Benign tumors of the parotid gland comprise the majority of salivary gland tumors.
ObjectiveTo review the clinical characteristics of parotid gland tumors submitted to surgical treatment by the same surgeon.
MethodsRetrospective study with 154 patients who had parotid gland tumors. Clinical and histological data, type of surgery, and complications were assessed and described.
ResultsThe main manifestation was a mass with a median evolution of 12 months for benign tumors and five months for malignant tumors. Ultrasonography was the most frequent complementary exam. Pleomorphic adenoma was the most common of the benign tumors, and mucoepidermoid carcinoma was the most frequent malignant tumor. Superficial parotidectomy with preservation of the facial nerve was the most common surgical procedure and reversible paresis of branches of the facial nerve was the most common complication.
ConclusionsPleomorphic adenoma is the most common parotid gland tumor and superficial parotidectomy with preservation of the facial nerve is the most common and appropriate treatment for most low-morbidity tumors.
Os tumores de parótida são frequentemente de natureza benigna e correspondem à maioria dos tumores de glândulas salivares.
ObjetivoRevisar as características clínicas de neoplasias de parótidas submetidas a tratamento cirúrgico pelo mesmo cirurgião.
MétodoEstudo retrospectivo, onde foram avaliados 154 pacientes com neoplasia de parótida. Dados clínicos, histológicos, tipo de cirurgia e complicações foram compilados e descritos.
ResultadosA principal manifestação foi a de uma massa tumoral com uma mediana de tempo de evolução de 12 meses para os tumores benignos e 5 meses para os tumores malignos. A ecografia foi o exame complementar mais indicado. Dentre os tumores benignos, o adenoma pleomórfico foi o mais comum e o carcinoma mucoepidermóide o mais frequente dentre os malignos. A parotidectomia superficial com preservação do nervo facial foi a cirurgia mais indicada e a paresia reversível de ramos do nervo facial, a complicação mais prevalente.
ConclusõesO adenoma pleomórfico é o tumor mais comum da glândula parótida e a parotidectomia superficial com preservação do nervo facial é o tratamento mais adequado para a maioria dos tumores de baixa morbidade.
Parotid tumors affect 1:100,000 people, representing 2–3% of tumors of the head and neck and 80% of salivary gland tumors.1,2 In 1991, parotid tumors were histologically classified into more than 30 types by the World Health Organization (WHO).2
The current literature estimates that approximately 80% of these tumors are benign, with pleomorphic adenoma being the most common and occurring between the fourth and sixth decades of life.3 Clinically, the most common manifestation of pleomorphic adenoma is the presence of a solitary, solid, firm, lobulated, mobile nodular lesion with well-defined margins, that is painless, to palpation, and of long evolution. This type of tumor can be quite large and invariably spares the function of the facial musculature. The second most common benign tumor is Warthin's tumor, which mostly affects men after the fifth decade of life and may be bilateral.
The most prevalent malignant tumor is the mucoepidermoid carcinoma, followed by adenoid cystic carcinoma. The presence of pain, facial paralysis, rapid growth, ill-defined margins, and skin infiltration are characteristics that are suspicious for malignancy.2
The first diagnostic imaging assessment for parotid tumors is usually ultrasonography, but this assessment does not determine the indication for surgical treatment. Computed tomography or magnetic resonance imaging assessment is not essential, but may be indicated in selected cases to plan appropriate treatment.2 Fine-needle aspiration (FNA), whether or not guided by ultrasound, can be used as a complementary diagnostic test, especially when a non-characteristic manifestation of pleomorphic adenoma is suspected. The purpose of FNA is to differentiate benign from malignant tumors, as it usually does not establish the definitive histological diagnosis.1–3 Incisional biopsy is contraindicated, as it is often the cause of neoplastic implantation and consequently, of recurrences of pleomorphic adenomas and malignant neoplasms. It is established that multiple recurrences of pleomorphic adenomas increase the possibility of malignant transformation of the tumor (carcinoma in a pleomorphic adenoma) and patients with these tumors often have undergone a biopsy or inadequate surgical excision in the past.1
The parotid gland has a superficial lobe, lateral to the facial nerve, that comprises 4/5 of the glandular parenchyma, and a smaller deep lobe. Superficial parotidectomy with facial nerve preservation is the most often indicated surgical procedure, as 90% of the tumors are located in the glandular superficial lobe and, thus, do not affect the facial nerve.2 Although tumors more often affect the superficial lobe, the term subtotal parotidectomy seems more appropriate than superficial parotidectomy.
