hematopoietic stem cell transplantation (HSCT) is associated with more respiratory infections due to immunosuppression.
Objectivethis study aimed to verify the frequency of rhinosinusitis after HSCT, and the association between rhinosinusitis and chronic graft vs. host disease (GVHD) and type of transplantation, clinical treatment, surgical treatment, and survival.
Methodsthis was a retrospective study in a tertiary university hospital. A total of 95 patients with hematological diseases undergoing HSCT between 1996 and 2011 were selected.
Resultschronic myeloid leukemia was the most prevalent disease. The type of transplant most often performed was the allogenic type (85.26%). The frequency of rhinosinusitis was 36%, with no difference between the autologous and the allogenic types. Chronic GVHD occurred in 30% of patients. Patients with GVHD had a higher frequency and recurrence of rhinosinusitis, in addition to more frequent need for endoscopic sinusectomy and decreased overall survival.
Conclusionthere was a higher frequency of rhinosinusitis in HSCT and GVHD. The type of transplant does not appear to predispose to the occurrence of rhinosinusitis. GVHD seems to be an aggravating factor and requires a more stringent treatment.
O transplante de células troncas hematopoiéticas (TCTH) associa-se a mais infecções respiratórias devido a imunossupressão.
ObjetivoEste trabalho tem o objetivo de verificar a frequência das rinossinusites pós-TCTH, a associação entre a rinossinusite e a doença do enxerto contra hospedeiro (DECH) crônico e o tipo de transplante e o tratamento clinico e o tratamento cirúrgico e a sobrevida.
MétodoEstudo retrospectivo em hospital universitário terciário. Foram selecionados 95 pacientes com doença hematológica submetidos a TCTH entre 1996 a 2011.
ResultadosA leucemia mieloide crônica foi a doença mais prevalente. O tipo de transplante mais realizado foi o alogênico (85,26%). A frequência de rinossinusite foi de 36%, sem diferença entre os tipos de transplante autólogo e alogênico. A DECH crônica ocorreu em 30% dos pacientes. Os pacientes com DECH tiveram maior frequência e recorrência de rinossinusite, além de mais necessidade de sinusectomia endoscópica e de diminuição da sobrevida global.
ConclusãoHouve maior frequência de rinossinusite no TCTH e DECH. O tipo de transplante não parece predispor a ocorrência da rinossinusite. A DECH parece ser um fator agravante e necessita de tratamento mais rigoroso.
Currently, hematopoietic stem cell transplantation (HSCT) is used in most tertiary hospitals for treatment of hematologic malignant and non-malignant diseases, immunodeficiencies, and solid tumors.1–5 The number of transplantations progressively increases with the improvement and modernization of techniques and drugs used. In Brazil, approximately 12,287 transplantations were performed in the latter half of 2012.6
In spite of advances in the transplantation process, patients are still predisposed to multiple upper airway infections and their complications.1–5,7,8 Immunosuppressive drugs, chemotherapy, radiation therapy, prolonged antibiotic therapy, graft vs. host disease (GVHD), and long periods of hospitalization are predisposing factors for airway infections described in the literature and observed in the everyday life of these patients.1–5,7,8
It is believed that immunosuppression is obviously the main triggering factor of such infections, since the airway is the location most exposed to the environment and its microorganisms. However, studies have demonstrated a higher prevalence and recurrence of rhinosinusitis in transplanted patients with GVHD.5,7,8 There is evidence that alterations in the ultrastructure and on the surface of the respiratory epithelium occur, as well as immunosuppression. Therefore, in addition to the absence of immune protection, there is an alteration on the surface and in the mucociliary clearance, increasing the vulnerability to airway infections in these patients.9,10
Supplementary examinations greatly assist in the diagnosis of rhinosinusitis in transplanted patients, especially nasal endoscopy.4,5,7,8 Computed tomography is used primarily to plan the surgical treatment; however, it does not appear to be useful to predict the occurrence of rhinosinusitis after transplantation.11–14
Isolation of the infectious microorganism through cultures or by direct screening is important to determine the drug therapy and even the surgical treatment, due to the existence of more diversified and resistant microorganisms, including fungi.4,5,7
The treatment of rhinosinusitis in transplanted patients must be established more promptly and should involve the use of broad-spectrum antibiotics for a long period.2–5,7,8,10 More predisposed patients, such as those with GVHD, are candidates to endoscopic sinusectomy in recurrent rhinosinusitis.4,5,7,15
This study aimed to analyze, firstly, the profile of patients treated in this department by assessing the frequency of rhinosinusitis after HSCT, and secondly, the association between rhinosinusitis, GVHD, the type of transplantation, as well as the clinical and surgical treatment of such rhinosinusitis.
