Waldenström's macroglobulinemia (WM) is a low-grade lymphoma originally described in 1944.1 It is a malignant lymphoproliferative disease characterized by the clonal expansion of B cells with lymphoplasmacytic differentiation that secrete monoclonal immunoglobulin M (IgM). Diagnostic criteria are based on specific clinical, morphological, and immunophenotypic parameters, besides the evidence of pathologic plasmacytoid cells in the bone marrow. Symptoms can be related either to tumor infiltration or to the amount and properties of the circulating monoclonal protein: cardiac and renal failure, mucosal bleeding, headache, visual disturbances, ataxia, and eventually coma have been described as part of the clinical spectrum of WM. Peripheral neuropathy occurs in nearly half of the patients and is mostly related to the reactivity of the IgM protein with different neural antigens. Frequently, it represents the initial presentation of the disease; sometimes it could precede the diagnosis of macroglobulinemia by several years.2 Conversely, the onset of audio-vestibular symptoms and signs as a presenting phenomena of WM is unusual. This report presents an original case, the first ever disclosed in literature, of bilateral vestibular loss (BVL) as the presenting symptom of WM, and the relevant literature is reviewed.
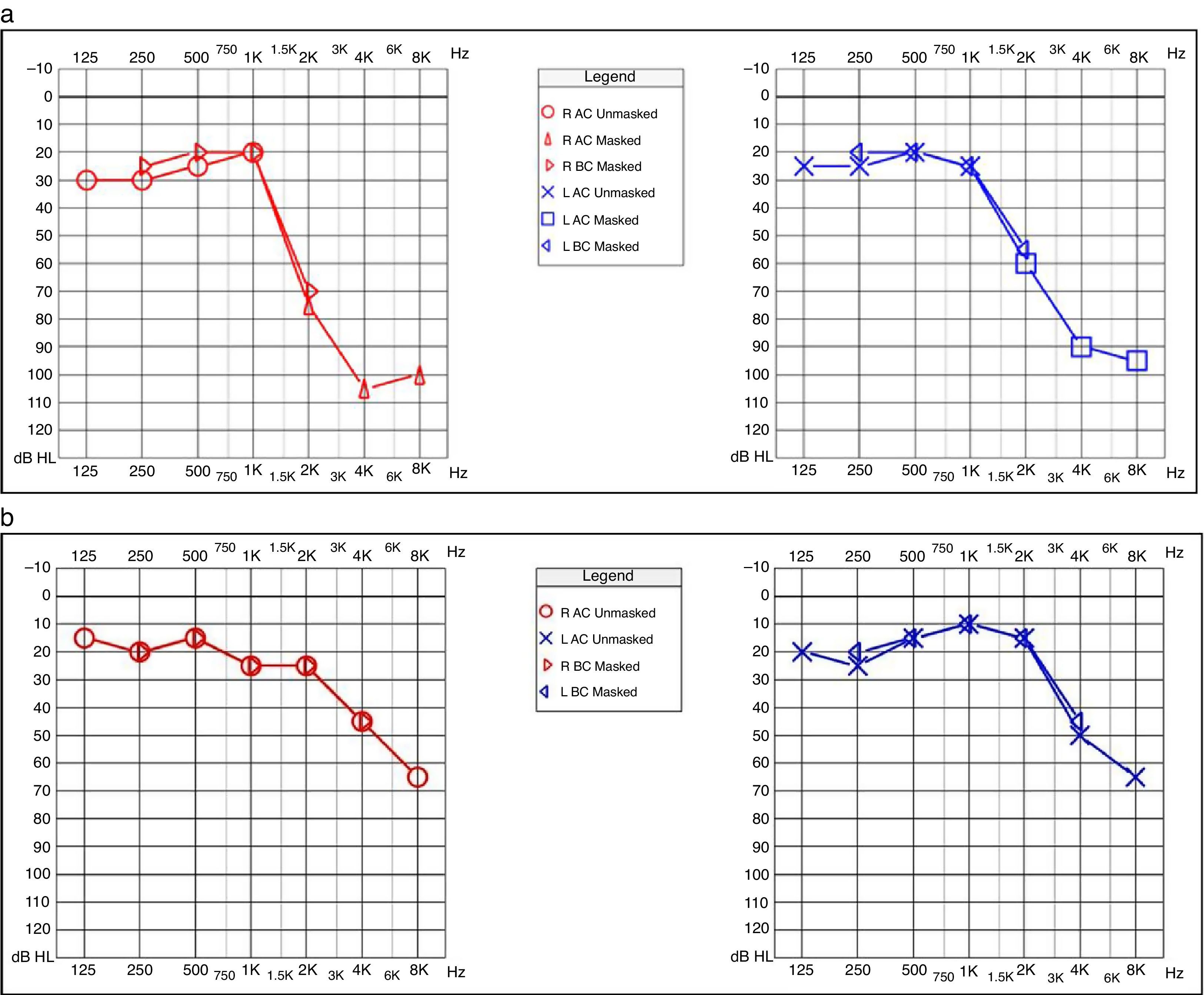
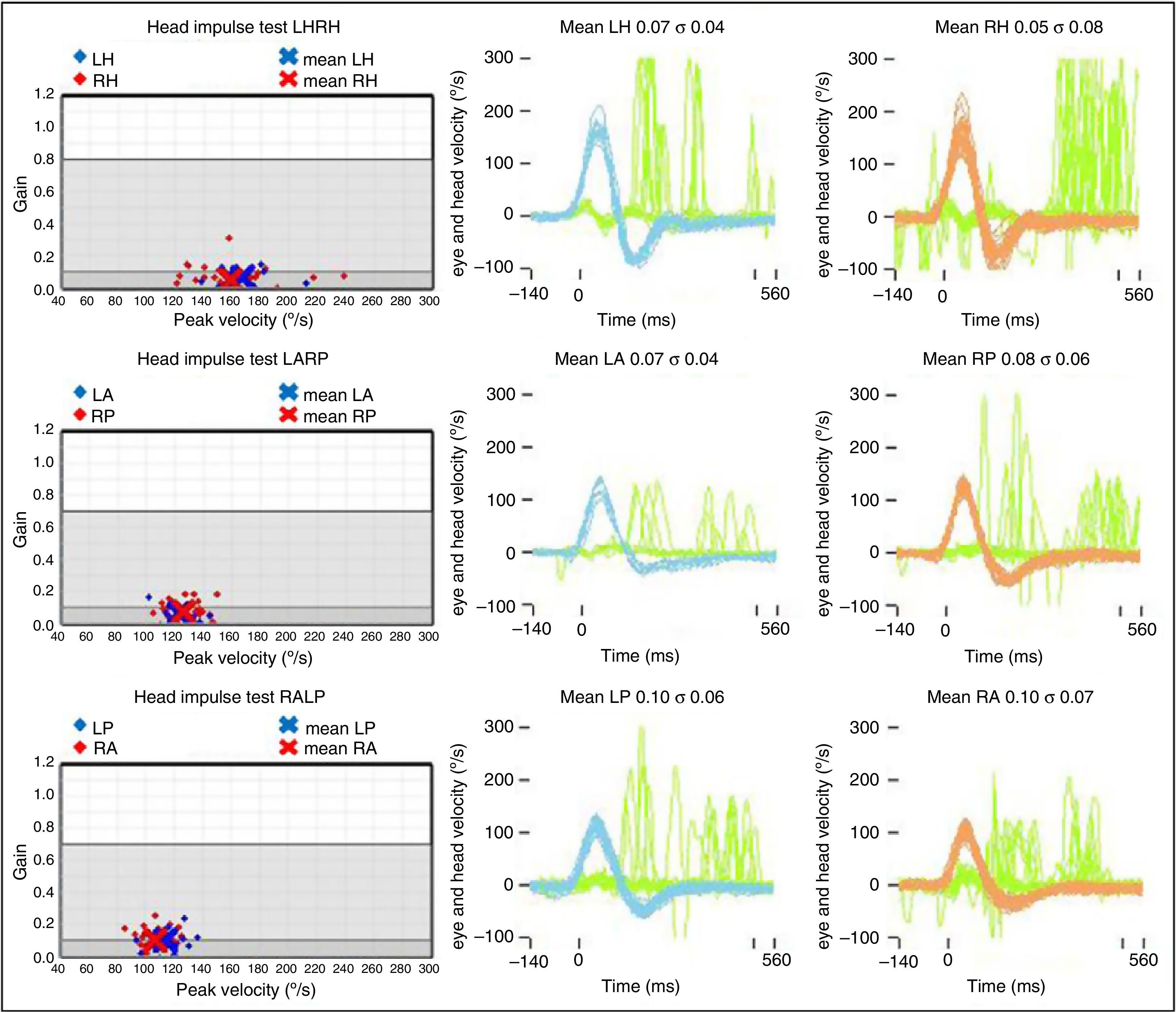
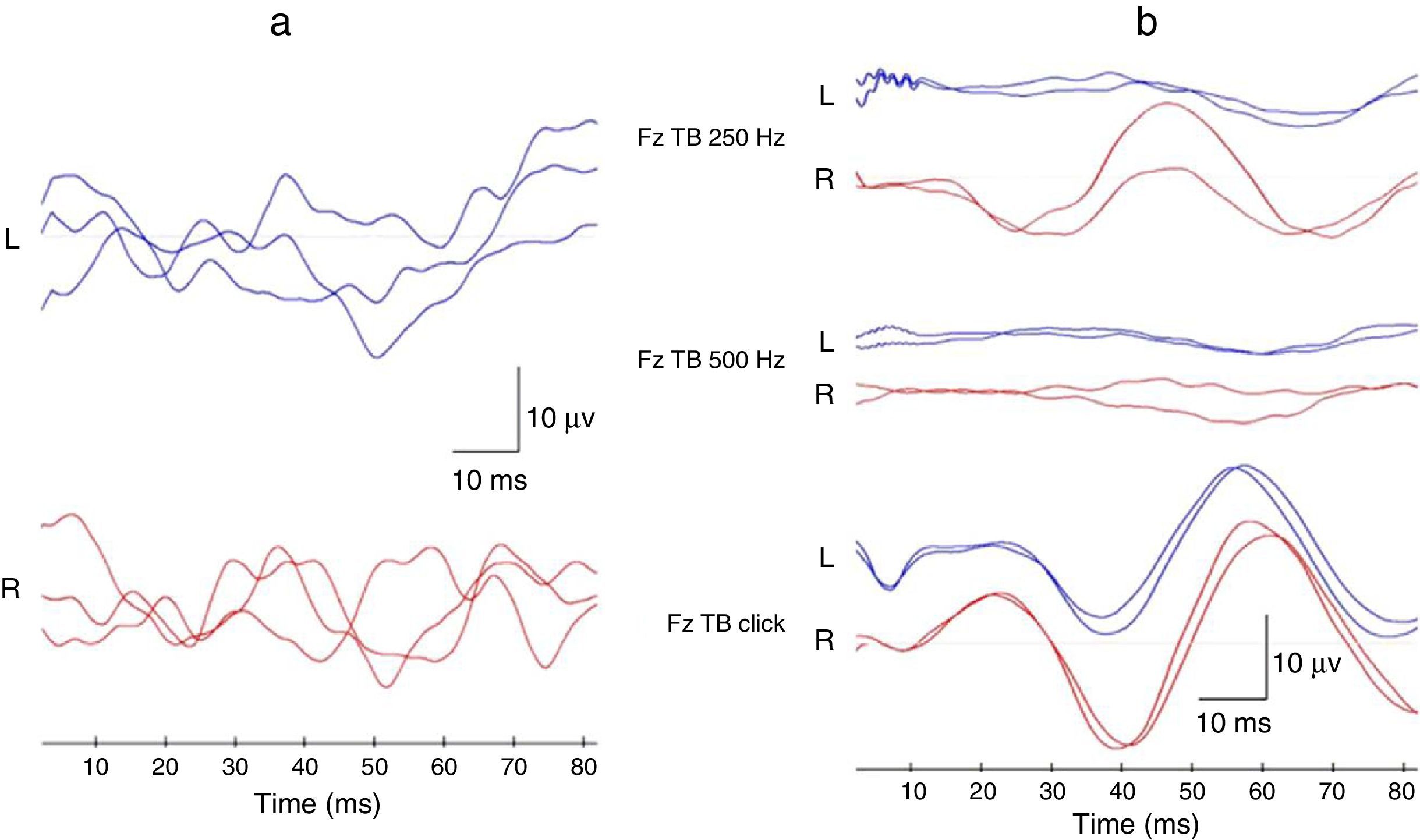
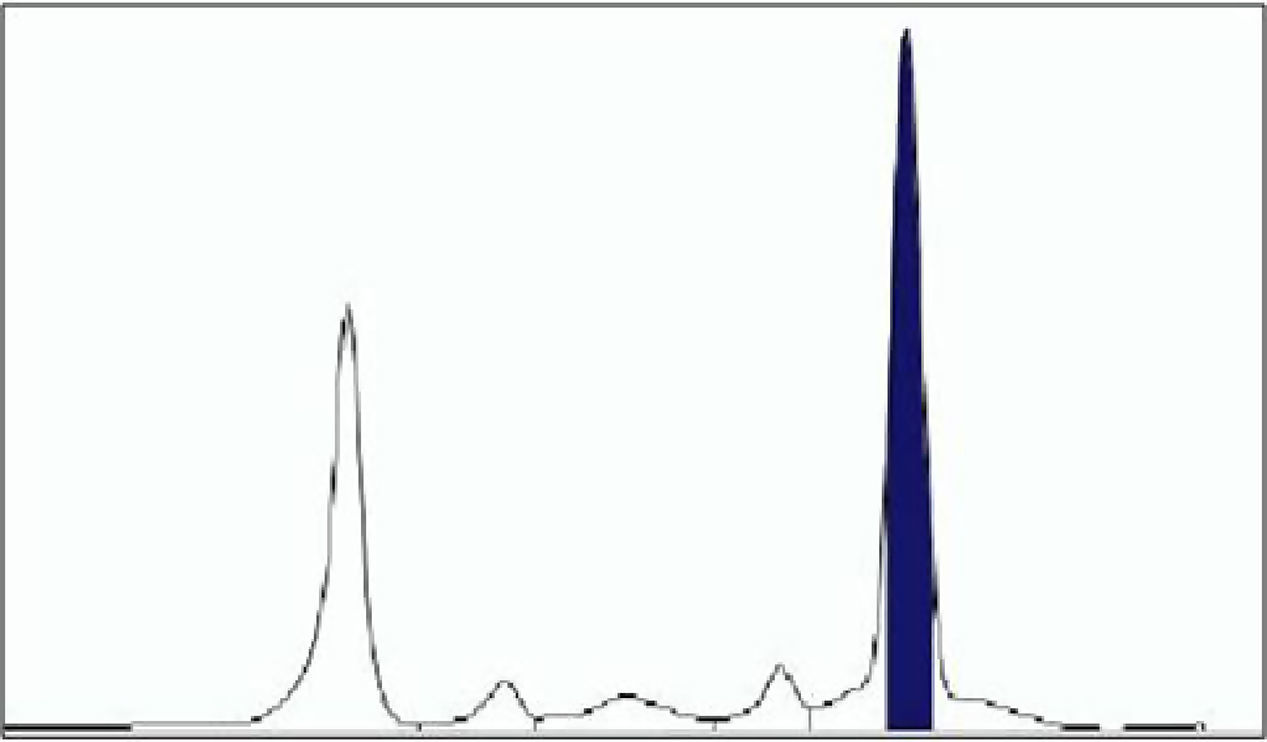
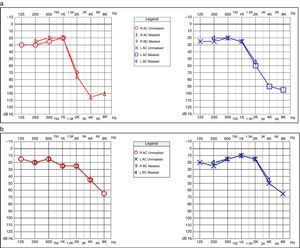
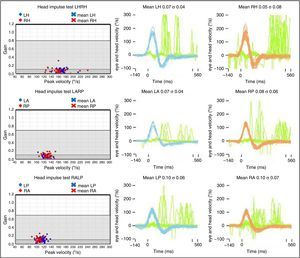
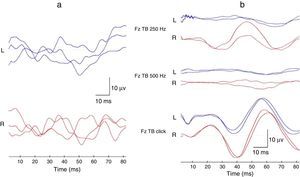
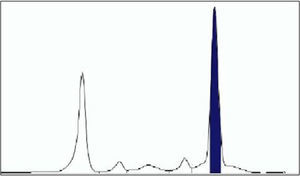
Case reportA 57-year-old woman presented at the hospital with the onset of asthenia, fatigue, progressive dizziness, and disequilibrium for a few months. Immediately before the symptoms began, she had already experienced positional vertigo spells while laying down or getting up from bed. Right posterior canal benign paroxysmal positional vertigo was diagnosed and treated successfully with two cycles of repositioning maneuvers at another institution. Since then, she had started to feel progressively unsteady, lightheaded, and even experienced oscillopsia while walking, becoming severely disabled