Obstructive sleep apnea syndrome has a high prevalence among adults. Cephalometric variables can be a valuable method for evaluating patients with this syndrome.
ObjectiveTo correlate cephalometric data with the apnea-hypopnea sleep index.
MethodsWe performed a retrospective and cross-sectional study that analyzed the cephalometric data of patients followed in the Sleep Disorders Outpatient Clinic of the Discipline of Otorhinolaryngology of a university hospital, from June 2007 to May 2012.
ResultsNinety-six patients were included, 45 men, and 51 women, with a mean age of 50.3 years. A total of 11 patients had snoring, 20 had mild apnea, 26 had moderate apnea, and 39 had severe apnea. The distance from the hyoid bone to the mandibular plane was the only variable that showed a statistically significant correlation with the apnea-hypopnea index.
ConclusionCephalometric variables are useful tools for the understanding of obstructive sleep apnea syndrome. The distance from the hyoid bone to the mandibular plane showed a statistically significant correlation with the apnea-hypopnea index.
A síndrome da apneia do sono apresenta grande prevalência na população adulta. A cefalometria com análise das variáveis morfológicas pode ser um método valioso na avaliação de pacientes com essa síndrome.
ObjetivoCorrelacionar dados cefalométricos com o índice de apneia-hipopneia do sono, com a finalidade de detectar fatores preditores para a gravidade da síndrome da apneia obstrutiva do sono.
MétodosTrata-se de um estudo retrospectivo, em que foram analisadas cefalometrias de pacientes em acompanhamento no ambulatório de distúrbios do sono da disciplina de Otorrinolaringologia, de um hospital universitário terciário, no período de junho de 2007 a maio de 2012.
ResultadosForam avaliados 96 pacientes, sendo 45 homens e 51 mulheres. Onze pacientes eram portadores de roncopatia, 20 de apneia leve, 26 de apneia moderada e 39 de apneia grave. A única variável cefalométrica que apresentou correlação estatisticamente significante com o índice de apneia e hipoapneia foi a distância linear perpendicular do osso hioide ao plano mandibular.
ConclusãoAs variáveis cefalométricas podem ser úteis no entendimento da síndrome da apneia obstrutiva do sono e uma atenção deve ser dada à variável que mede a distância do hioide perpendicularmente ao plano mandibular.
The obstructive sleep apnea syndrome (OSAS) is characterized by pauses in breathing during sleep, micro-arousals and daytime sleepiness. These symptoms are caused by repeated episodes of obstruction at one or more upper airway levels during sleep.1
This syndrome has a high prevalence in the adult population, affecting 4% of men and 2% of women.1 Affected patients have a higher risk of cardiovascular disease, motor vehicle accidents due to daytime sleepiness and may present a significant decline in neurocognitive function.2The pathogenesis of OSAS has been investigated through several structural and physiological methods.3 An increase in pharyngeal collapse has been postulated as a factor of OSAS physiopathology. Furthermore, it is known that craniofacial abnormalities and soft tissue characteristics are involved in upper airway patency. However, it is unclear how much the morphology of the craniofacial skeleton and soft tissue characteristics may affect the pharyngeal collapse and contribute to episodes of apnea. Therefore, the etiological significance of the association of the craniofacial skeleton and soft tissues of the oropharynx in OSAS is still controversial.3–8In this context, cephalometry and 3D-CT scanning can assess craniofacial skeleton abnormalities and the characteristics of oropharyngeal soft tissues. Although cephalometry has a limited two-dimensional view, it is asimple and affordable assessment method with less radiation exposure than computed tomography.3–6A meta-analysis of cephalometric studies, reported by Miles et al.,9 showed the most relevant variables that may be associated with the development and severity of OSAS: the angle between the anterior cranial base and the maxilla (SNA), the angle between the anterior cranial base and the mandible (SNB), the posterior airway space (PAS), the length of soft palate (PNS-P), and the distance from the hyoid bone to the mandibular plane (MP-H). Other studies have also stressed the importance of cephalometric variables in sleep apnea.10–12
Many studies have used cephalometric variables, usually associated with data from endoscopic evaluation to assess OSAS development. Although facial skeleton disorders and soft tissue alterations in the oropharynx are described in OSAS patients, any direct association is unclear, and it is still debatable whether the analysis of these cephalometric morphological variables can be a tool in the assessment of patients with OSAS.13A better understanding of the etiology and physiopathology of OSAS is extremely important to the selection of the most appropriate treatment. Several therapies have been proposed and studiedincluding the use of an intraoral appliance (IOA), skeletal surgery and soft tissue surgery, as well as a continuous positive airway pressure (CPAP) device.14,15 In some studies cephalometry has been given an important role in therapeutic decision-making in selecting from various skeletal surgery techniques.16–18
This study aimed to evaluate possible correlations between cephalometric data and the severity of the apnea-hypopnea index (AHI).
