Intravascular papillary endothelial hyperplasia – known as Masson's tumor – is a rare benign entity. It was first described in 1923 by a French pathologist under the name hémangioendothéliome végétant intravasculaire.1 It is currently considered a reactive intravascular proliferation that develops either in a dilated vessel's lumen, a hematoma or a preexisting vascular lesion.2,3 No malignant degeneration has been yet reported. We present three cases of Masson's tumor of the maxillary sinus, which were all treated with endoscopic surgery and initially considered potentially malignant. A literature review of other cases found in the paranasal sinuses and nasal cavity is presented.
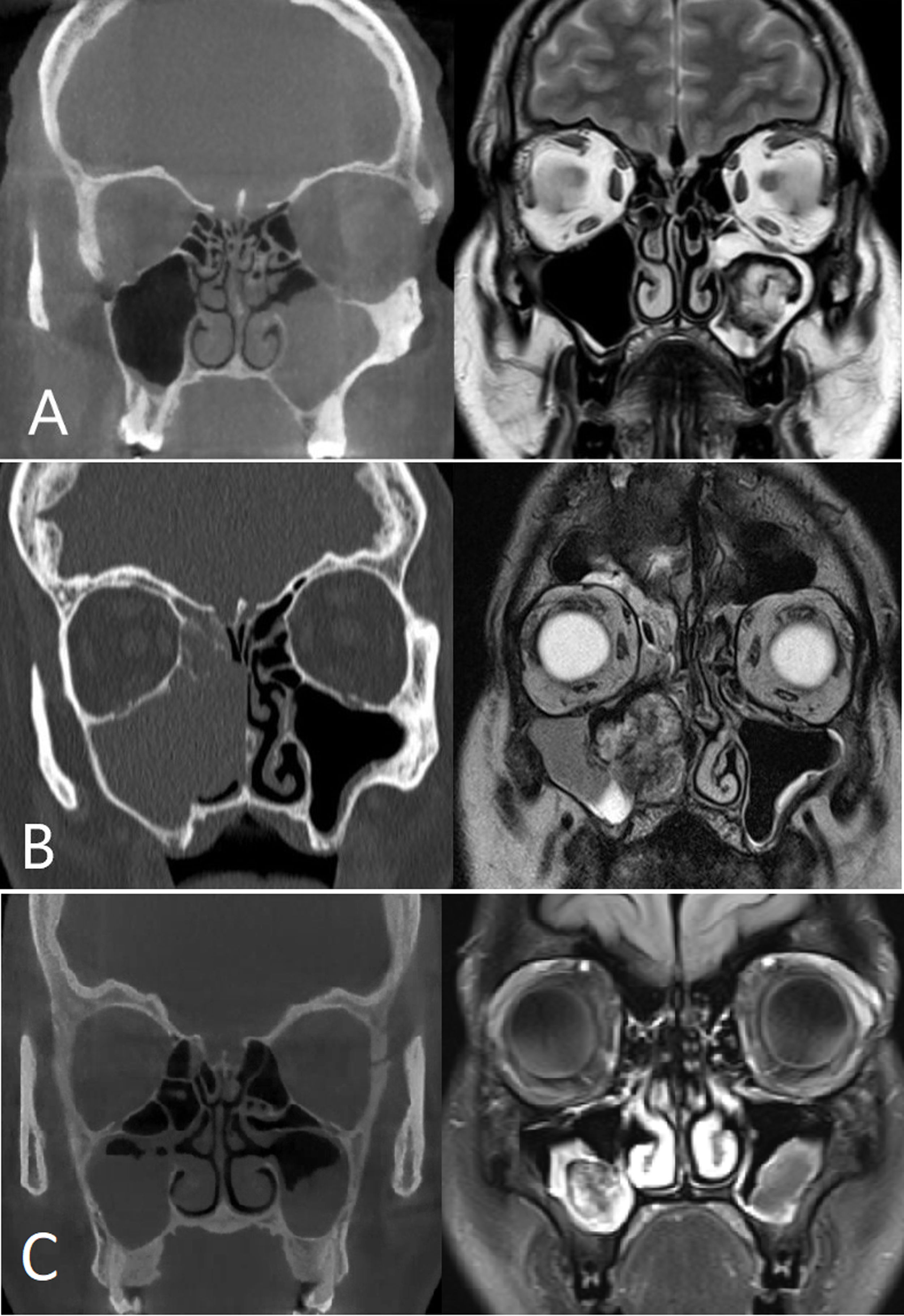
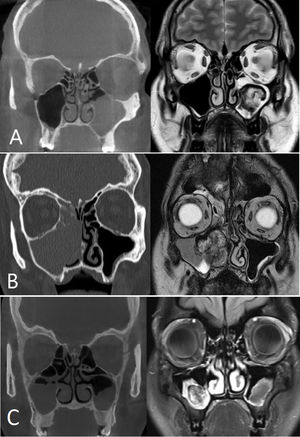
Case reports1st caseA 46-year-old man presented with left nasal obstruction and occasional bloody rhinorrhea for 7 months. He had a history of substituted hypothyroidism. Nasal endoscopy revealed a small polyp in the left middle meatus. Computed tomography (CT) and magnetic resonance imaging (MRI) showed a left maxillary sinus filled with a heterogeneous fleshy lesion (Fig. 1A). Transnasal resection