during her daily activities. She also noticed a rapidly progressive bilateral hearing impairment and recurrent nasal bleedings. Surprisingly, she did not show any spontaneous or positional nystagmus at the infrared video-oculography, while audiometric test revealed a moderate-to-severe bilateral high-frequency sensorineural hearing loss (Fig. 1a). Subsequently, she was submitted to an extensive neuro-otologic assessment: standard bithermal caloric test showed minimal/absent caloric responses bilaterally. No response was elicited even after ice-water stimulation, proving bilateral deficient vestibulo-ocular reflex (VOR) at low-frequency range. High-frequency VOR gain for all six semicircular canals was tested with the video head impulse test (vHIT). VOR gain for each canal showed to be extremely deficient (Fig. 2). Saccular and utricular function was measured using air-conducted cervical vestibular evoked myogenic potentials (VEMPs) and bone-conducted ocular VEMPs, respectively. No reliable response could be detected bilaterally (Fig. 3). Temporal bone high-resolution computed tomography (CT) scan was negative and gadolinium-enhanced brain magnetic resonance imaging (MRI) excluded central nervous system (CNS) involvements. All principal causes of bilateral vestibular failure were excluded through an accurate anamnesis. The patient was submitted to a parallel internal medicine assessment, which detected signs of pulmonary arterial hypertension. Peripheral blood analysis revealed pancytopenia (WBC 2.78×109/L, RBC 3.32×1012/L, Hemoglobin 96g/L, HCT 30.1%, Platelets 94×109/L). Thus, she was submitted to the Hematologic Unit of the institution for further investigation. Serum protein electrophoresis revealed hypergammaglobulinemia with a homogeneous narrow and dense band migrating to the gamma region (Fig. 4), with an albumin/globulins ratio of 0.44. Quantitative testing for immunoglobulins showed abnormal serum levels of IgM paraprotein (92.71g/L) and serum immunofixation resulted positive for monoclonal component type IgM/kappa. Urine immunofixation test was positive for Bence Jones protein. She immediately underwent a bone marrow biopsy that demonstrated diffuse monoclonal lymphoplasmacytic infiltrate (IgM+, IgD-, CD20+, CD3-immunophenotype with non-paratrabecular pattern of infiltration and 15% residual bone marrow cellularity), confirming the diagnosis of WM. Residual physical examination proved substantially normal (including the lack of lymphadenopathies, purpura, and sensorimotor neuropathy) besides acrocyanosis and papilledema. To complete the diagnostic workup, the patient was then submitted to a total body CT scan that excluded organomegalies or lytic bone lesions. She was therefore scheduled for a combination therapy based on high-dose intravenous steroids and plasmapheresis. The patient was re-evaluated at the institution two months later, presenting with a partial normalization of blood cells analysis (WBC 4.45×109/L, RBC 3.66×1012/L, Hemoglobin 104g/L, HCT 33.1%, Platelets 114×109/L, IgM 32.5g/L, albumin/globulins ratio of 1.42). She felt relieved from fatigue and asthenia, and her audiometric test surprisingly showed a consistent improvement in high-frequency hearing thresholds bilaterally (Fig. 1b). Nevertheless, a further oto-neurologic assessment confirmed a persistent deficiency in her vestibular function.
