamans et al.18 | Campanini et al.14 | Ravesloot and Vries10 | Rabelo et al.11 | Salamanca et al.13 | Soares et al.15 | Gillespie et al.12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Items | N° | ||||||||||
| Title and abstract | 1 | + | + | + | + | + | + | + | + | + | + |
| Introduction | |||||||||||
| Context | 2 | + | + | + | + | + | + | + | + | + | + |
| Objectives | 3 | + | + | + | + | + | + | + | + | + | + |
| Method | |||||||||||
| Design | 4 | + | + | + | + | + | + | ¿ | + | + | + |
| Context | 5 | + | + | ¿ | + | + | + | + | + | + | + |
| Participants | 6 | + | + | + | + | + | + | + | + | + | + |
| Variables | 7 | + | + | + | + | + | + | + | + | + | + |
| Sources of data/measurement | 8 | + | + | + | + | + | + | + | + | + | + |
| Bias | 9 | ¿ | + | + | ¿ | ¿ | ¿ | + | ¿ | + | ¿ |
| Study size | 10 | + | + | + | + | + | + | + | + | + | + |
| Quantitative variables | 11 | + | + | + | + | ¿ | ¿ | + | ¿ | + | ¿ |
| Statistical methods | 12 | + | + | + | + | + | + | + | ¿ | + | + |
| Results | |||||||||||
| Participants | 13 | ¿ | + | + | ¿ | ¿ | + | + | + | + | ¿ |
| Descriptive data | 14 | + | + | + | + | + | + | + | + | + | + |
| Outcome | 15 | + | + | + | + | + | + | + | + | + | + |
| Main results | 16 | + | + | + | + | + | + | + | ¿ | + | + |
| Other analyses | 17 | ¿ | ¿ | ¿ | ¿ | ¿ | + | ¿ | ¿ | + | ¿ |
| Discussion | |||||||||||
| Main results | 18 | + | + | + | + | + | + | + | + | + | ¿ |
| Limitations | 19 | ¿ | + | + | ¿ | ¿ | + | ¿ | ¿ | + | ¿ |
| Interpretation | 20 | + | + | + | + | + | + | + | + | + | + |
| Generalization | 21 | ¿ | + | + | ¿ | + | ¿ | ¿ | ¿ | ¿ | ¿ |
| Other information | |||||||||||
| Funding | 22 | N | + | + | ¿ | + | ¿ | ¿ | ¿ | + | ¿ |
| Total | 16 | 21 | 19 | 16 | 17 | 18 | 17 | 14 | 21 | 14 | |
| Level of evidence | 3B | 1B | 1B | 2B | 2B | 2B | 2B | 2B | 2B | 2B | |
| Grade of recommendation | B | A | A | B | B | B | B | B | B | B | |
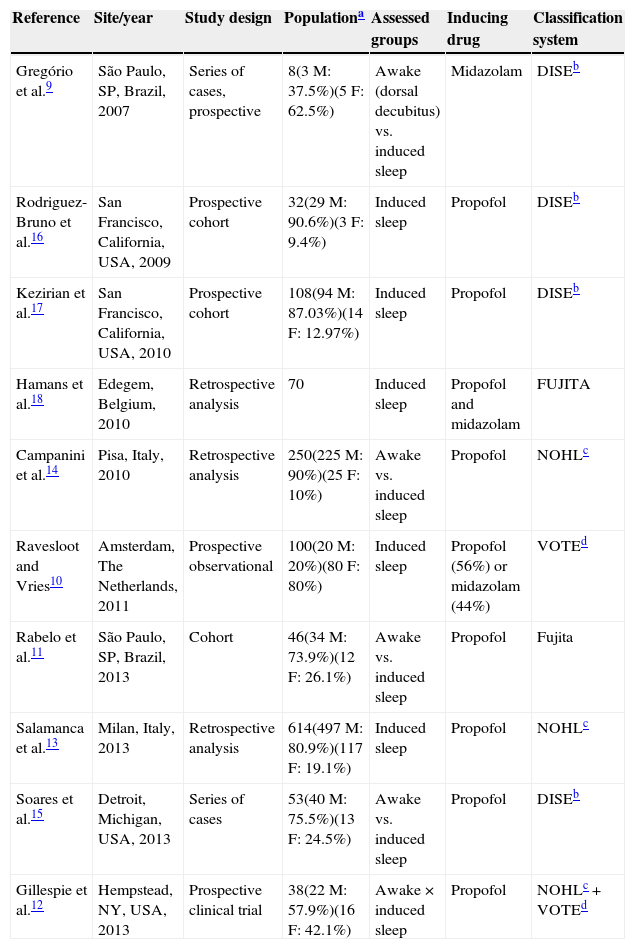
