Extraskeletal osteosarcoma (ESOS) is a rare malignant soft tissue sarcoma with a histological similarity to primary bone osteosarcoma but not attached to bone or periosteum.1–9 It accounts for 1% of all soft tissue sarcomas and about 4% of osteogenic osteosarcomas.1,2,6,8 Since first described by Wilson in 1941,10 only several major series have been published.3,8 Although tumor of advanced age group, the average median age group is 60.1–9 In the literature, studies are emphasizing male dominance equally or female dominance.2,3,5,8 Extraskeletal osteosarcoma is a very rare subtype that makes up 4%–5% of all osteosarcomas.1–9 The lower extremity, shoulder girdle, upper extremity, and retroperitoneum, especially the thigh and hip, are the most common places for ESOS;1–9 these tumors are rarely seen in the head and neck region.1–3,5–7 Only 6%–10% of patients present with tumors in the head and neck area; in such cases, the mandible and maxilla are the dominant places.1,2,5,6 In the literature, extraskeletal osteosarcoma from the parapharyngealarea has not been reported. Herein, the first case of ESOS originating from the parapharyngeal area is presented with the literature.
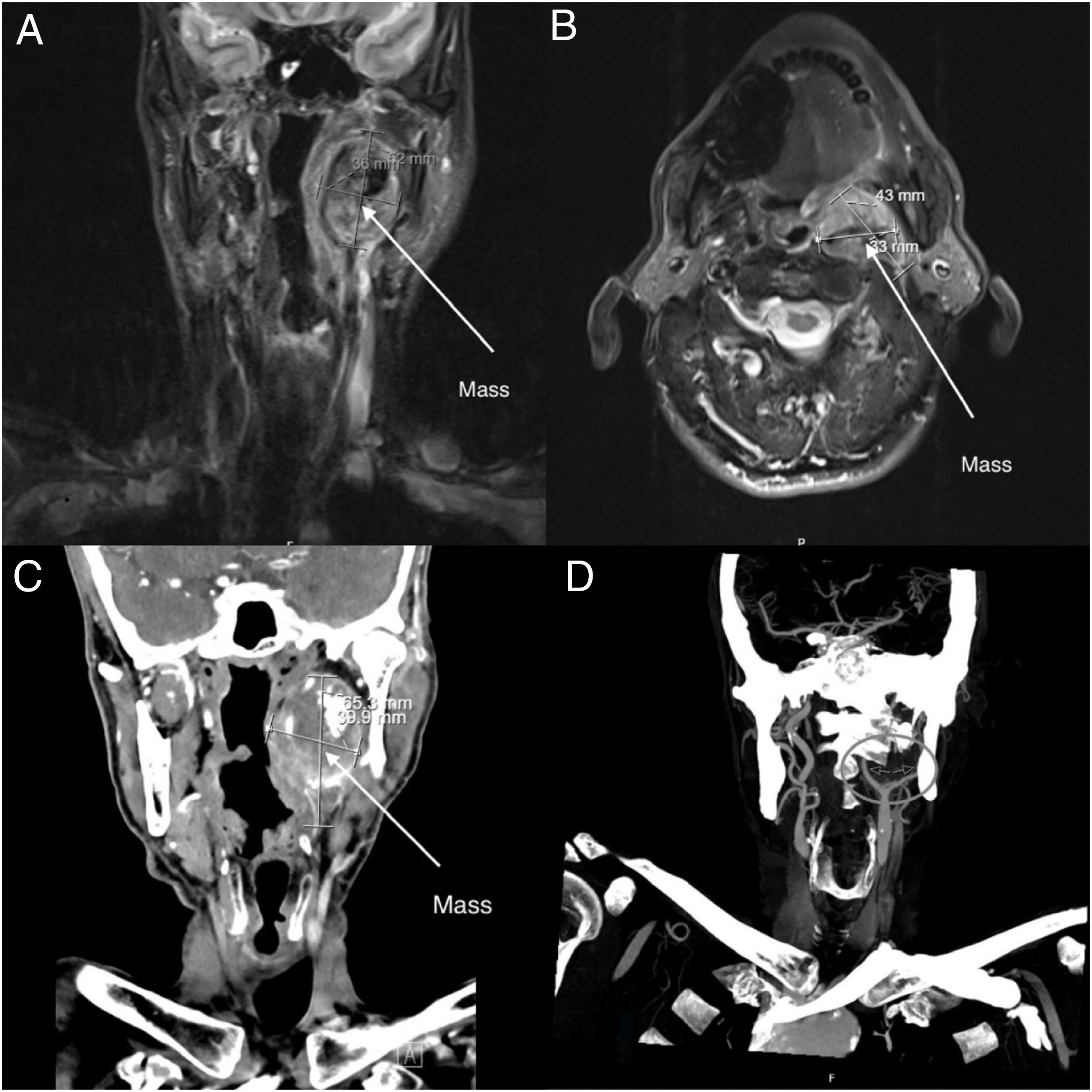
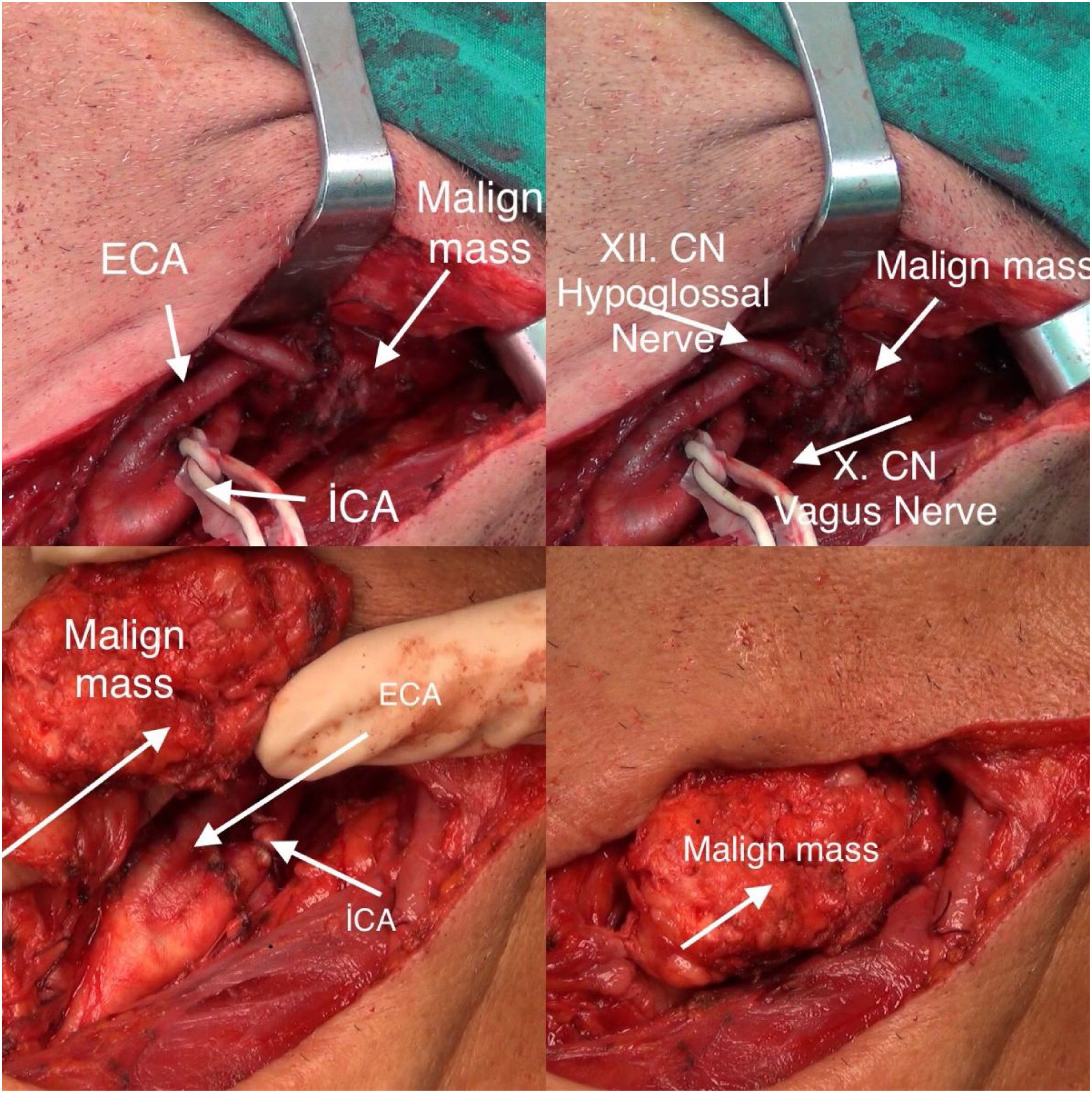
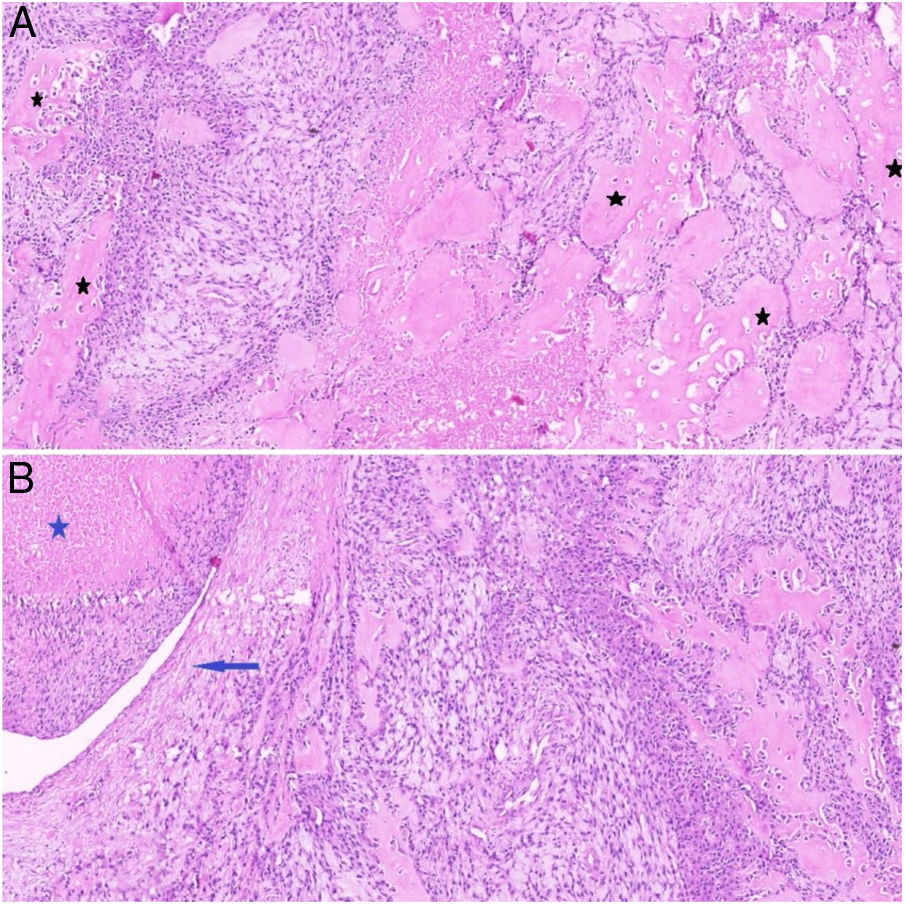
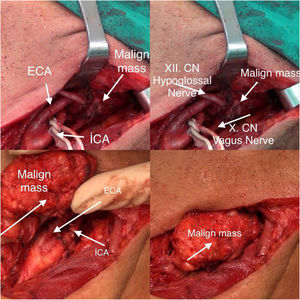
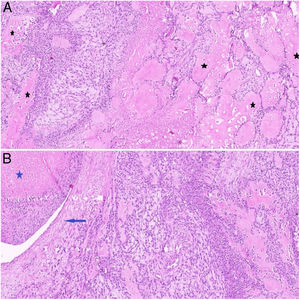
Case reportA 69-year-old male patient presented to our clinic with pain in the left parapharyngeal area, difficulty swallowing, disphagia, hoarseness, and speech impairment. Examination of the patient revealed a hard mass that was found upon deep palpation of the left parapharyngeal area. Also, the patient had displaced the left uvula medially on the oral cavity examination. The patient had left hypoglossal nerve palsy and the tongue was deviated to the left. Left vocal cord paralysis was present on the patient's endoscopic examination. In