Video head impulse test (vHIT) with an ICS Video-oculographic system (GN Otometrics A/S – Denmark) for all semicircular canals (LH: left horizontal, RH: right horizontal, LA: left anterior, RP: right posterior, LP: left posterior, RA: right anterior). Passive, unpredictable 5°–20°, 50°–250°/s, and 750°–5000°/s2 head impulses were delivered manually on the plane of the horizontal and vertical canals while the patient was asked to keep looking at an earth-fixed target. On the right, blue lines represent head impulses exciting left canals, red lines correspond to head impulses exciting right canals, and green lines represent eye movements induced by the activation of the vestibulo-ocular reflex (VOR) following each head impulse. For each canal, the corresponding mean value of VOR gains with related standard deviation (σ) is reported. Overt saccades can be easily detected. On the left, each dot represents the VOR gain (eye velocity/head velocity) for each impulse. VOR showed to be extremely deficient for all canals.
Vestibular evoked myogenic potentials (VEMPs) evaluated using an Epic Plus system (Labat s.r.l. – Mestre, Italy) with a two-channel averaging capacity. (a) Air conducted (AC) cervical VEMPs were evoked delivering tone burst (TB) via headphones with frequency 500Hz, duration 8ms, intensity 120dB SPL, and stimulation rate 5Hz. Upper blue lines correspond to myogenic responses recorded on the left sternocleidomastoid muscle (SCM), lower red lines represent responses recorded on the right SCM. (b) Bone conducted (BC) ocular VEMPs were assessed using three different sagittal (Fz) stimulations: TB 250Hz (duration 8ms, intensity 1.5V), TB 500Hz (8ms, 1.5V), and click (0.5ms, 1.0V), all delivered by a hand-held minishaker with an attached Perspex rod (type 4810 – Bruel and Kjaer P/L, Denmark), with intensity amplification modified through a power amplifier (type 2718 – Bruel and Kjaer). Blue lines represent responses recoded under patient's left eye; red lines correspond to responses recorded under the right eye. No reliable potentials could be detected at the SCM nor under the eyes, besides uncertain late responses after click stimuli.
BVL is a rare condition. Though its etiology often remains unknown, as in most studies the idiopathic form coincides with the largest group of patients,3,4 this disorder is thought to represent the final common expression of different pathologic conditions, including ototoxicity, bilateral endolymphatic hydrops, infections, tumors (cerebellar tumors, neurofibromatosis type 2), surgical procedures on the inner ear or on the VIII cranial nerves, and autoimmune disease.3,4 BLV typically manifests with chronic disequilibrium, gait ataxia, and oscillopsia while walking. Only a few case series and literature reviews report hematologic pathologies as a possible cause of BVL3,4 and, similarly, cochleo-vestibular symptoms appear to be an unusual presentation of hematological disorders.5 Nevertheless, several reports described audio-vestibular manifestations occurring in patients with WM. A direction-changing positional nystagmus has been explained through the effect of heavy globulins on the cupulae of the canals, resulting in a buoyancy mechanism.6 Conversely, hearing loss and various levels of vestibular impairment have been related to different pathologic processes occurring in WM, such as multiple hemorrhagic phenomena,7 small vessel thrombosis secondary to sudden release of clotting factors,5 and increased blood viscosity resulting in the obstruction of labyrinthine small vessels.8 Moreover, some reports have also described a symptomatic improvement with a reduction of blood hyperviscosity, mainly after plasmapheresis.5,6 Indeed, one of the most important consequences related to the rheological properties of circulating IgM pentameters is hyperviscosity syndrome (HS), which is a distinguishing feature of WM. Nevertheless, it is observed in only 10%–30% of patients with WM and it can be also seen in patients with other hematological disorders.9 It is the consequence of the abnormal size and increased blood concentration of the monoclonal protein, leading to an aggregation of red cells and an increased vascular resistance. This condition is responsible for the onset of typical symptoms, such as skin and mucosal bleeding, visual disturbance, a huge variety of neurological disorders, and cardiovascular manifestations.1,9 Once diagnosed, it must be treated, as it may lead to life-threatening consequences. The