The studies used midazolam9,10 and propofol10–17 to perform sedation for nasofibrolaryngoscopy, either alone or associated.18 The types of classifications used in the identification of obstruction sites varied among studies and used the own parameters of DISE,9,11,16,18 the Fujita classification,11,18 velum oropharynx tongue-base epiglottis (VOTE),13 or nose oropharynx hypopharynx larynx (NOHL).13,14 All selected studies were favorable to the DISE as an important tool in the assessment of obstruction sites in patients with OSAS.
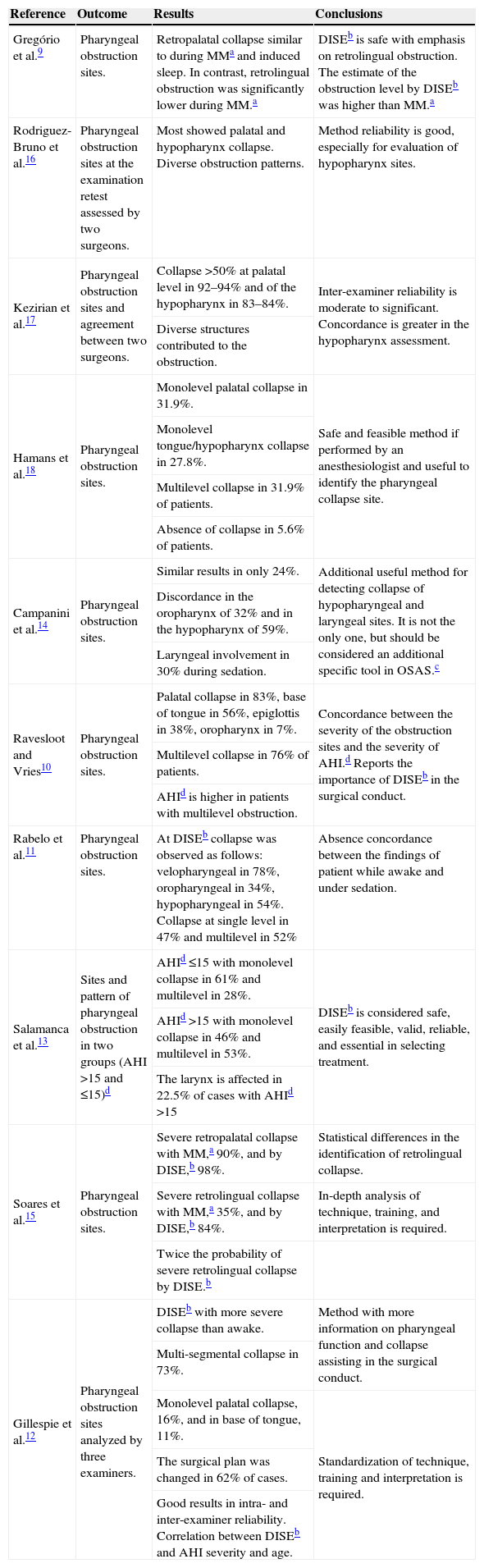
Rabelo et al., when analyzing a prospective cohort of 46 patients using the Fujita classification, found no concordance between the findings of patients assessed in wakefulness and under sedation. Patients submitted to sleep endoscopy showed involvement of the velopharyngeal region in 78.26% of cases, oropharyngeal narrowing in 34.78%, and hypopharyngeal narrowing in 54.34%. Obstructions at a single level were observed in 47.83%, while multilevel obstructions were observed in 52.17%.11 However, other studies evaluating the airway during wakefulness and under induced sleep did not differ significantly in the presence of severe retropalatal collapse, but showed significant difference in the incidence of severe retrolingual collapse. Gregorio et al., when analyzing a small sample of eight patients, using midazolam to perform sedation, observed similar retropalatal obstruction during the Müller maneuver (MM) and induced sleep. In contrast, retrolingual obstruction was significantly lower during MM.9
Hamans et al., in a retrospective analysis of 70 patients undergoing DISE with midazolam and propofol, found monolevel palatal collapse in 31.9%, monolevel tongue/hypopharynx collapse in 27.8%, and collapse at several levels in 31.9% of patients. No collapse was observed in 5.6% of patients. Sleep endoscopy was considered feasible and safe in daily practice, when sedation is performed by an anesthesiologist, and is helpful in locating the collapse site in the airway, which may interfere with treatment choices.18
Ravesloot and de Vries, in a prospective analysis of 100 DISEs evaluated using the VOTE classification, found several levels of obstruction, present in 76 patients, statistically significant when associated with a higher apnea-hypopnea index (AHI), compared to patients with obstruction at a single level. They found that most patients had obstruction at a palatal level (83%), at the base of the tongue (56%), or at the epiglottis (38%).