Materials and methodsThis was a retrospective study performed in a tertiary university hospital. A total of 95 patients with hematologic diseases submitted to HSCT were selected. They were treated at the Otorhinolaryngology-Head and Neck Surgery Outpatient Clinic from 1996 to 2011. Inclusion criteria were all types of HSTC, adult patients, and any otorhinolaryngology complaint. Pediatric patients and those who were not submitted to a transplant were excluded.
The variables studied were hematological disease, type of transplantation, rhinosinusitis occurrence and GVHD, alterations in the computed tomography (CT) scan of the paranasal sinuses and nasal endoscopy, type of clinical treatment, need for sinonasal surgery, and overall survival time. These data were collected from medical records and examinations performed at the service. Records that contained incomplete data for the statistical analysis were excluded. Missing data were removed from the calculation during the statistical analysis of each variable. Therefore, the total of some variables was less than the total sample number (95).
The diagnosis of rhinosinusitis was established according to the symptoms and signs on physical examination, in addition to nasal endoscopy results, according to the Guidelines on Rhinosinusitis of ABORL-CCF and EPOS.10
The Research Ethics Committee of UNICAMP approved the study, and an informed consent was obtained from all patients (088/2001).
Comparisons were performed between the variables, type of transplantation, and GVHD with rhinosinusitis occurrence, treatment, and survival. These variables were statistically analyzed through frequency distribution, Fisher's exact test, Kaplan–Meier curves, and Cox models.
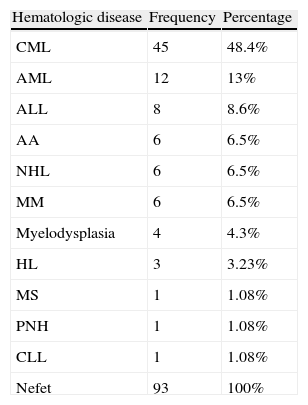
ResultsRegarding hematological disease, chronic myeloid leukemia was the most prevalent disease, followed by acute myeloid leukemia and acute lymphocytic leukemia. Table 1 shows the distribution of hematologic malignancies in the 95 patients.
Frequency of hematologic diseases of the selected patients.
| Hematologic disease | Frequency | Percentage |
| CML | 45 | 48.4% |
| AML | 12 | 13% |
| ALL | 8 | 8.6% |
| AA | 6 | 6.5% |
| NHL | 6 | 6.5% |
| MM | 6 | 6.5% |
| Myelodysplasia | 4 | 4.3% |
| HL | 3 | 3.23% |
| MS | 1 | 1.08% |
| PNH | 1 | 1.08% |
| CLL | 1 | 1.08% |
| Nefet | 93 | 100% |
CML, chronic myeloid leukemia; AML, acute myeloid leukemia; ALL, acute lymphoblastic leukemia; AA, aplastic anemia; NHL, non-Hodgkin's lymphoma; MM, multiple myeloma; HL, Hodgkin's lymphoma; MS, multiple sclerosis; PNH, paroxysmal nocturnal hemoglobinuria; CLL, chronic lymphocytic leukemia; Nefet, N effective.
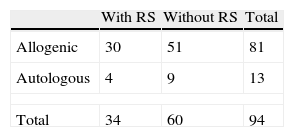
The type of transplantation most often performed was the allogenic type (85.26%). Acute rhinosinusitis occurred in 34 patients, which corresponds to a rate of 36.17%. There was no significant difference in the occurrence of rhinosinusitis in different autologous (30%) or allogenic (37%) transplantations. The type of HSCT was not associated with a higher incidence of sinusitis (Table 2).