MethodsWe performed a retrospective, cross-sectional study, in which medical records of 381 patients treated at the Sleep Disorder Outpatient Clinic of the Discipline of Otorhinolaryngology, Head and Neck Surgery of a tertiary university hospital were assessed between June 2007 and May 2012. The following parameters were analyzed: gender, age, AHI, body mass index (BMI) and cephalometric data. Of the total number of selected patients, those with incomplete data, with no cephalometry data and younger than 18 years were excluded. Thus a total of 96 patients remained in the study.
Patients were divided into four groups according to AHI demonstrated by polysomnography: snoring (group 1), mild OSAS (group 2), moderate OSAS (group 3) and severe OSAS (group 4).
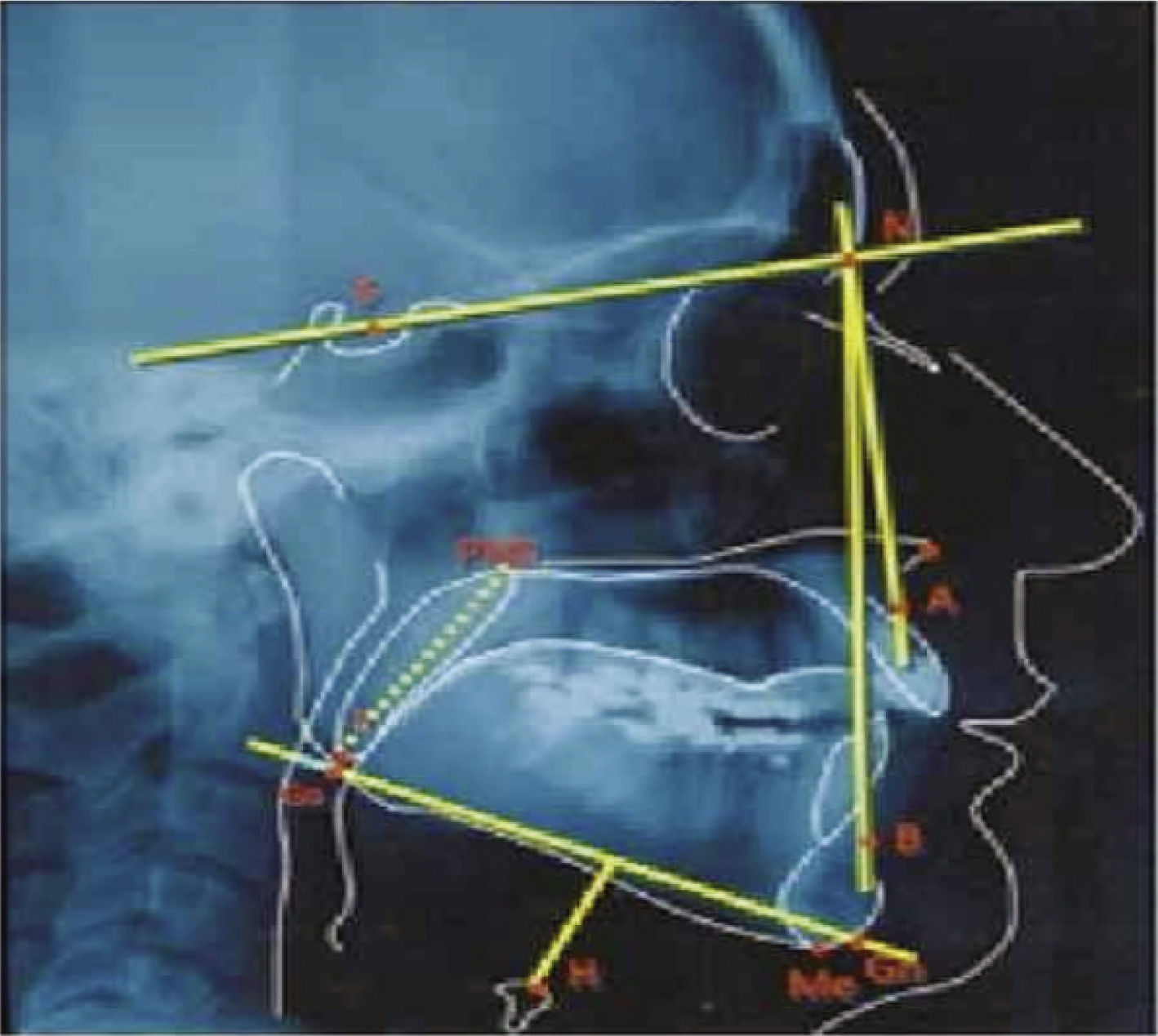
Teleradiography (Fig. 1) was considered adequate if performed in a lateral view, with the head in a natural position and barium contrast at the base of the tongue. The following measures were assessed through the cephalometric analysis:
SNA: Angle formed between the point sella, nasion and point A. This angle shows the position of the maxilla relative to the anterior cranial base. Therefore, it defines the degree of protrusion or retrusion of the maxilla in the anteroposterior direction. Reference value (RV): 82°.19
SNB: Angle formed between the point sella, nasion and point B. The magnitude of this angle indicates the position of the mandible relative to the anterior cranial base. Thus, it demonstrates the degree of protrusion or retrusion of the mandible in the anteroposterior direction. Reference value (RV): 80°.19
