Mucoceles are cystic formations lined with respiratory epithelium that contain a mucoid or mucopurulent fluid. Although benign, mucoceles are locally expansive, due to continuous production and accumulation of mucus, resulting in erosion and underlying bone remodeling. This may affect the orbit, skull base, or soft tissue of the face. Frontal, ethmoidal, and fronto-ethmoidal sinuses are the most common locations, while the, maxillary and sphenoidal sinuses are less frequently affected. Maxillary sinus mucoceles are rare, accounting for less than 10% of all mucoceles in the USA and Europe.1
Orbital symptoms are relatively common in patients with mucocele, due to the expansion of the lesion into the orbit.1 These symptoms are usually caused by ethmoidal, sphenoidal, and frontal mucoceles. Ophthalmologic impact is unusual from maxillary mucoceles. As to orbital symptoms, edema and periorbital pain are the most common findings. Amaurosis is the most feared complication, but fortunately it occurs with low frequency,2 and its occurrence in maxillary mucoceles is extremely rare.1–5
The objective of this study is to report a rare case of maxillary mucocele leading to amaurosis.
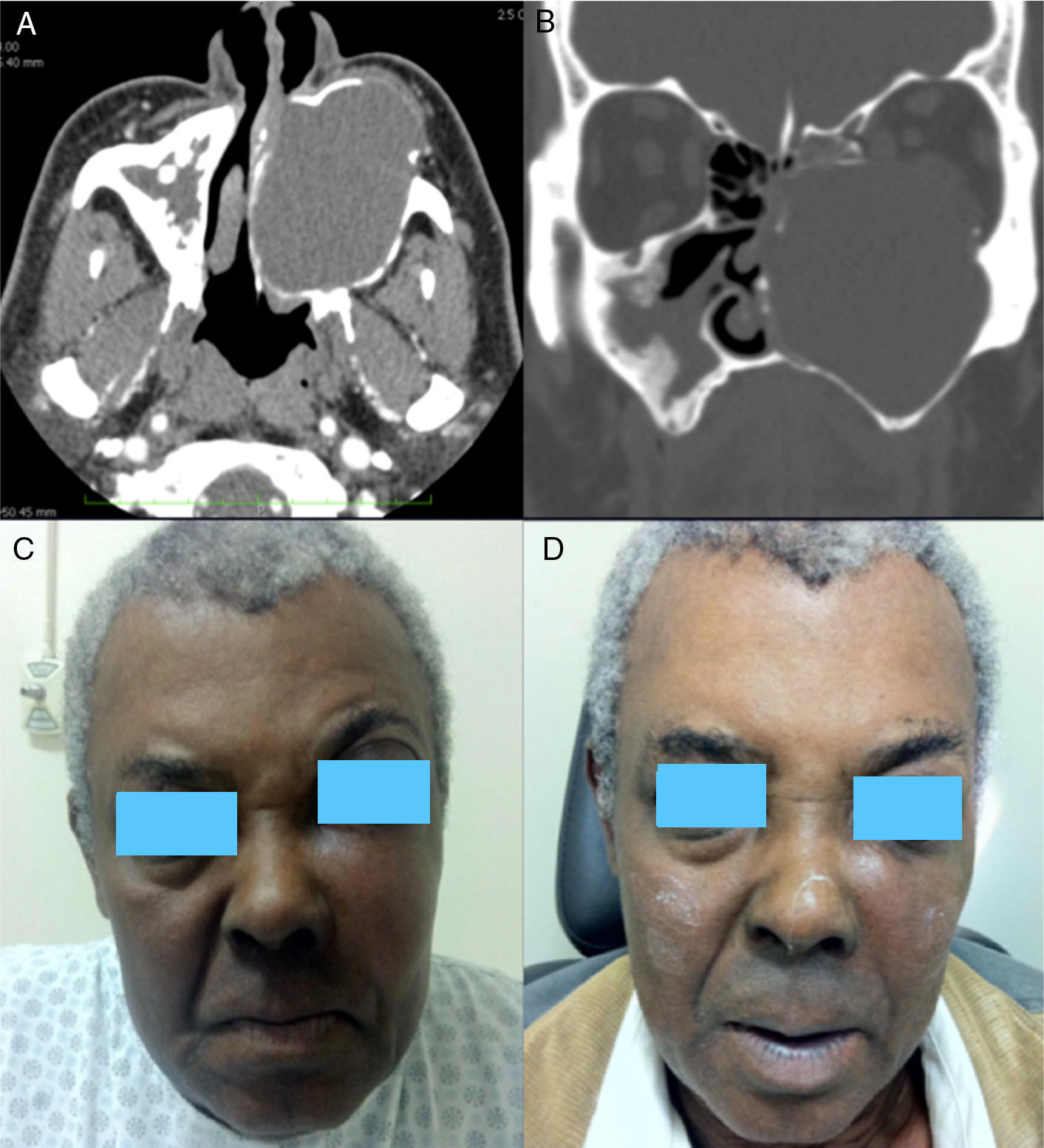
Case presentationThis report concerns a male patient, 67 years of age, with proptosis and a progressive bulging in left malar region, in association with a lasting continuous ipsilateral nasal obstruction/clear rhinorrhea. In about five months, his visual acuity began to decrease, accompanied by progressive eye pain on the left side. Clinical history revealed facial trauma 18 years in the past, hypertension and diabetes mellitus. Physical examination revealed left malar area deformity, with pain on palpation in association with ipsilateral proptosis. Nasal endoscopy showed medialization of the left lateral nasal wall, causing a complete occlusion of the nasal cavity. An ophthalmologic evaluation showed decreased left pupillary reflexes, visual acuity, and extraocular motility. Computed tomography of the paranasal sinuses showed an expansible lesion into the left maxillary sinus, with density compatible with soft tissue, with no contrast enhancement, and remodeling of the adjacent bone structure, suggestive of maxillary mucocele (Fig. 1).
(A) Computed tomography (CT) (axial section), showing an expansive lesion occupying the entire left maxillary sinus and promoting remodeling of bone limits. (B) CT (coronal section), showing an extension of the lesion to the orbital cone. (C) Preoperative picture showing bulging of the malar area and proptosis (left side). (D) Postoperative photography showing a clear improvement of bulging and proptosis.