The association between the facial nerve and the gland is responsible for most of the technical difficulties and complications of the surgical approaches. Because of a particular tumor histological type or extension, a decision to perform a parotidectomy with deliberate sacrifice of the facial nerve trunk or branches, possibly with an associated neck dissection, is sometimes made during surgery. Therefore, the pathologist's contribution of frozen section examination during surgery is essential. The treatment of malignant tumors of the parotid can be supplemented with adjuvant radiotherapy, but chemotherapy is rarely indicated. The prognosis is determined according to the histological type and the pre- and post-surgical staging.2
The objective of this study was to review the 154 parotidectomies performed by the same surgeon from 1990 to 2011, giving a current overview of clinical examination, laboratory tests, histological types, surgical management, complications, and postoperative outcomes, considering the prevalence of parotid tumors in this population.
MethodWe reviewed the current literature and did a retrospective study of 154 patients with a previous history of parotid tumors, surgically treated from 1990 to 2011 by the same surgeon, performed by database analysis. We included only those patients with complete records and whose surgical indication was not associated with inflammatory disease of the parotid or medical conditions other than tumor-related. All histological findings were performed by the same pathologist from a referral hospital.
Data were computed in an Excel spreadsheet and classified as variables of the analysis, which in turn were classified as qualitative, with a numerical scale code, or as quantitative. Qualitative variables included gender (male or female), disease symptoms, initial physical examination, preoperative tests, chosen surgical technique, postoperative complications, and histological diagnosis. Quantitative variables were age (in years), disease evolution, and follow-up (in months). As for the initial symptoms, the cases were classified as incidental mass, incidental lesion in imaging exams, local pain/inflammation, and previous biopsy. Each of the variables was grouped according to a numerical scale.
Regarding the physical examination, cases were recorded according to the initial clinical impression, which considered lesion location (superficial or deep), size (≤2cm or >2cm), and histological hypothesis according to palpation (non-palpable, adenoma, benign non-adenoma, malignant). Regarding the preoperative data, we verified whether the patient had undergone computed tomography (CT), magnetic resonance imaging (MRI), or ultrasound; the result was evaluated and the tumor was classified as a solid or cystic lesion. FNA was assessed for the groups as follows: no examination, benign result, or malignant result. As for the surgical technique, the operations were classified as total or subtotal parotidectomy and dermal parotidectomy, divided into groups represented by a numerical scale from 0 to 2.
The presence of intraoperative frozen sections was considered. When present, the results were separated into two groups: benign and malignant. The presence of FNA and the definitive histological diagnosis were correlated. Regarding the surgical preservation of the facial nerve, the sample comprised two groups: one submitted to intentional surgical resection and the other in which it was not necessary. Postoperative complications were also analyzed: transient paresis, transient paralysis, salivary fistula, Frey's syndrome, and permanent facial paralysis. Patients who had recurrence during the period were analyzed regarding the histological type.
The database was transferred to IBM Statistical Package for the Social Sciences, PSS 20 software, where data analyses were performed. The program was used to calculate frequencies, means, medians, and standard deviations, as well as to set the distribution asymmetry of scalar variables. Frequencies were obtained for the nominal variables and crossovers were evaluated for significance using Pearson's χ2 test, with p<0.001 considered significant.