the medical history of the patient, there was no history of malignancy, radiation exposure, or family history of malignancy. In the radiological examination of the patient, on computerized tomography (CT), a mass in the left carotid artery bifurcation was present with dimensions of 5×3,5×3.5cm, with punctate calcifications and showing springiness between internal carotid artery (ICA) and external carotid artery (ECA) in the left parapharyngeal area, and considered as a paraganglioma at the foreground (Fig. 1). On magnetic resonance imaging (MRI) examination it was reported as a 52×36×33mm paraganglioma mass containing punctate calcified foci, which were thought to originate from left carotid bifurcation, which retained contrast in the left parapharyngeal area (Fig. 1). In carotid angiography; a weak feeding mass is observed from the ascending pharyngeal branch of the left ECA, and it was observed that the push, springiness, luminal irregularity-stenosis were observed in the mass ICA (Fig. 1). Fine needle aspiration cytology was not planned for the patient because of paraganglioma pre-diagnosis. During the surgical operation, it was observed that the internal carotid artery was invaded and surrounded by a malignant mass. During the dissection of the mass, the internal carotid artery was injured and it was observed that it was almost completely infiltrated with the mass. Therefore the internal carotid artery was ligated. Postoperatively, the patient did not develop stroke or neurological deficits. This situation was explained by the predominance of the contralateral internal carotid artery due to the long-term invasion and infiltration of the internal carotid artery by the mass. The mass was removed en-bloc. The desirable clean surgical margins could not be achieved, especially due to the invasion of the canal through which the internal carotid artery enters the skull base and the skull base mucosa