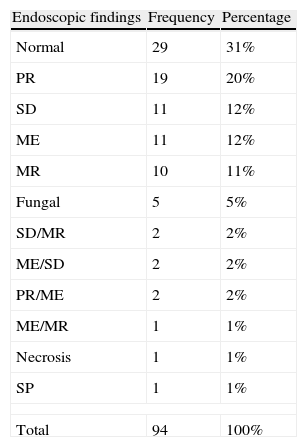
Nasal endoscopy was performed in 98.95% of patients. This examination showed results within the normal range in 29% of cases. The most frequent alteration (20%) found was purulent rhinorrhea (Table 3). Alterations suggestive of fungal infection were observed in little more than 5% of patients, such as brownish or grayish mucosa of the anterior nasal septum and middle and lower turbinates, in addition to necrosis of the nasal fossa structures, mainly of the middle turbinate in 1% of patients.
Nasal endoscopy alterations.
| Endoscopic findings | Frequency | Percentage |
| Normal | 29 | 31% |
| PR | 19 | 20% |
| SD | 11 | 12% |
| ME | 11 | 12% |
| MR | 10 | 11% |
| Fungal | 5 | 5% |
| SD/MR | 2 | 2% |
| ME/SD | 2 | 2% |
| PR/ME | 2 | 2% |
| ME/MR | 1 | 1% |
| Necrosis | 1 | 1% |
| SP | 1 | 1% |
| Total | 94 | 100% |
PR, purulent rhinorrhea; SD, septal deviation; ME, mucosal edema; MR, mucoid rhinorrhea; SP, septal perforation; Necrosis, signs of necrosis of the mucosa and signs of fungal infection with whitish, gray, or black staining (fungal).
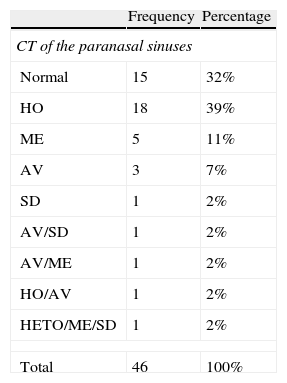
The CT scan of the paranasal sinuses was performed in 48.42% of patients. The homogeneous opacification of the paranasal sinus without bone structural alterations, regardless of the affected sinus, was the most frequent alteration (approximately 40%), followed by mucosal edema in 10% of the CTs (Table 4).
Computed tomography (CT) of the paranasal sinuses findings.
| Frequency | Percentage | |
| CT of the paranasal sinuses | ||
| Normal | 15 | 32% |
| HO | 18 | 39% |
| ME | 5 | 11% |
| AV | 3 | 7% |
| SD | 1 | 2% |
| AV/SD | 1 | 2% |
| AV/ME | 1 | 2% |
| HO/AV | 1 | 2% |
| HETO/ME/SD | 1 | 2% |
| Total | 46 | 100% |
HO, homogeneous opacification; ME, mucosal edema; AV, anatomic variation; SD, septal deviation; HETO, heterogeneous opacification.
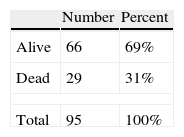
Approximately 70% of the patients were alive at the time of the study (Table 5). The mean time of HSCT was 8.9 years (4 months–16 years).
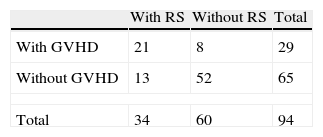
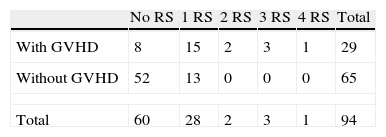
The development of GVHD after transplantation occurred in 30.53% of patients. The occurrence of GVHD was not associated with higher mortality (p=0.228). However, the frequency (72%) and the number of rhinosinusites were significantly higher in patients with GVHD (Table 6). Approximately 28% of patients with GVHD had more than two episodes of rhinosinusitis, whereas no patients without GVHD had rhinosinusitis recurrence (Table 7).