reason why particular organ sites, such as the eyes and the CNS, are more frequently involved than others in HS may be explained by the sluggish flow occurring in certain vascular beds, resulting in further enhancement of blood viscosity. Moreover, it is well known that the inner ear and the retina are similar in terms of vascularization, considering their peripheral location and their blood supply of terminal type. Therefore, it could be easily hypothesized that the same typical pathologic findings documented in the retina of patients with HS can likely occur in the labyrinth of the same subjects.8 On the basis of the abnormal level of serum IgM and the typical symptoms of HS, it is believed that the BVL detected in the present case could be likely explained on a vascular basis. In particular, serum hyperviscosity could have been responsible for obstruction of capillaries, resulting in anoxia of the peripheral vestibular end organ as demonstrated by the nearly absolute lack of responses after stimulation of all canals and maculae. Even the positional vertigo spells that occurred in the early stage of the disease could be explained by a sudden deficit of utricular perfusion. Detachment of otoliths due to an ischemic lesion of the utricular macula could have resulted in canalolithiasis of the still functionally active posterior canal. It could have represented the first premonitory sign of an incipient progressive vestibular anoxia, reinforcing the hypothesis of hyperviscosity as the basis of vestibular loss.
In contrast with most of the literature in which hearing loss usually prevails on vestibular symptoms in patients affected by WM,5,7 in the present case cochlear function was partially spared by hypoxia, with only a bilateral high-frequency hearing impairment.
Besides subjective anatomo-physiologic factors privileging cochlear versus vestibular microcirculation, the reason why mainly vestibular receptors have been affected by ischemia, with only a partial involvement of the basal turn of the cochlea, could be explained considering the anatomy of vascular inner ear supply. On the basis of scanning electron microscopic studies, a model for the vascular pathways in the labyrinth has been described, and therefore different clinical scenarios have been proposed depending on which arterial or venous branch could be involved by ischemia.10 According to this model, selective combined ischemia at the level of both vestibular anterior artery (supplying lateral and superior canal ampullae and utricular macula) and vestibulo-cochlear artery (feeding posterior canal ampulla, saccular macula, and cochlear basal turn) may represent the pathologic event responsible for the onset of the present symptoms, sparing vascular supply to the upper part of the cochlea. Similarly, blood stagnation at the level of the auditory internal vein in association with a blockage of the venous drainage from the lower part of the cochlea could result in the same clinical picture.
Finally, even more particular combinations among insufficient arterial flows and specific interruptions of the venous return could lead to anoxia of the same labyrinthine compartments and therefore to damage of the same receptors.
ConclusionIn patients with a clinical picture consistent with BVL, even without evident systemic involvement, hematological disorders such as WM should always be considered as underlying causative factors. It is important for neuro-otologists to consider HS in differential diagnosis of cochleo-vestibular symptoms and signs, as it could lead even to life-threatening consequences. Similarly, hematologists should be aware of the possibly of irreversible damages on sensorineural end organs, such as the inner ear, caused by the extremely high levels of IgM and HS. In fact, thanks to its particularly high sensitivity, the inner ear could be an early detector of systemic pathological manifestations as shown in this unique case report. Moreover, subclinical alterations of cochleo-vestibular function could occur more frequently in patients with WM. Therefore, a systematic neuro-otologic assessment should be promptly suggested in such cases, in order to prevent labyrinthine hypoxia and eventually to adopt appropriate therapeutic strategies.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Castellucci A, Piras G, Brandolini C, Modugno GC, Ferri GG. Waldenström's macroglobulinemia presenting with bilateral vestibular loss: a case report. Braz J Otorhinolaryngol. 2015;81:571–5.