PAS: Lower pharyngeal space related to retrolingual airspace. Linear distance between a point on the base of the tongue and another point on the posterior pharyngeal wall, both determined by the length of the B-Go line. Reference value (RV): Men – 19mm/ Women–15mm.19
PNS-U: Soft palate length, measured from the posterior nasal spine (PNS) to the tip of the uvula (U). Reference value (RV): Men – 34mm/ Women – 35mm.19
Mp-H: Linear distance along a perpendicular line from point H to the mandibular plane (Mp). Reference value (RV): Men – 19mm/ Women– 15mm.19
Data were statistically analyzed using the SAS System, release 9.2, and Tukey's statistical test was used to compare the means of variables between groups, with p<0.05 being considered statistically significant.
This research was previously approved by the Research Ethics Committee of the institution, under the number 83946.
ResultsA total of 96 patients were evaluated: 45 men and 51 women, with a mean age of 50.3 years (range of 18 to 72 years). Eleven patients had snoring, 20 mild OSAS, 26 moderate OSAS, and 39 had severe OSAS. The male/female ratio remained homogeneous in the subgroups.
The mean BMI in all groups was 28.8kg/m2 and the distribution between the groups was as follows: snoring group, mean BMI: 25.04kg/m2; mild OSAS, mean BMI: 28.9kg/m2; moderate OSAS, mean BMI: 28.36kg/m2, severe OSAS, mean BMI: 30.2kg/m2.
The SNA, SNB and PAS values showed no statistically significant correlation with AHI. PNS-P values, although higher in patients with moderate and severe apnea than in snoring and mild OSAS, were not statistically significantly different. The analysis of MP-H values, on the other hand, showed greater length values in groups 3 and 4 than in groups 1 and 2, and these data are statistically significant (p<0.01) (Table 1).