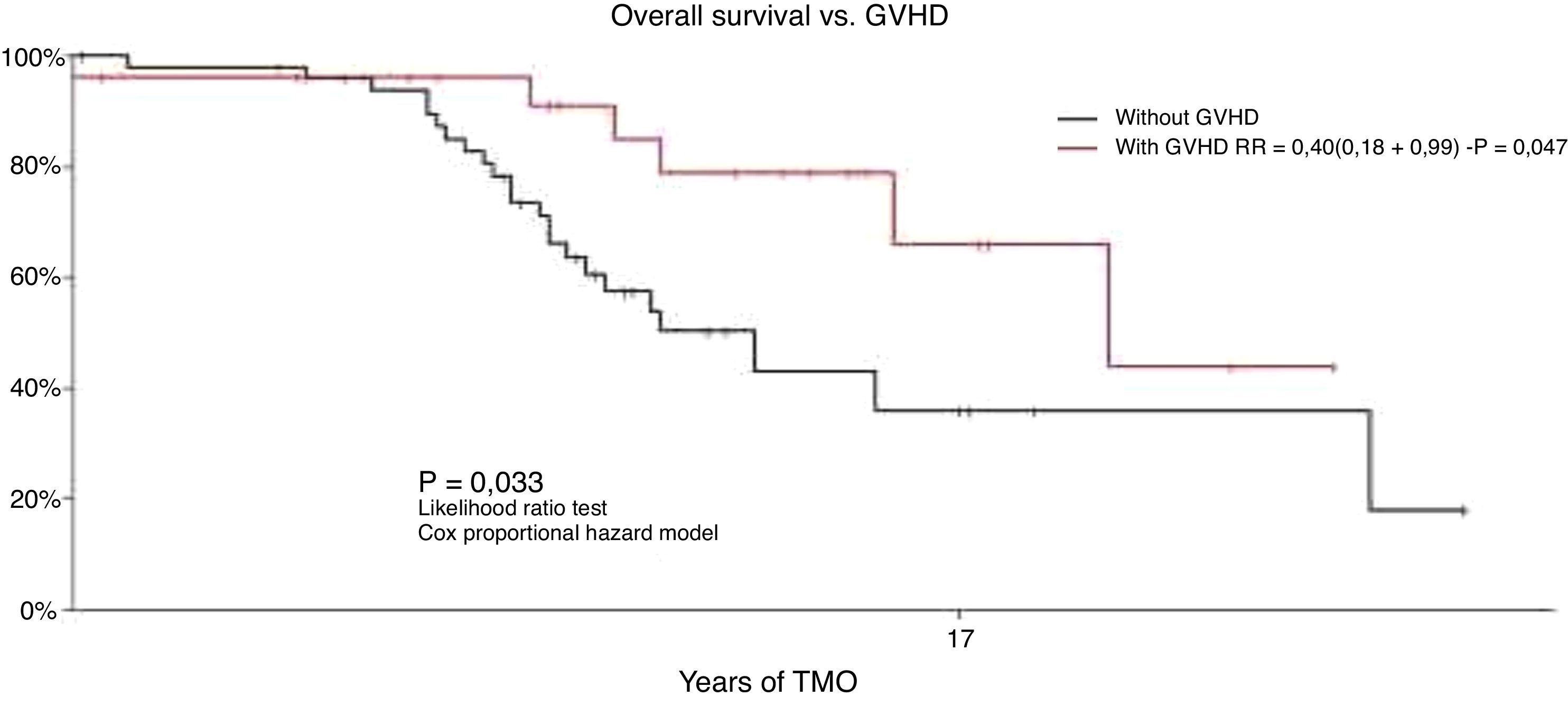
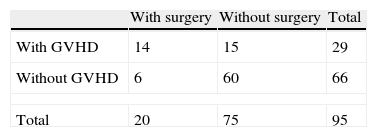
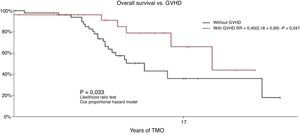
The patients who had GVHD had greater need for surgical treatment (p<0.001) and decreased overall survival (Table 8 and Fig. 1). The surgical treatment performed was endoscopic sinusectomy under general anesthesia.
Endoscopic sinusectomy was performed in 58% (20/34) of patients with rhinosinusitis, and approximately 48% of these patients had GVHD; only 9% did not have GVHD.
DiscussionThe increased number of immunosuppressed patients as a result of advancements in medicine in the treatment of malignant neoplasms, and degenerative and autoimmune diseases has simultaneously provided greater experience in the management of these cases.
