In children, hypoacusis, or conductive hearing loss, is usually acquired; otitis media with effusion is the most common etiology. However, in some cases this condition is congenital, ranging from deformities of the external and middle ear to isolated ossicular chain malformations. The non-ossicular anomalies of the middle ear, for instance, persistent stapedial artery and anomaly of the facial nerve, are uncommon but may accompany the ossicular defects.
ObjectiveThis study aimed to describe the clinical presentation, diagnostic tests, and therapeutic options of congenital malformations of the middle ear.
MethodsThis was a retrospective study of cases followed in otolaryngologic consultations since 2007 with the diagnosis of congenital malformation of the middle ear according to the Teunissen and Cremers classification. A review of the literature regarding the congenital malformation of the middle ear and its treatment is presented.
ConclusionMiddle ear malformations are rarely responsible for conductive hearing loss in children. As a result, there is often a late diagnosis and treatment of these anomalies, which can lead to delays in the development of language and learning.
Na criança, a hipoacusia de condução é geralmente adquirida, sendo a otite média com efusão a etiologia mais comum. No entanto, em alguns casos é congênita, decorrente desde de deformidades das orelhas média e externa até malformações isoladas da cadeia ossicular. As anomalias não ossiculares da orelha média, como a persistência da artéria estapédica e a alteração do percurso do nervo facial, são incomuns, podendo acompanhar as malformações ossiculares.
ObjetivoEste estudo tem como objetivo descrever a apresentação clínica, os meios auxiliares de diagnóstico e opções terapêuticas das malformações congênitas da orelha média.
MétodosOs autores apresentam um estudo retrospectivo de casos de malformação congênita da orelha média diagnosticados de acordo com a classificação de Teunissen e Cremers, acompanhados em consultas otorrinolaringológicas desde 2007. É também apresentada uma revisão da literatura sobre malformações congênitas da orelha média e seu tratamento.
ConclusãoAs malformações da orelha média são raramente responsáveis pela hipoacusia de condução nas crianças. A demora no diagnóstico e tratamento pode levar a atrasos na linguagem e na aprendizagem.
In children, conductive hearing loss is usually acquired, and otitis media with effusion is the most common etiology. However, in some cases are congenital, ranging from deformities of the external and middle ears to isolated malformations of the ossicular chain. These latter conditions are very rare, often leading to late diagnosis, especially when they are unilateral.1 Ossicular malformations may be accompanied by non-ossicular middle ear deformities, such as the persistence of the stapedial artery, an anomaly of facial nerve path, high jugular bulb, and an aberrant internal carotid artery.2,3
Congenital anomalies of the middle ear can be classified into major, when associated with an involvement of the tympanic membrane and external ear, or minor, when there is an exclusive involvement of the middle ear.4
The effects of malformations of the middle ear can range from the altered configuration and size of the tympanic cavity to variation in the number, size, and configuration of ossicles. Anomalies of the round window and, more rarely, of the oval window may still occur. The most common isolated ossicular deformity involves the stapes superstructure and the long apophysis of the incus.5
In 1993, Teunissen and Cremers created a classification of minor malformations, based on the surgical approach, dividing them into four main groups: isolated stapes ankylosis, stapes ankylosis associated with other ossicular malformations, deformity of the ossicular chain with mobile stapes footplate, and severe aplasia or dysplasia of oval or round windows (Table 1).4
Classification of minor congenital malformations according to Teunissen and Cremers.