DiscussionIn the medical literature, several predictors of OSAS have been identified and studied, including: obesity (increased body mass index), older age, increased cervical and abdominal circumference, in addition to the craniofacial disposition and pharyngeal soft tissues.3,19,20
These predisposing and/or etiological factors of OSAS have been extensively investigated by polysomnography, flexible nasal endoscopy, sleep-endoscopy and cephalometry. However, even with the use of all available methods, the precise identification of the airway obstruction site is limited because of the inability to reproduce the sleep state in awake patients.21
It is known that airway patency is influenced by craniofacial configuration, pharyngeal soft tissue characteristics and pharyngeal muscle contraction. There are two hypotheses that attempt to explain upper airway collapse: the neural hypothesis, which implies reduction of the oropharyngeal dilator muscle activity, and the anatomical theory which explains the collapse through the relationship of boney anatomy and soft tissues relaxation during sleep. Deposits of cervical fat may also contribute to the reduction of airway patency.22
Therefore, the structural relationships of the craniofacial skeleton and pharyngeal soft tissue may contribute to airway compromise.
After a comprehensive review, Miles et al.9 indicated that a direct and causal association between the relationship of craniofacial structures and the presence and severity of OSAS is very difficult to find in the literature. In this context, several studies have attempted to establish such a direct association between cephalometric measurements, and the presence and severity of OSAS.3–8 Sforza et al.22 demonstrated that the cephalometric variables that measure the length of the soft palate (PNS-P) and the distance from the hyoid perpendicular to the mandibular plane (MP-H) were associated with the presence of OSAS. Riha et al.23 described a lower position of the hyoid, and found that an increase in MP-H was associated with the presence of OSAS. Partinen et al.24 also found an association of the posterior airway space (PAS) and the distance from the hyoid bone perpendicular to the mandibular plane (MP-H) with OSAS.
Although all these studies have shown an association between variations in cephalometric measurements and the presence of OSAS, few studies have correlated these variables with disease severity, as we did in the present study. This issue remains minimally addressed in the national specialized literature.
In our series, the analyzed cephalometric variables were SNA, SNB, PAS, PNS-U and MP-H. The values of the SNA, SNB, PAS and PNS-U showed no significant correlation with AHI. In agreement with the studies mentioned above, in our study the only variable that correlated with OSAS severity was MP-H. Therefore, attention should be given to the increased distance from the hyoid bone (MP-H), as the muscles of the tongue are partially anchored to the hyoid bone and their height can influence the relationship of soft tissues in the oropharynx.25
One might think that this finding would be more consistent if it were associated with decreased posterior airway space (PAS), which did not occur in our sample. However, our data were collected from teleradiographs obtained during the wakened state;during sleep in sleep the location of the hyoid bone is lower-than-normal, and the base of the tongue assumes a more vertical positionthat would facilitate pharyngeal collapse. However, measured values of MP-H in the literature exhibit some variability perhaps reflecting an imbalance between the action of the supra-hyoid and infra-hyoid muscles and the amount of cervical fat deposition.22In this paradigm, there are many possible explanations for the difficulty of directly associating cephalometric variables with OSAS severity. First, cephalometry is obtained while the individual is awake and standing, which does not reflect changes that occur during sleep with the subject lying down and with relaxed pharyngeal muscles. Second, cephalometry provides information on the anteroposterior pharyngeal dimensions, but not on the laterolateral dimensions and recent studies with magnetic resonance imaging showed a reduction in lateral pharyngeal space in OSAS patients when compared with snoring patients only. Finally, it is possible that the configuration of the upper airway which is elliptical, may predispose to pharyngeal collapse during sleep and this configuration may be be more important than the absolute size of the airway.22–24
Thus, our study suggests that while there may be a recognizable cephalometric predisposition for sleep-disordered breathing, this is only one of many aspects involved in the physiopathology of OSAS. Future studies should be performed to provide more information about the influence of anatomical variables on upper airway collapsibility.
ConclusionThe cephalometric variables are useful tools for understanding OSAS. The distance from the hyoid bone to the mandibular plane (MP-H) showed a statistically significant correlation with AHI.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Silva VG, Pinheiro LAM, Silveira PL, Duarte ASM, Faria AC, Carvalho EGB, et al. Correlation between cephalometric data and severity of sleep apnea. Braz J Otorhinolaryngol. 2014;80:191-5.
Study conducted at the Outpatient Clinic of Sleep Disorders of the Discipline of Otorhinolaryngology, Head and Neck, Faculdade de Ciências Médicas, Universidade Estadual de Campinas (UNICAMP), Campinas, SP, Brazil.