was proposed and revealed an almost avascular soft tissue mass with no attachment within the maxillary sinus and surrounded by an inflammatory mucosa. The postoperative course was uneventful. Histological analysis showed no signs of malignancy but spots of papillary endothelial hyperplasia in an organized hematoma. The patient remained asymptomatic, with no endoscopic sign of recurrence 3 years after the intervention.
(A) Patient 1, coronal CT slice without injection: left maxillary sinus fullness with thickening of surrounding bone. Coronal MRI slice T2-weighted: Heterogeneous tumor in left maxillary sinus with liquid retention. (B) Patient 2, coronal CT slice without injection: right maxillary sinus fullness with intersinusonasal wall demineralization from tumor compression, extending to the surrounding ethmoid cells and nasal fossa. Coronal MRI slice T2-weighted: right maxillary sinus tumor in antra with liquid retention. (C) Patient 3, coronal CT slice without injection: partial maxillary sinuses fullness predominant on the right with intact surrounding bone. Coronal MRI slice T2-weighted: right antral maxillary sinus heterogenous tumor. Thickened mucosa in the left maxillary sinus.
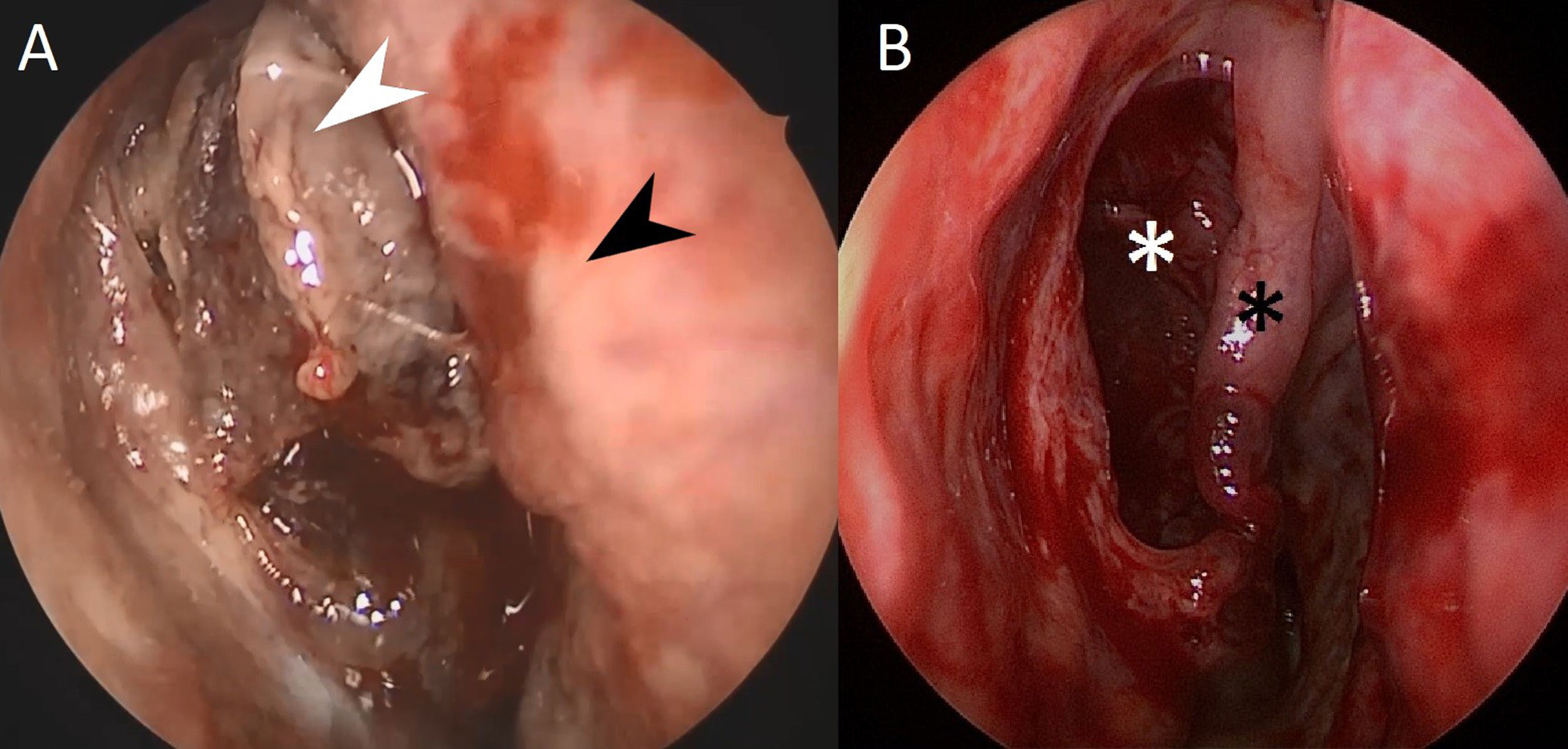
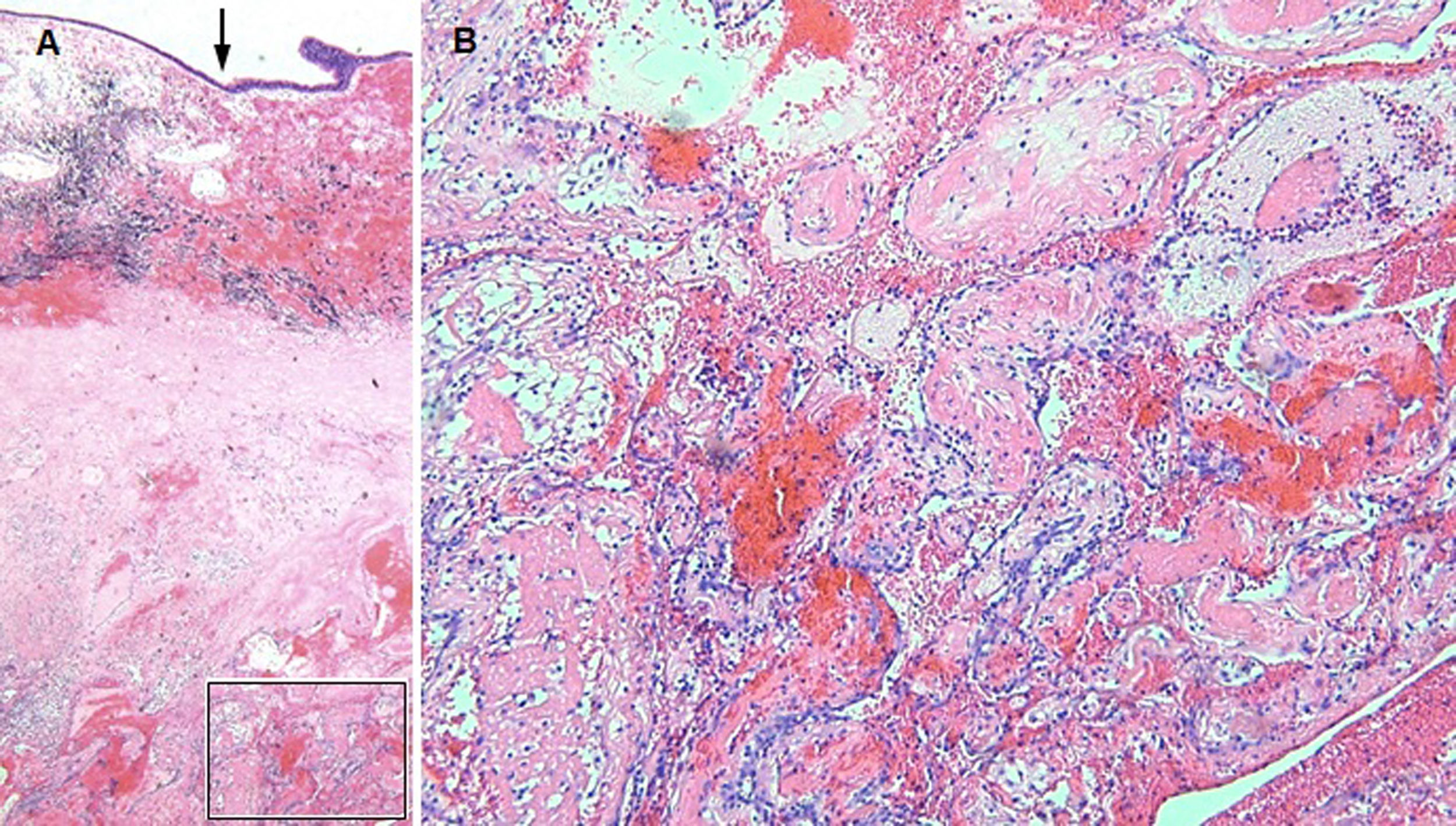
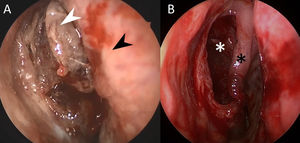
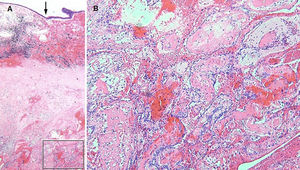
A 76-year-old man consulted several times for repeated right-sided epistaxis associated with posterior rhinorrhea and cough for 5 months. He had a history of ischemic heart disease, high blood pressure, high cholesterol, gout, obesity and active smoking (30 pack-years). Nasal endoscopy revealed a purplish translucent fleshy mass in the right nasal fossa, emerging from middle meatus (Fig. 2A). CT and MRI confirmed the presence of a heterogeneous maxillary tissue mass extending into the nasal fossa, with partial diffusion restriction, associated with fluid retention in the surrounding ethmoid cells (Fig. 1B). Only minimal hemorrhagic material was found on transnasal biopsy and a diagnostic resection was scheduled. The mass was not inserted, attached or adherent to surrounding structures, allowing easy and complete tumorectomy. Adjacent mucosal and bony structures were intact, suggesting a benign process (Fig. 2B). Histological analysis revealed a polypoid alteration of the respiratory mucosa with foci of papillary endothelial hyperplasia in a hematoma in the process of advanced organization, without malignancy (Fig. 3). The postoperative follow-up was uncomplicated, and the patient remained asymptomatic from a rhinological point of view. Nevertheless, due a persistent cough with hemoptysis, a CT of the chest was performed and demonstrated what was later confirmed as a small cell lung carcinoma.
Patient 2 (A), endoscopic view of the right nasal fossa before resection: white arrow: tumor. Black arrow: nasal septum. (B) Same view after total endoscopic resection: one must notice the integrity of the mucosa and bone. White asterisk: posterior wall of right maxillary sinus. Black asterisk: right middle turbinate.
Patient 2 (A), histological analysis showing a respiratory mucosa overhanging an old, organized hemorrhage (framing) with evidence of active resorption (siderophages). The arrow indicates the surface epithelium. (B) Higher magnification showing a non-atypical endothelial proliferation organized in the form of a labyrinthine network and papillary buds. H&E coloring. Original magnification: (A) 20×; (B) 100×.