| Class | Malformations | % |
|---|---|---|
| 1 | Ankylosis or isolated congenital fixation of the stapes | 30.6% |
| • Footplate fixation | ||
| • Superstructure fixation | ||
| 2 | Stapes ankylosis associated with other malformations of the ossicular chain | 38.1% |
| • Deformities of the incus and/or malleus, or aplasia of the long apophysis of the incus | ||
| • Bone fixation of malleus and/or incus | ||
| 3 | Congenital anomalies of the ossicular chain with mobile stapes footplate | 21.6% |
| • Disruption of the ossicular chain | ||
| • Epitympanic fixation | ||
| • Tympanic fixation | ||
| 4 | Congenital aplasia or severe dysplasia of the oval and round windows | 9.7% |
| • Aplasia | ||
| • Dysplasia | ||
| • Prolapse of facial nerve | ||
| • Persistence of stapedial artery |
Most of these cases occur sporadically; one-quarter of the cases occur in the context of a genetic syndrome, including branchiootorenal (BOR) syndrome, Crouzon syndrome, Klippel-Feil syndrome, or Pfeiffer syndrome.6 In non-syndromic children, the clinical history plays a crucial role, and the most common presentation is a child with diminished hearing acuity, speech delay, and poor school performance with a normal otoscopy. Many children have a history of prior insertion of transtympanic ventilation tubes, in cases of suspected otitis media with effusion.7
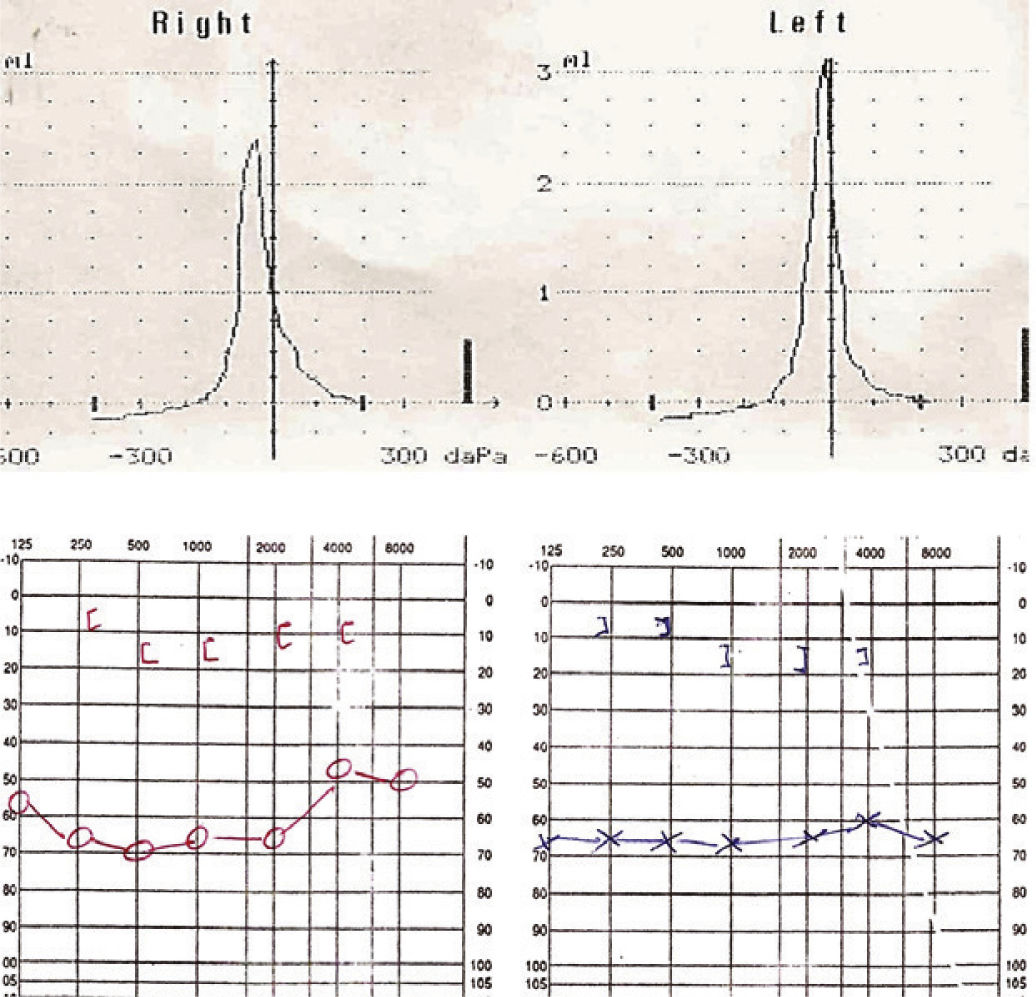
The impedancimetry and audiometry are critical, demonstrating a normal pressure in the middle ear (tympanogram type A), with a possible reduction in compliance due to the fixation of the ossicular chain, and an average hearing threshold of 50dB HL with an air-bone gap of about 35dB HL.