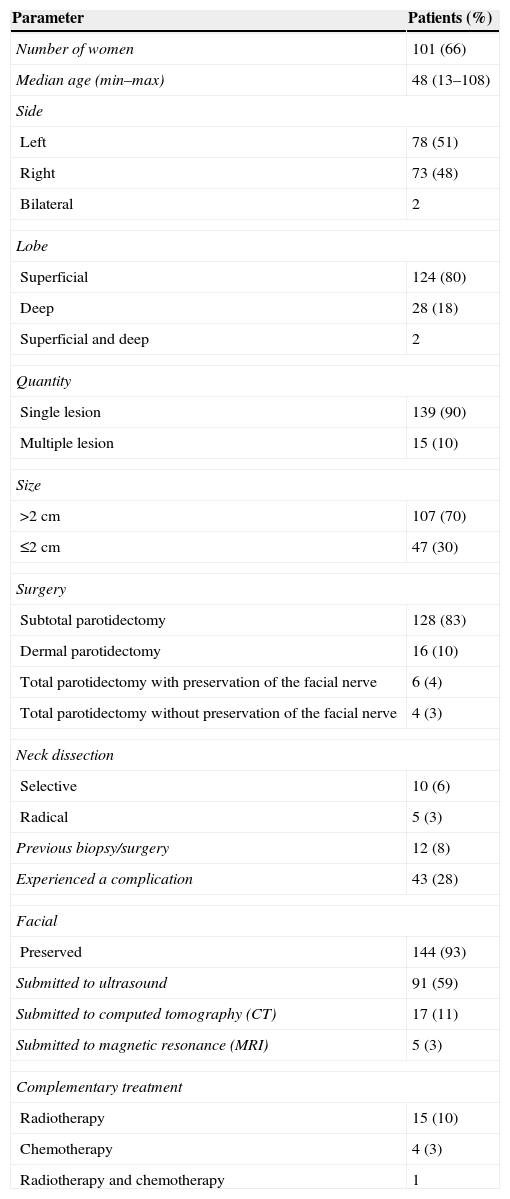
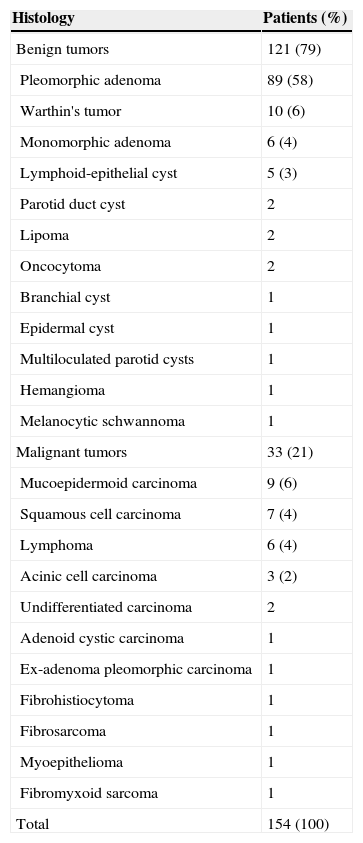
ResultsA total of 159 surgeries performed in 154 patients were selected between 1990 and 2011 (Table 1) and 124 benign and 35 malignant tumors (Table 2) were identified. Pleomorphic adenoma (92 cases) was the most frequent benign tumor and mucoepidermoid carcinoma was the most frequently identified malignant tumor (nine cases). As for the initial presentation, the main finding was a tumor mass in 94.9% of all cases reported in the study. Other presentations were an incidental lesion on imaging studies, and local pain, or inflammation. The median of pre-diagnostic clinical outcome for benign tumors was 12 months and for malignant tumors, five months. The most relevant clinical characteristics of the benign and malignant tumors are shown in Table 3.
Demographic analysis of the sample.
| Parameter | Patients (%) |
|---|---|
| Number of women | 101 (66) |
| Median age (min–max) | 48 (13–108) |
| Side | |
| Left | 78 (51) |
| Right | 73 (48) |
| Bilateral | 2 |
| Lobe | |
| Superficial | 124 (80) |
| Deep | 28 (18) |
| Superficial and deep | 2 |
| Quantity | |
| Single lesion | 139 (90) |
| Multiple lesion | 15 (10) |
| Size | |
| >2cm | 107 (70) |
| ≤2cm | 47 (30) |
| Surgery | |
| Subtotal parotidectomy | 128 (83) |
| Dermal parotidectomy | 16 (10) |
| Total parotidectomy with preservation of the facial nerve | 6 (4) |
| Total parotidectomy without preservation of the facial nerve | 4 (3) |
| Neck dissection | |
| Selective | 10 (6) |
| Radical | 5 (3) |
| Previous biopsy/surgery | 12 (8) |
| Experienced a complication | 43 (28) |
| Facial | |
| Preserved | 144 (93) |
| Submitted to ultrasound | 91 (59) |
| Submitted to computed tomography (CT) | 17 (11) |
| Submitted to magnetic resonance (MRI) | 5 (3) |
| Complementary treatment | |
| Radiotherapy | 15 (10) |
| Chemotherapy | 4 (3) |
| Radiotherapy and chemotherapy | 1 |
Histological assessment of parotid tumors.