limiting the mass. It was observed intraoperatively that the nerve vagus and nerve hypoglossus were invasioned by the malignant mass (Fig. 2). The patient had preoperative nerve vagus and nerve hypoglossus paralysis, so there was no change in his current dysphagia and dysphonia. The mass was sent to the pathology laboratory in 10% formaldehyde solution. The tissues were fragmented and irregular in appearance. The cut surfaces of the tissues were partially solid, partially hard and gritty. After routine tissue processing, sections of tissue embedded in paraffin were stained with hematoxylin and eosin (H&E). Microscopically, the tumor was characterized by new bone formation intermingled with atypical spindle and epithelioid cells (Fig. 3A and B). Immunohistochemically the tumor cells were stained with vimentin, CD99 and synaptophysin antibodies. There were no staining with CD34, CD31, PanCK, S-100 and alpha smooth muscle actin antibodies. The case was reported as osteosarcoma with the morphological and immunohistochemical findings. The primary tumor focus was investigated for osteosarcoma metastasis. No other tumor focus was detected radiologically. Thus, the case was accepted as ESOS with pathological and radiological findings. The patient was given a chemotherapy regimen containing ciplatin and adriamycin by medical oncology. The patient has been receiving chemotherapy for 6 months and remains alive. However, the surveillance expectation of medical oncology is low.
Extraskeletal osteosarcoma is a rare malignant soft tissue sarcoma with a histological similarity to primary bone osteosarcoma, but not attached to bone or periosteum.1–9 Extraskeletal osteosarcoma is very rare. The incidence of ESOS is so low that the annual incidence in a study conducted in Norway; it was expressed as 0.2 per million.3 It can develop secondary to radiation therapy.1,3,6,8 Reviewing the current literature, it can develop