Patients with complete concentric collapse of the soft palate were significantly more likely to have higher AHI and body mass index (BMI), while an anteroposterior velar collapse was significantly associated with a lower BMI. Moreover, the AHI was significantly higher in patients with complete anterior-posterior collapse of the tongue. The observation of an obstruction at the base of the tongue or epiglottis was more common in patients with positional OSAS; however, this difference was not statistically significant (p=0.058).10 Gillespie et al., in a prospective study with 38 patients, found multi-segmental airway collapse in 73% of cases, uni-segmental collapse at palatal level in 16%, and at the base of tongue level in 11%. The surgical plan was changed after sleep endoscopy in 23 cases (62%) and remained unchanged in 14 cases (38%).12Patients with complete concentric collapse of the soft palate were significantly more likely to have higher AHI and body mass index (BMI), while an anteroposterior velar collapse was significantly associated with a lower BMI. Moreover, the AHI was significantly higher in patients with complete anterior-posterior collapse of the tongue. The observation of an obstruction at the base of the tongue or epiglottis was more common in patients with positional OSAS; however, this difference was not statistically significant (p = 0.058).12 Gillespie et al., in a prospective study with 38 patients, also using the VOTE classification, found multi-segmental airway collapse in 73% of cases, uni- segmental collapse at palatal level in 16%, and at the base of tongue level in 11%. The surgical plan was changed after sleep endoscopy in 23 cases (62%) and remained unchanged in 14 cases (38%).13
Other conclusions should also be mentioned, such as the absence of significant correlation between DISE scores and BMI, tonsillar grading, the modified Mallampati Index, the Epworth Sleepiness Scale (ESS) or the quality of life assessment using the Functional Outcomes of Sleep Questionnaire (FOSQ). Thus, the increasing DISE score seems to indicate greater severity when measured by AHI.