| Histology | Patients (%) |
|---|---|
| Benign tumors | 121 (79) |
| Pleomorphic adenoma | 89 (58) |
| Warthin's tumor | 10 (6) |
| Monomorphic adenoma | 6 (4) |
| Lymphoid-epithelial cyst | 5 (3) |
| Parotid duct cyst | 2 |
| Lipoma | 2 |
| Oncocytoma | 2 |
| Branchial cyst | 1 |
| Epidermal cyst | 1 |
| Multiloculated parotid cysts | 1 |
| Hemangioma | 1 |
| Melanocytic schwannoma | 1 |
| Malignant tumors | 33 (21) |
| Mucoepidermoid carcinoma | 9 (6) |
| Squamous cell carcinoma | 7 (4) |
| Lymphoma | 6 (4) |
| Acinic cell carcinoma | 3 (2) |
| Undifferentiated carcinoma | 2 |
| Adenoid cystic carcinoma | 1 |
| Ex-adenoma pleomorphic carcinoma | 1 |
| Fibrohistiocytoma | 1 |
| Fibrosarcoma | 1 |
| Myoepithelioma | 1 |
| Fibromyxoid sarcoma | 1 |
| Total | 154 (100) |
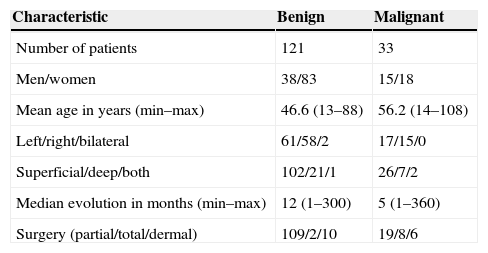
Clinical characteristics of benign and malignant tumors.
| Characteristic | Benign | Malignant |
|---|---|---|
| Number of patients | 121 | 33 |
| Men/women | 38/83 | 15/18 |
| Mean age in years (min–max) | 46.6 (13–88) | 56.2 (14–108) |
| Left/right/bilateral | 61/58/2 | 17/15/0 |
| Superficial/deep/both | 102/21/1 | 26/7/2 |
| Median evolution in months (min–max) | 12 (1–300) | 5 (1–360) |
| Surgery (partial/total/dermal) | 109/2/10 | 19/8/6 |
The ratio between men and women for benign tumors was 1:2, while for malignant tumors it was 1:1. The median age for the presentation of benign tumors was 45 years and for malignant tumors, 59 years. Regarding the clinical examination, the accuracy of preoperative palpation to determine the affected lobe and to infer the histological type was analyzed. The identification of tumor depth on palpation was compared with the intraoperative diagnosis and showed a sensitivity of 95.2% and specificity of 66.7% in the diagnosis of tumors of the superficial lobe, while it showed a sensitivity of 64.3% and specificity of 96.8% for those in the deep lobe. In cases where palpation resulted in suspected superficial and deep involvement, the examination sensitivity was 100% and specificity was 98.7% compared to intraoperative diagnosis.
To evaluate the accuracy of clinical assumption of histological type, histological analysis was defined as the gold standard in the following categories: pleomorphic adenoma, benign non-pleomorphic adenoma, and malignant. Palpation identified cases of pleomorphic adenoma with a sensitivity of 92.1% and specificity of 76.9% to rule out other histological types. At the identification of benign tumors other than pleomorphic adenoma, palpation showed a sensitivity of 75% and specificity of 89.3% when ruling out other causes. As for the diagnosis of malignancy, palpation showed a sensitivity of 57.6% to identify malignant cases and specificity of 100%.