High-resolution computed tomography (CT) imaging is the method of choice, since it allows for a correct visualization of bony structures. However, exploratory tympanotomy is the method that most reliably establishes the definitive diagnosis.8,9
The appropriate treatment consists of hearing aids or surgical intervention. In case of surgical treatment for unilateral ear involvement, this should ideally be delayed until 10 years of age, adolescence, or even adulthood, so that the patient can have an active role in treatment decisions.10
In cases of bilateral hearing loss, the treatment is imperative, and the use of a conventional prosthesis or bone-anchored hearing aid (BAHA) are good options for the child who is not a candidate for reconstructive surgery. Conversely, in unilateral hearing loss, there is no consensus in the literature regarding the best option; in this case, it is necessary to weigh the possible advantages (masking tinnitus and a better hearing performance in a noisy environment) versus the disadvantages (otitis externa, altered body image) of the hearing aids.6,11
Based on these concepts, the authors present illustrative clinical cases of the disease in question.
MethodsThis was a retrospective longitudinal cohort study between January of 2007 and July of 2013 that included all patients with a diagnosis of congenital malformation of the middle ear, followed in the Otorhinolaryngology Department. Five patients were included after the processes, audiometric records, and computed tomographies (CTs) of ears were reviewed. The malformations were classified according to the Teunissen and Cremers classification. Patients with concomitant external ear malformations were excluded.