Salamanca et al. used the NOHL classification system and reported the largest analyzed population of 614 patients, and divided the subjects into those with AHI ≤15 and AHI >15. They found in the first group, AHI ≤15 (32.4%), a monolevel obstruction in 61.3% (92.6% oropharynx) and multilevel in 28.2% (oro- and hypopharynx 87.5%). In the second group, AHI >15 (67.6%), they found one monolevel obstruction in 46.5% (95% oropharynx) and multilevel in 53.5% (obstruction of two levels in 91.5%, with oropharynx and hypopharynx obstruction in 77%; obstruction of three levels in 8.5%, with oropharynx, hypopharynx, and larynx obstruction in 8.5%). The larynx participated in 12.5% of cases with AHI >15. DISE was considered a safe, easy-to-perform, valid, and reliable procedure, in addition to being considered by the group as an important clinical assessment that may be essential in determining treatment.13
Campanini et al., with the second largest series (250 patients), also used the NOHL classification and demonstrated identical obstruction sites identified at endoscopy during wakefulness and induced sleep in only 25% of patients.14 Soares et al., who retrospectively assessed 53 patients, showed that the observations made when awake and during DISE were not significantly different regarding the presence of severe retropalatal collapse, but differed significantly regarding the incidence of severe retrolingual collapse (DISE 84.9%; wakefulness 35.8%). In patients with Friedman I and II, regarding the tongue position, the difference was even greater (DISE 88.9%; wakefulness 16.7%).15
Rodriguez-Bruno et al. prospectively studied 32 patients that underwent two separate DISE assessments. The studies were evaluated by a non-blinded surgeon and by another blinded surgeon (who only knew whether or not the patient had undergone prior tonsillectomy). Almost all showed evidence of obstruction at the palate level; the vast majority also showed evidence at the hypopharynx level. The obstruction patterns were diverse. Test–retest reliability results were higher for the evaluations related to the hypopharynx. The two DISE studies were reviewed twice by each surgeon. They found good test–retest reliability (range 50–80%), mainly in airway assessment at the hypopharynx level.16 These findings were similar to those found in the study of Gillespie et al., which assessed the test–retest and inter-examiner reliability performed by three otorhinolaryngologists qualified in DISE examinations. The inter-examiner reliability, when blindly and randomly assessed, demonstrated good results (K=0.65, K=0.62 between pairs of observers). Test–retest reliability was good (K=0.61).12
The inter-rater reliability was also observed by Kezirian et al. in a prospective study of 108 patients, in which all subjects exhibited evidence of palatal obstruction and most also demonstrated hypopharyngeal obstruction. Both reviewers determined that most individuals had palate and hypopharynx obstruction. Video images were subsequently reviewed by two surgeons. The reliability between the presence of obstruction in the palate and the hypopharynx (K=0.76 and K=0.79, respectively) was higher than for the degree of obstruction (weighted K-values=0.60 and 0.44). The reliability of the evaluation of the hypopharynx structures was greater than for those of the palate. In general, DISE inter-observer reliability ranged from moderate to substantial.17
The detailed characteristics of the studies are described in Tables 2 and 3.
Synthesis of the 10 selected articles.
| Reference | Site/year | Study design | Populationa | Assessed groups | Inducing drug | Classification system |
|---|---|---|---|---|---|---|
| Gregório et al.9 | São Paulo, SP, Brazil, 2007 | Series of cases, prospective | 8(3 M: 37.5%)(5 F: 62.5%) | Awake (dorsal decubitus) vs. induced sleep | Midazolam | DISEb |
| Rodriguez-Bruno et al.16 | San Francisco, California, USA, 2009 | Prospective cohort | 32(29 M: 90.6%)(3 F: 9.4%) | Induced sleep | Propofol | DISEb |
| Kezirian et al.17 | San Francisco, California, USA, 2010 | Prospective cohort | 108(94 M: 87.03%)(14 F: 12.97%) | Induced sleep | Propofol | DISEb |
| Hamans et al.18 | Edegem, Belgium, 2010 | Retrospective analysis | 70 | Induced sleep | Propofol and midazolam | FUJITA |
| Campanini et al.14 | Pisa, Italy, 2010 | Retrospective analysis | 250(225 M: 90%)(25 F: 10%) | Awake vs. induced sleep | Propofol | NOHLc |
| Ravesloot and Vries10 | Amsterdam, The Netherlands, 2011 | Prospective observational | 100(20 M: 20%)(80 F: 80%) | Induced sleep | Propofol (56%) or midazolam (44%) | VOTEd |
| Rabelo et al.11 | São Paulo, SP, Brazil, 2013 | Cohort | 46(34 M: 73.9%)(12 F: 26.1%) | Awake vs. induced sleep | Propofol | Fujita |
| Salamanca et al.13 | Milan, Italy, 2013 | Retrospective analysis | 614(497 M: 80.9%)(117 F: 19.1%) | Induced sleep | Propofol | NOHLc |
| Soares et al.15 | Detroit, Michigan, USA, 2013 | Series of cases | 53(40 M: 75.5%)(13 F: 24.5%) | Awake vs. induced sleep | Propofol | DISEb |
| Gillespie et al.12 | Hempstead, NY, USA, 2013 | Prospective clinical trial | 38(22 M: 57.9%)(16 F: 42.1%) | Awake×induced sleep | Propofol | NOHLc + VOTEd |
Synthesis of the ten selected articles (cont.).