Following the diagnostic flow, FNA indication cases were reviewed. Forty-two patients underwent FNA, of which 66.7% were benign, as opposed to 26.2% malignant and 7% inconclusive findings. Considering the postoperative results of the histopathological assessment as the gold standard, FNA had a sensitivity of 90.9% to identify cases of malignancy and specificity of 87.1%. There were three inconclusive FNA reports, but all were benign at the histological assessment.
Regarding imaging studies, 17 CT and five MRI assessments were performed. Ultrasound was used in 91 cases and alterations were observed in 98.9% of the cases. The most common alteration at the ultrasound was the presence of solid lesion (77 cases), followed by cystic lesion (13 cases). The main solid pathologies were: pleomorphic adenoma (47 solid, two cystic, and one lesion without particularities), monomorphic adenoma (four solid lesions found in four tests), squamous cell carcinoma (4/5), mucoepidermoid carcinoma (4/4), lymphoma (4/4), acinar cell carcinoma (2/2), oncocytoma (2/2), and lipomas (2/2). The main cystic pathologies were: Warthin's tumor (four cystic findings in four tests), lympho-epithelial cyst (3/3), and parotid duct cyst (2/2).
The analysis of the surgical technique demonstrated a predominance of subtotal parotidectomies (83%), followed by dermal parotidectomies (10%), total parotidectomy with preservation of the facial nerve (4%), and finally, total parotidectomy without preservation of the facial nerve (3%). Fifteen cases of neck dissection (ten selective and five radical) were performed. The radical dissections were performed in one case of superficial parotidectomy, one case of total parotidectomy with preservation of the facial nerve, one case of total parotidectomy without preservation of the facial nerve, and two cases of dermal parotidectomy. Selective dissections were performed in two cases of superficial parotidectomy, two cases of total parotidectomy with preservation of facial nerve, two cases of total parotidectomy without preservation of the facial nerve, and four cases of dermal parotidectomy. The sensitivity and specificity of the intraoperative frozen section analysis, with permanent histology representing the gold standard to identify malignancy, was 66.7% and 99.1%, respectively.
In all, five patients underwent intentional facial nerve resection. None of these cases had undergone a previous hospital admission, but all had malignant histology: mucoepidermoid carcinoma (two cases), squamous cell carcinoma (one case), undifferentiated carcinoma (one case), and malignant fibrous histiocytoma (one case). As for the 16 dermal parotidectomies performed, most were mainly associated with a prior hospital admission; 13 cases (81.2%) had previous history of biopsy or surgery. The other three cases were dermal parotidectomy associated with malignant histology. Regarding complications, the main findings were: paralysis or transient paresis (21 cases), salivary fistula (six cases), Frey's syndrome (five cases), and permanent facial paralysis (five cases).
DiscussionKnowledge in parotid tumors is an essential tool for the surgeon at the time of diagnosis and treatment. The scientific literature includes some institutional experience in this matter, with most results indicating that benign tumors are the most frequent. The present study confirmed the prevalence of benign tumors in 81.4% of the population studied, close to the proportion reported in other studies, which demonstrate consensus regarding pleomorphic adenoma as the most frequent diagnosis of parotid tumors.1–3
As for malignancy, mucoepidermoid carcinoma and secondary metastases each represent 5% of the studied cases, and lymphoma, 4.3%. In 2002, Sungur found an equivalent proportion of malignant tumors, 17%, but reported adenoid cystic carcinoma as the primary malignant tumor in his sample. In 2008, studies showed a higher prevalence of mucoepidermoid carcinoma, equivalent to 3% of malignant tumors of the sample.3 Taking these results in consideration, we believe that both mucoepidermoid carcinoma and adenoid cystic carcinoma should be considered in cases of suspected malignancy of the tumor.