A 33-year-old woman presented right sided rhinorrhea for several years, associated with occasional ipsilateral increased intraorbital pressure and headache. She had a history of invasive ductal carcinoma with metastasis to lymph nodes and bones, treated with maintenance immunochemotherapy. Clinically, yellowish secretions were present in the right middle meatus. MRI showed a heterogeneous tumor in the right maxillary sinus surrounded by thickened mucosa. CT confirmed subtotal filling of right maxillary sinus with integrity of the surrounding bone (Fig. 1C). In order to clarify a potential sinus metastasis, transnasal endoscopic resection was indicated. It showed the presence of a fleshy dark lesion enveloped in mucus without any infiltration to the surrounding mucosa. Postoperative follow-up was unremarkable. Histology showed multiple fibrohemorrhagic changes compatible with Masson's tumor, without malignancy.
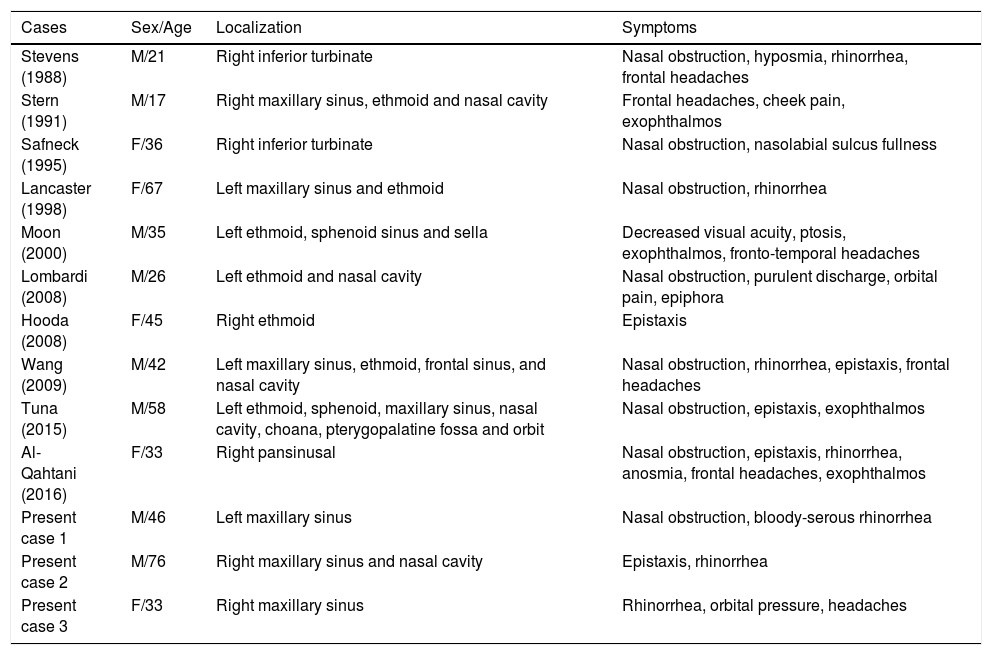
DiscussionMasson's tumor is a rare entity that might be unfamiliar to many specialists. It mimics malignancy from a clinical, endoscopic but especially radiological, point of view. Since its first description in 1923, there have been reported cases affecting almost all parts of the human body, with only very few reports in the sinonasal area. Commonly, symptoms are not specific and related to the affected organ, with the appearance of a lump or a bleeding, rarely associated with pain. The radiological assessment and the biopsies often suggest malignancy. According to one of the largest series reported, this tumor is frequently subcutaneous and dermal with a predilection for the head and neck, digital and trunk regions.2 Cases were also described in the liver, the orbit, intramuscularly, in the oral cavity and intracranially. To the best of our knowledge, only 10 cases, prior to the our reported ones, involved the paranasal sinuses or nasal cavity.3–12 A review of the existing literature on this subject is summarized in Table 1. The men versus women ratio is 1.6:1 and the mean age of presentation is 41±16 years old. The symptoms are those of any sinonasal pathology and do not show specificity.