| Reference | Outcome | Results | Conclusions |
|---|---|---|---|
| Gregório et al.9 | Pharyngeal obstruction sites. | Retropalatal collapse similar to during MMa and induced sleep. In contrast, retrolingual obstruction was significantly lower during MM.a | DISEb is safe with emphasis on retrolingual obstruction. The estimate of the obstruction level by DISEb was higher than MM.a |
| Rodriguez-Bruno et al.16 | Pharyngeal obstruction sites at the examination retest assessed by two surgeons. | Most showed palatal and hypopharynx collapse. Diverse obstruction patterns. | Method reliability is good, especially for evaluation of hypopharynx sites. |
| Kezirian et al.17 | Pharyngeal obstruction sites and agreement between two surgeons. | Collapse >50% at palatal level in 92–94% and of the hypopharynx in 83–84%. | Inter-examiner reliability is moderate to significant. Concordance is greater in the hypopharynx assessment. |
| Diverse structures contributed to the obstruction. | |||
| Hamans et al.18 | Pharyngeal obstruction sites. | Monolevel palatal collapse in 31.9%. | Safe and feasible method if performed by an anesthesiologist and useful to identify the pharyngeal collapse site. |
| Monolevel tongue/hypopharynx collapse in 27.8%. | |||
| Multilevel collapse in 31.9% of patients. | |||
| Absence of collapse in 5.6% of patients. | |||
| Campanini et al.14 | Pharyngeal obstruction sites. | Similar results in only 24%. | Additional useful method for detecting collapse of hypopharyngeal and laryngeal sites. It is not the only one, but should be considered an additional specific tool in OSAS.c |
| Discordance in the oropharynx of 32% and in the hypopharynx of 59%. | |||
| Laryngeal involvement in 30% during sedation. | |||
| Ravesloot and Vries10 | Pharyngeal obstruction sites. | Palatal collapse in 83%, base of tongue in 56%, epiglottis in 38%, oropharynx in 7%. | Concordance between the severity of the obstruction sites and the severity of AHI.d Reports the importance of DISEb in the surgical conduct. |
| Multilevel collapse in 76% of patients. | |||
| AHId is higher in patients with multilevel obstruction. | |||
| Rabelo et al.11 | Pharyngeal obstruction sites. | At DISEb collapse was observed as follows: velopharyngeal in 78%, oropharyngeal in 34%, hypopharyngeal in 54%. Collapse at single level in 47% and multilevel in 52% | Absence concordance between the findings of patient while awake and under sedation. |
| Salamanca et al.13 | Sites and pattern of pharyngeal obstruction in two groups (AHI >15 and ≤15)d | AHId ≤15 with monolevel collapse in 61% and multilevel in 28%. | DISEb is considered safe, easily feasible, valid, reliable, and essential in selecting treatment. |
| AHId >15 with monolevel collapse in 46% and multilevel in 53%. | |||
| The larynx is affected in 22.5% of cases with AHId >15 | |||
| Soares et al.15 | Pharyngeal obstruction sites. | Severe retropalatal collapse with MM,a 90%, and by DISE,b 98%. | Statistical differences in the identification of retrolingual collapse. |
| Severe retrolingual collapse with MM,a 35%, and by DISE,b 84%. | In-depth analysis of technique, training, and interpretation is required. | ||
| Twice the probability of severe retrolingual collapse by DISE.b | |||
| Gillespie et al.12 | Pharyngeal obstruction sites analyzed by three examiners. | DISEb with more severe collapse than awake. | Method with more information on pharyngeal function and collapse assisting in the surgical conduct. |
| Multi-segmental collapse in 73%. | |||
| Monolevel palatal collapse, 16%, and in base of tongue, 11%. | Standardization of technique, training and interpretation is required. | ||
| The surgical plan was changed in 62% of cases. | |||
| Good results in intra- and inter-examiner reliability. Correlation between DISEb and AHI severity and age. |