Mass palpation at parotid gland topography was the main manifestation at the physical examination in the study population, in 93.9% of cases, in agreement with the literature. There have also been isolated reports of incidental lesion in imaging exams, local pain, or referral from another specialist. Palpation is established as an excellent clinical parameter for topographic location and classification of lesions regarding malignancy, with proven significance in the sample through its high sensitivity for demonstrating nodules in the superficial lobe (95.3%) and high specificity for nodules in the deep lobe. Moreover, it showed a sensitivity of 92.3% for classification of nodules in pleomorphic adenoma and 100% specificity for classification of nodules compatible with malignancy. The mean evolution time of benign tumors was approximately three times greater than that of malignant tumors. These data agree with the clinical experience that malignant tumors are more aggressive and have fast evolution, whereas benign ones, in turn, have an insidious onset and slow growth.
Considering that clinical examination seems to be a good diagnostic method for benign tumors, it is understood that the indication of complementary diagnostic tests occurs predominantly in cases where there is suspicion of malignancy, which occurred in 27.3% of cases, in accordance with previous studies.1 Compared to postoperative anatomopathological results, FNA showed excellent sensitivity and specificity for the diagnosis of malignant tumors, especially when associated with appropriate assessment of clinical criteria associated with malignancy. In 2004, Bova et al. showed that FNA had significant sensitivity and specificity for malignant tumors in their sample4; however, another recent study from 2013 demonstrated through retrospective analysis that FNA is also a reliable method for preoperative analysis for benign tumors, with higher sensitivity and specificity not just for benign, but both than imaging tests. In the same study, the sensitivity and specificity associated with FNA was 85.7% and 99.5%, respectively, similar to the result of the 154 patients in this sample, 90.9% and 87.1%, respectively. The same trend was observed in the studied sample; i.e., imaging tests were requested only in cases where there was a significant suspicion of malignancy or involvement of adjacent structures, showing adequate sensitivity in these cases.5
Therefore, this sample was similar to recent studies regarding the request for additional tests. CT was utilized more frequently than MRI as it was a more accessible examination in Brazil, especially considering the years comprising this study. As for the surgical management of parotid tumors, both subtotal and total parotidectomy are safe procedures in experienced hands, with transient facial nerve paralysis representing the main complication, which appears less frequently in more conservative surgical procedures.6
This sample showed marked prevalence of subtotal parotidectomy (83.9%), in which lymph node resection was necessary in only 2.2% of cases. This is justified by a previously noted higher frequency of benign tumors, such as pleomorphic adenoma. Cases in which full parotidectomy was indicated had a conclusive malignant histopathological diagnosis in 75% of cases. When deciding the most appropriate surgical procedure, intraoperative frozen section evaluation showed high sensitivity (90.9%) and specificity (100%) for identifying malignancy in agreement with the literature, which indicates that it is a good method in this surgical choice.6
High specificity is desirable in an intraoperative examination, as it can reliably rule out malignancy, preventing unnecessary radical interventions. Another procedure that has been studied in the management of benign tumors is dermal parotidectomy, which according to Albergotti et al., 2012, in their meta-analysis, showed recurrence rates similar to superficial parotidectomy, albeit with lower incidence of major complications.7 In the present study, the choice of this procedure was mainly associated with cases of recurrence, and in 50% of cases, patients with a previous history of biopsy (performed at other services).
The most-feared postoperative complication after parotid surgery is facial paralysis, which occurs at a frequency of 20–40% in the literature, with only 4% of cases being definitive.6–8 The present study showed an incidence of 15% of cases with postoperative facial paralysis and only 1.9% of cases with permanent paralysis. Thus, it is concluded that cases of permanent paralysis are rare, and are associated with severe malignant cases with prior involvement of adjacent structures.
ConclusionsAccording to this study, considering the surgical team's experience, a single node in the parotid region is the main manifestation of cancer of the parotid gland. The pleomorphic adenoma is the most prevalent histological type and subtotal parotidectomy with facial nerve preservation is the best treatment for these patients. Definitive facial paralysis is justified only in cases of malignant neoplasms.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Maahs GS, Oppermann PO, Maahs LGP, Machado Filho G, Ronchi AD. Parotid gland tumors: a retrospective study of 154 patients. Braz J Otorhinolaryngol. 2015;81:301–6.
Institution: Universidade Federal do Rio Grande do Sul (UFRS), Porto Alegre, RS, Brazil.