Summary of published cases of nasal intravascular endothelial papillary hyperplasia.
| Cases | Sex/Age | Localization | Symptoms |
|---|---|---|---|
| Stevens (1988) | M/21 | Right inferior turbinate | Nasal obstruction, hyposmia, rhinorrhea, frontal headaches |
| Stern (1991) | M/17 | Right maxillary sinus, ethmoid and nasal cavity | Frontal headaches, cheek pain, exophthalmos |
| Safneck (1995) | F/36 | Right inferior turbinate | Nasal obstruction, nasolabial sulcus fullness |
| Lancaster (1998) | F/67 | Left maxillary sinus and ethmoid | Nasal obstruction, rhinorrhea |
| Moon (2000) | M/35 | Left ethmoid, sphenoid sinus and sella | Decreased visual acuity, ptosis, exophthalmos, fronto-temporal headaches |
| Lombardi (2008) | M/26 | Left ethmoid and nasal cavity | Nasal obstruction, purulent discharge, orbital pain, epiphora |
| Hooda (2008) | F/45 | Right ethmoid | Epistaxis |
| Wang (2009) | M/42 | Left maxillary sinus, ethmoid, frontal sinus, and nasal cavity | Nasal obstruction, rhinorrhea, epistaxis, frontal headaches |
| Tuna (2015) | M/58 | Left ethmoid, sphenoid, maxillary sinus, nasal cavity, choana, pterygopalatine fossa and orbit | Nasal obstruction, epistaxis, exophthalmos |
| Al-Qahtani (2016) | F/33 | Right pansinusal | Nasal obstruction, epistaxis, rhinorrhea, anosmia, frontal headaches, exophthalmos |
| Present case 1 | M/46 | Left maxillary sinus | Nasal obstruction, bloody-serous rhinorrhea |
| Present case 2 | M/76 | Right maxillary sinus and nasal cavity | Epistaxis, rhinorrhea |
| Present case 3 | F/33 | Right maxillary sinus | Rhinorrhea, orbital pressure, headaches |
Clinico-histological correlation is important when dealing with this lesion. In our experience, the higher the clinical suspicion, the higher the chances to match proper histological diagnosis. It remains speculation, but it could be that Masson's tumor in the paranasal sinuses is perhaps less rare than reported, due to a low clinical suspicion and a lack of communication between the surgeon and the pathologist. A similar phenomenon has been observed recently with hamartomas of the olfactory clefs (REAH),13 where the mention of the entity in the clinical differential diagnosis addressed to the pathologist increases the number of cases found.
The endoscopic aspect during resection must also prompt the surgeon to specifically request the search for intravascular papillary endothelial hyperplasia. In the three cases presented here, the clinical appearance was avascular, without the accompanying expected bleeding. The mass appeared to be poorly vascularized and easy to resect. It was further surprising for the surgeon that the masses lacked a real attachment or insertion point to an intact mucosa, similar to what is observed with removal of a fungus ball.
Radiologically, the three cases presented similarly with a heterogeneous mass suggesting a malignant or at least a solid and tissue process. The differential diagnosis for all three cases were inflammatory polyp, inverted papilloma, lymphoma, adenocarcinoma, squamous cell carcinoma or metastasis. It is difficult on the basis of these three cases to conclude to what extent radiology can suspect this rare specific lesion. On the other hand, it is clear that MRI adds a preoperative value in cases of unilateral opacity discovered on CT. It is also striking to see the similarity on magnetic resonance imaging of all three lesions presented and the cases reported in the literature, to the point where we raise the question if the diagnosis could not already be suspected in the basis of MRI.
Histologically, Masson's tumor must be differentiated from angiosarcoma.14 Histological analysis showed an organized hematoma associated with non-atypical intraluminal endothelial proliferation, characteristic of intravascular papillary endothelial hyperplasia. A correct diagnosis will allow adequate treatment which consists of a complete resection, thus avoiding overtreatment. In our modest series, two patients had a concomitant oncological condition, which raises the question of a simple coincidence or of a potential cofactor promoting the formation of Masson's tumor. The literature, based on small number of cases reported, cannot answer this question.
ConclusionThree new cases of intravascular papillary endothelial hyperplasia of the maxillary sinus are presented. The endoscopical, radiological and pathological characteristics are discussed. These are the 6th, 7th and 8th cases of maxillary sinus involvement reported in the literature. Due to its clinical and radiological presentation, Masson's tumor is often mistaken for a malignant disease and the histology analysis only can confirm the benign diagnosis. The definitive treatment is the complete resection of the lesion.
Conflicts of interestThe authors declare no conflicts of interest.