The patient underwent maxillary mucocele marsupialization through nasal endoscopy by a wide maxillary middle meatal antrostomy, resulting in a profuse draining of a yellow-citrine fluid. In the immediate postoperative period (IPP), the case evolved with significant reduction of facial deformity and resolution of visual complaints. An ophthalmologic examination in the IPP revealed full recovery of visual acuity and extrinsic ocular motility; a few days later the patient showed improvement of pupillary reflex. A one-year follow-up showed that the patient remains asymptomatic, with a mild residual facial asymmetry and no other complaints.
DiscussionAmaurosis is the most serious orbital complication of any mucocele. The largest published series of cases of mucoceles with orbital involvement showed an incidence of 18.8% of amaurosis, when only patients with orbital involvement were considered.2 Smaller series have demonstrated variation from 6.7% to 40% for amaurosis, always considering only patients with orbital involvement.2–5 When all cases of mucocele were considered, lower occurrence of amaurosis has been reported, approximately 5%.2
Almost 30% of all mucoceles may erode toward the orbit, and the fronto-ethmoidal mucoceles are primarily responsible for this extension, followed by frontal and ethmoidal mucoceles.1 Maxillary mucoceles, in addition to being rare, seldom invade the orbit.1–5 Even in the face of an invasion, usually the only orbital symptoms are eye pain,3,5 proptosis,3 or diplopia.3 A report of amaurosis caused by maxillary mucocele occurred in a patient who had been subjected to skeletal surgery (Le Fort III), where this previous procedure, by fracturing the orbital floor and sinus, could have facilitated both the development of the mucocele and its extension toward the orbit.4 The patient of the present maxillary mucocele report was not involved with previous surgery, thus revealing a case of atypical development of a relatively rare disease.
Final considerationsThe authors report a patient with maxillary mucocele of atypical evolution, involving the orbit and leading to vision loss. Early diagnosis followed by an appropriate and prompt treatment can lead to immediate recovery of vision.
Conflict of interestsThe authors declare no conflict of interests.
Please cite this article as: Simões JC, Nogueira-Neto FB, Gregório LL, Caparroz FA, Kosugi EM. Visual loss: a rare complication of maxillary sinus mucocele. Braz J Otorhinolaryngol. 2015;81:451–3.
Institution: Rhinology Sector, Department of Otorhinolaryngology and Head and Neck Surgery, Escola Paulista de Medicina, Universidade Federal de São Paulo (EPM/UNIFESP), São Paulo, SP, Brazil.