An anatomical, methodological approach during sleep can be crucial to guide the surgeon during decision-making regarding treatment. This review aimed to show the role of DISE as an additional method to identify the sites of obstruction that were not detected by other tests. Several authors have shown that, when incorrectly or insufficiently applied, the selection criteria used for surgical treatment may be responsible for the failure rates related to OSAS surgery.15,17,19
The number of articles found in the present review was small, indicating that there are few studies utilizing this approach. It is noteworthy that this review was systematically performed by a single researcher. Studies with different designs were included and all of them included only individuals with OSAS. The assignment of qualitative categories to the grades of recommendations of selected articles was strong and moderate evidence favored the practice of sleep endoscopy for obstruction site analysis in these patients.
Results are still inconclusive regarding the type of obstruction, due to the difficulty with standardization among the studies. However, when assessing the patient's obstruction sites while awake and under induced sleep, the studies did not differ significantly regarding the presence of severe retro-palatal collapse, but did regarding the incidence of severe retrolingual collapse. Furthermore, examinations by DISE have demonstrated a significant role of laryngeal obstruction in OSAS.
Sleep endoscopy has emerged as an important technique in identifying multilevel collapses, especially in the positioning of the base of the tongue and epiglottis.
There have been no studies that assessed whether the findings obtained by DISE can predict success of surgical treatment in patients with OSAS. Only one article reported that the findings changed the surgical indication12; however, it made no reference to the surgical success in these patients. Sleep endoscopy plays an important role in the identification of multilevel obstruction, without necessarily ensuring treatment success when these sites are surgically addressed.
Although it was not the purpose of this review, it is pertinent to the findings described in the articles that we find good test–retest reliability, especially for airway and hypopharyngeal assessments, as well as good inter-rater reliability.
That the article assessment was performed by a single examiner is a limitation of this study. Furthermore, there was some difficulty in describing results, as the articles did not use the same classification system for the identification of obstruction sites. Nonetheless, the findings of this literature review can be generalized, as they involve studies from different locations, involving a large number of patients, with results pointing toward the same direction.
ConclusionDespite the lack of standardization in clinical examinations, the type of drugs used for sedation and the classification system used, the results obtained till date favor the inclusion of DISE in the investigation of obstruction sites in patients with OSAS, particularly with respect to the larynx and hypopharynx. The technique is valid, dynamic, safe, and easy to perform. The VOTE classification system currently appears to be the most used, as it is easy to apply. Furthermore, the use of a universal DISE scoring system can facilitate the scientific assessment of studies conducted in single centers, as well as multicentric studies, allowing comparison of results.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Viana Jr. AC, Thuler LCS, Araújo-Melo MH. Drug-induced sleep endoscopy in the identification of obstruction sites in patients with obstructive sleep apnea. Braz J Otorhinolaryngol. 2015;81:439–46.
Institution: Universidade Federal do Estado do Rio de Janeiro (UNIRIO), Rio de Janeiro, RJ, Brazil.