in the field receiving radiotherapy 10–15 years following treatment. In some publications, secondary development to trauma is mentioned.1,6,7 Extraskeletal osteosarcomata, are rarely seen in the head and neck region.1–3,5–7 When the current literature is reviewed, there is no case of ESOS of the parapharyngeal area. In this respect, our current case is the first study presented in the literature.
Fine needle aspiration cytology is diagnosed as malignant cytology in the diagnosis of ESOS and is generally inadequate about its natüre.6 Extraskeletal osteosarcoma has no radiologically specific findings. The most important point is that there is no bone or periosteal connection. Computerized tomography and MRI examinations were not specific, and mineralization was seen in less than a third of extraskeletal cases, and ossification was mature instead of immature osteoid and eccentric rather than central.7
There is no standardization of the treatment of ESOS. If it can be accepted today, it is a wide surgical resection.1–9 However, recently, multi-approach treatment modalities are recommended. However, the efficacy and use of chemotherapy and radiotherapy in these approaches are not completely clear. The use of chemotherapy/radiotherapy is not standardized due to the small number of patients and the results being different by the centers. Especially, the resection of ESOS in the head and neck region is quite difficult due to anatomical localization and the desired surgical margins cannot be achieved, which increases the importance of chemotherapy and radiotherapy. However, there is no consensus in the existing head and neck osteosarcomas about treatment. The average survival of patients with ESOS is between 25%–77%.1–9
ConclusionIn conclusion, we present this rare case, which is seen for the first time in the parapharyngeal area, for educational purposes.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.