Patients undergoing transplantations suffer several preparatory organic modifications and remain immunosuppressed during this process for a variable period of time.1–5,7 The allogenic HSCT may or may not be myeloablative, which causes increased immunosuppression in patients.1 In this study, there was a higher number of allogenic transplantations; however, the percentage of myeloablative procedures was not obtained.
The frequency of rhinosinusitis coincided with the post-HSCT estimate described in the literature (36.7%), but was slightly lower than that in the previous study (42%) performed in this same service.2,3,5,8 This can be explained by the greater care given to these patients before transplantation, or lower myeloablation during the current HSCT process. As no data were obtained regarding myeloablation, the latter association cannot be explained. However, the frequency of rhinosinusitis remains higher when compared to immunocompetent patients (5–15%).10
Anterior rhinoscopy is inadequate for the appropriate sinonasal assessment of these transplanted patients. Nasal endoscopy is the ideal and essential examination to attain a correct and early diagnosis of rhinosinusitis, both pre- and post-HSCT. Endoscopic assessment can evaluate the characteristics of secretion and the mucosa. Thus, it better suggests the etiologic factor (bacterial, viral, or fungal) and allows for early treatment of sinonasal disease. It is noteworthy that the sign of necrosis or brownish or grayish mucosa, mainly in the middle turbinate and anterior nasal septum, suggests invasive fungal infection.4,5,7,10,15
Computed tomography (CT) of the paranasal sinuses is a specific examination, in spite of its low sensitivity, as it does not differentiate the type of secretion (purulent or mucoid). It also does not show specific signs of invasive fungal sinusitis in the initial stage of the disease. However, in immunosuppressed patients, CT assists in the management of unfavorable cases and is crucial in the assessment of rhinosinusitis complications.11–14
The literature shows controversial opinions regarding the performance of CT pre-HSCT. Billings showed that CT of the paranasal sinuses before transplantation may be useful for the prevention of rhinosinusitis post-HSCT in children.14 However, Arulrajah argued that the symptoms of rhinorrhea, cough, and nasal congestion have similar importance to the CT results, with no need for CT when these symptoms exist.12 Kasow suggested the performance of preventive CT of the paranasal sinuses before HSCT in children due to the alterations found in the examinations, although these were not directly related to the child's symptoms.13
Ortiz showed that CT pre-HSCT in adults does not predict post-HSCT sinusitis; and anatomical variations do not predispose to rhinosinusitis after HSCT, but contribute to post-HSCT rhinosinusitis severity.11 Therefore, performing CT of the paranasal sinuses prior to HSCT is suggested only when the patient has chronic sinonasal symptoms or acute rhinosinusitis with unfavorable evolution. After the HSCT, this examination would be effective in cases refractory to medical treatment or suspected cases of complications, either fungal or bacterial, in order to highlight specific causes blocking ostial drainage, anatomical variations, or invasion of adjacent structures.
The frequency of GVHD found in the study (30%) was lower than that reported in the literature (50%).5,8 These patients were more susceptible to the development and recurrence of rhinosinusitis, which is in agreement with the literature.2–5,8,9
A previous study showed that in addition to immunosuppression, there is a change in the ultrastructure of the respiratory ciliated pseudo-stratified epithelium and microscopic changes on the epithelial surface, such as squamous metaplasia and fibrosis. Therefore, there must be a change in mucociliary clearance that would predispose to recurrence of the rhinosinusitis.9 Thus, these patients with GVHD have a greater need of surgical treatment for recurrent rhinosinusitis control.8,9
ConclusionPatients who received HSCT have a higher incidence of sinusitis when compared to immunocompetent patients.
The type of transplantation does not influence the frequency of rhinosinusitis; however, chronic GVHD appears to actually be an aggravating factor.
Chronic GVHD was associated with a greater need for sinus surgery to control rhinosinusitis. Additionally, these patients with chronic GVHD showed decreased overall survival.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Bento LR, Ortiz E, Nicola EM, Vigorito AC, Sakano E. Sinonasal disorders in hematopoietic stem cell transplantation. Braz J Otorhinolaryngol. 2014;80:285–9.
Institution: Discipline of Otorhinolaryngology, Head and Neck Unit, Rhinology Sector of Hospital das Clínicas – UNICAMP, Campinas, SP, Brazil.