A review of the literature through the PubMed database was performed, assessing congenital malformations of the middle ear and its treatment.
Description of casesFive cases of patients with clinical diagnosis of malformation of the middle ear are presented. All children underwent audiogram, tympanogram, and high resolution CT.
Case 1Male child, 6 years old, white, healthy, referred to an otolaryngologic consultation after multiple myringotomies with bilateral transtympanic ventilation tube insertion, without hearing improvement, and no history of recurrent acute otitis media (AOM) nor family history of deafness.
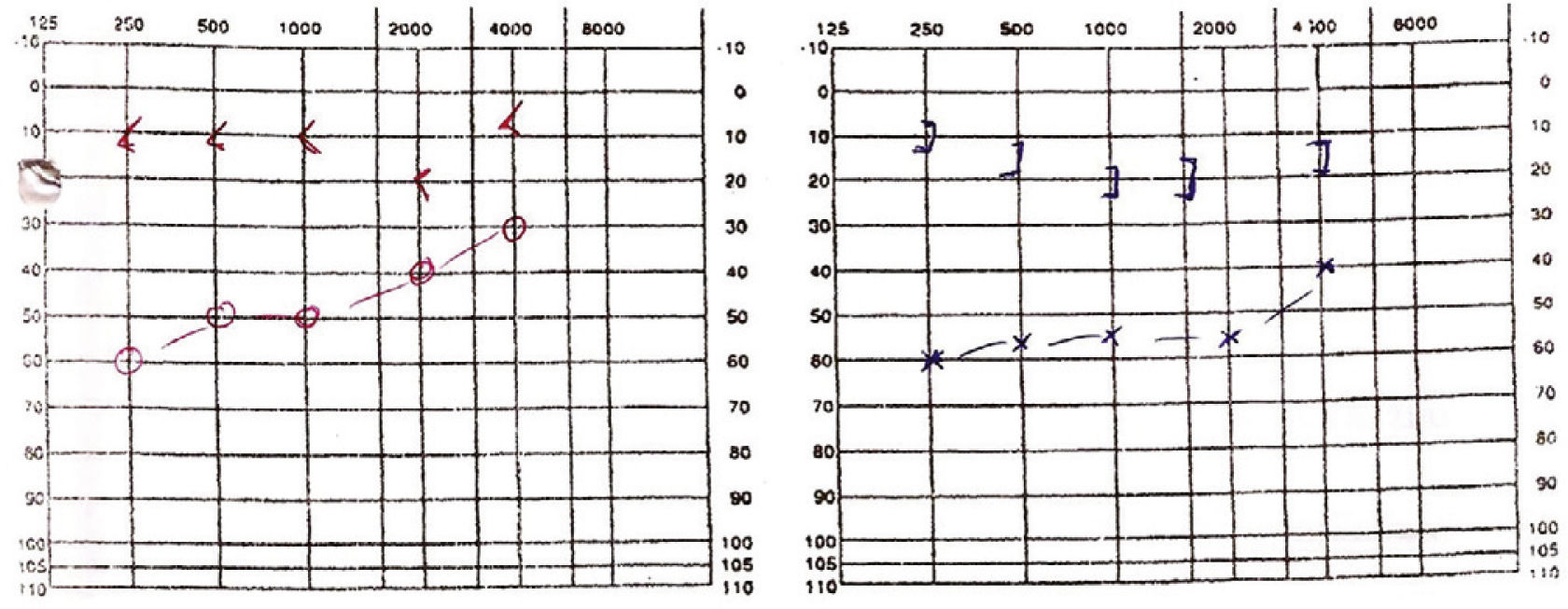
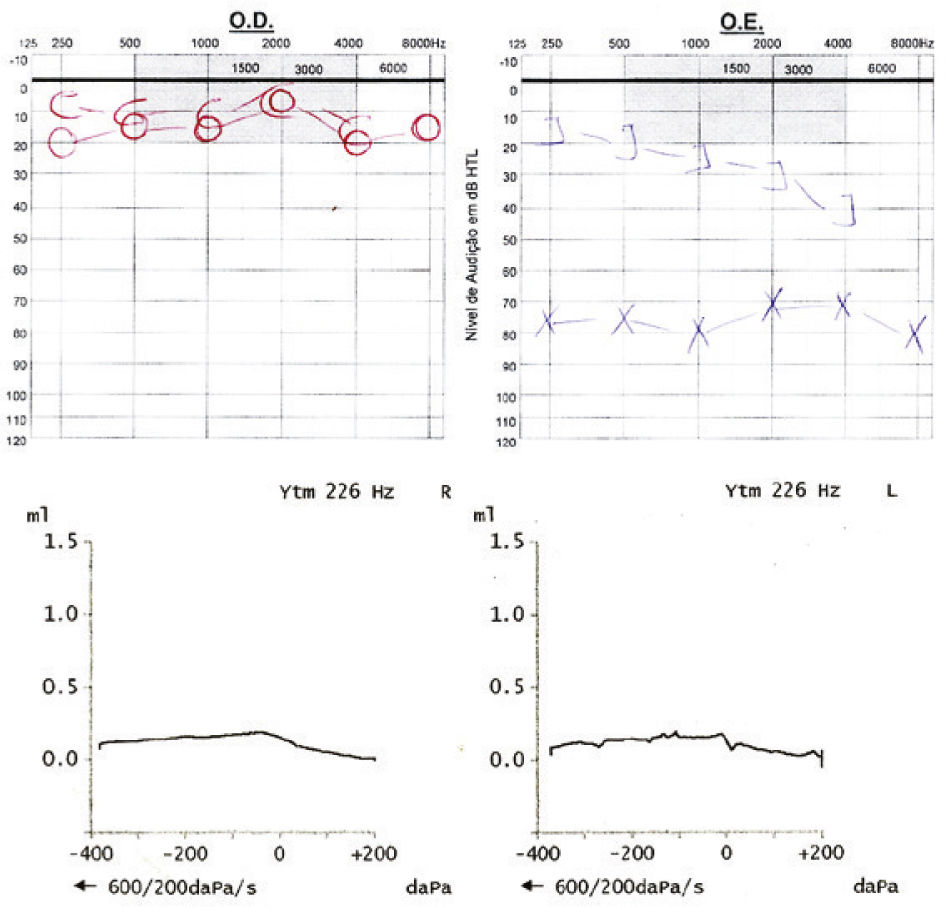
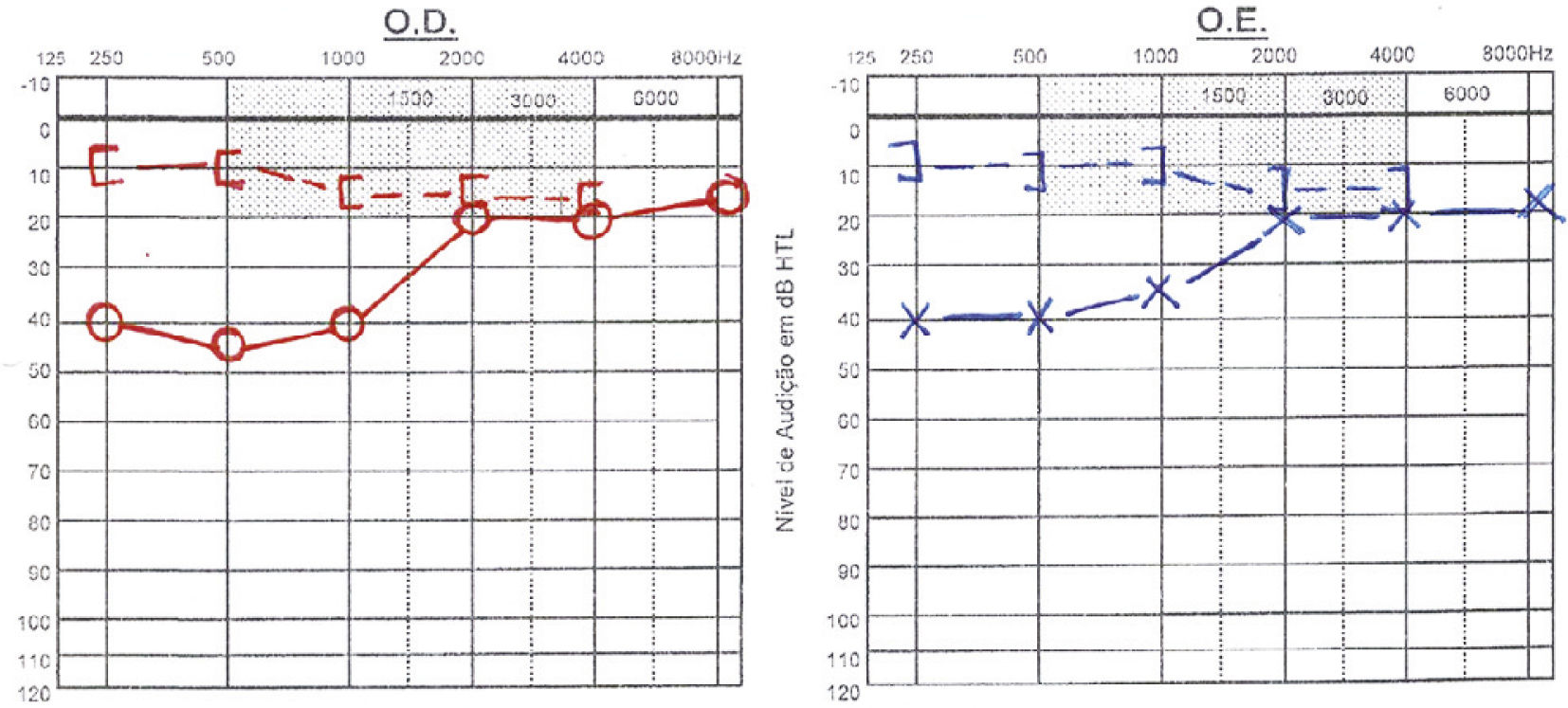
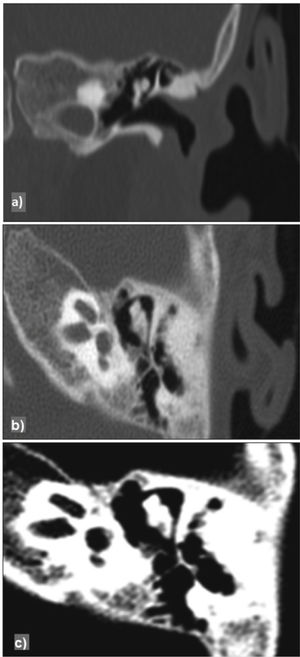
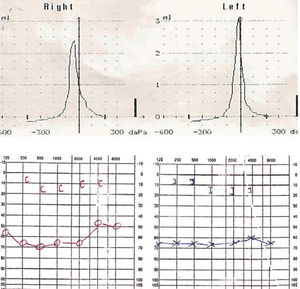
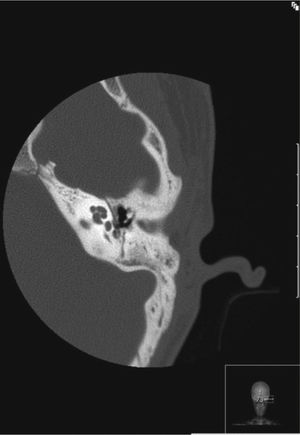
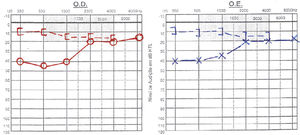
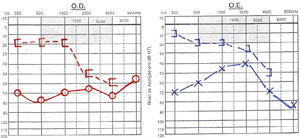
At physical examination, the external auditory canals and tympanic membranes were normal. The audiometry revealed moderate conduction hearing loss (Fig. 1).
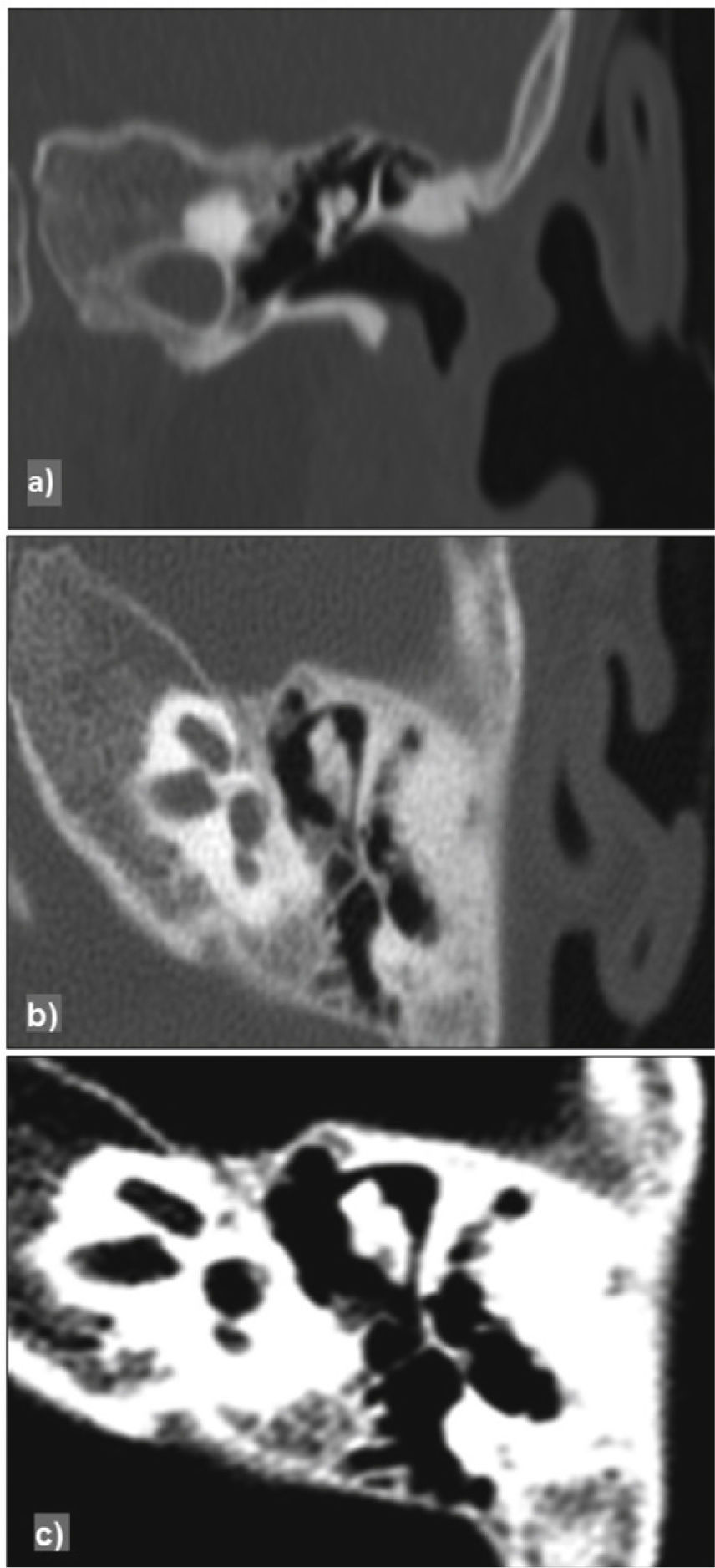
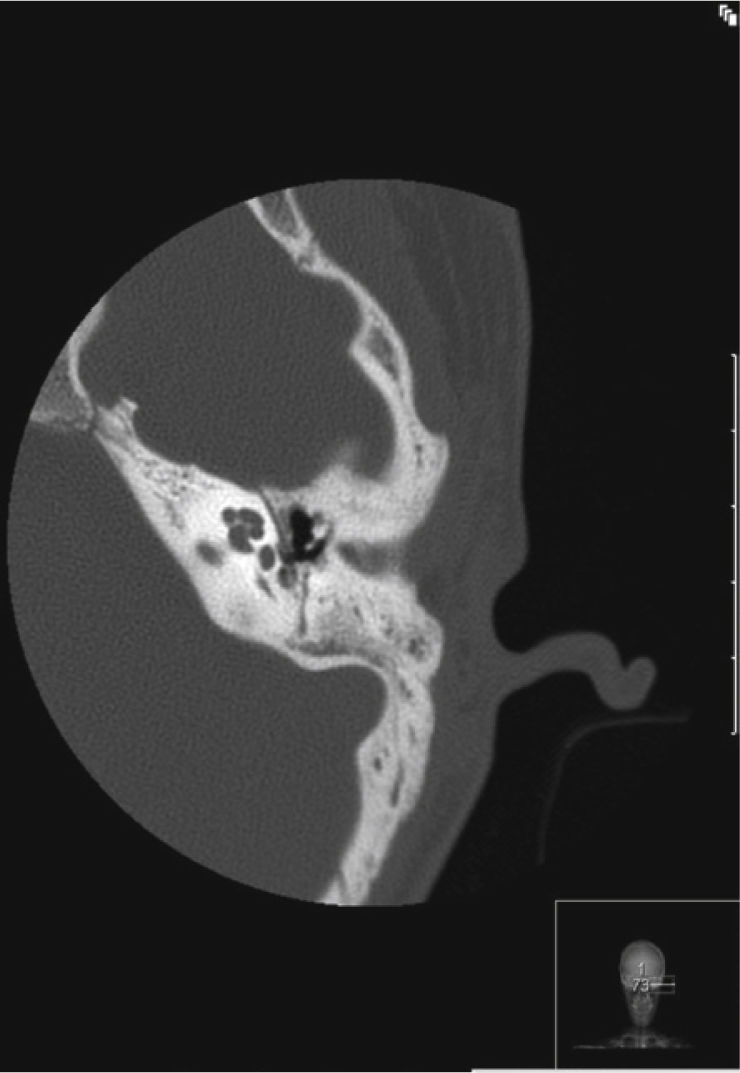
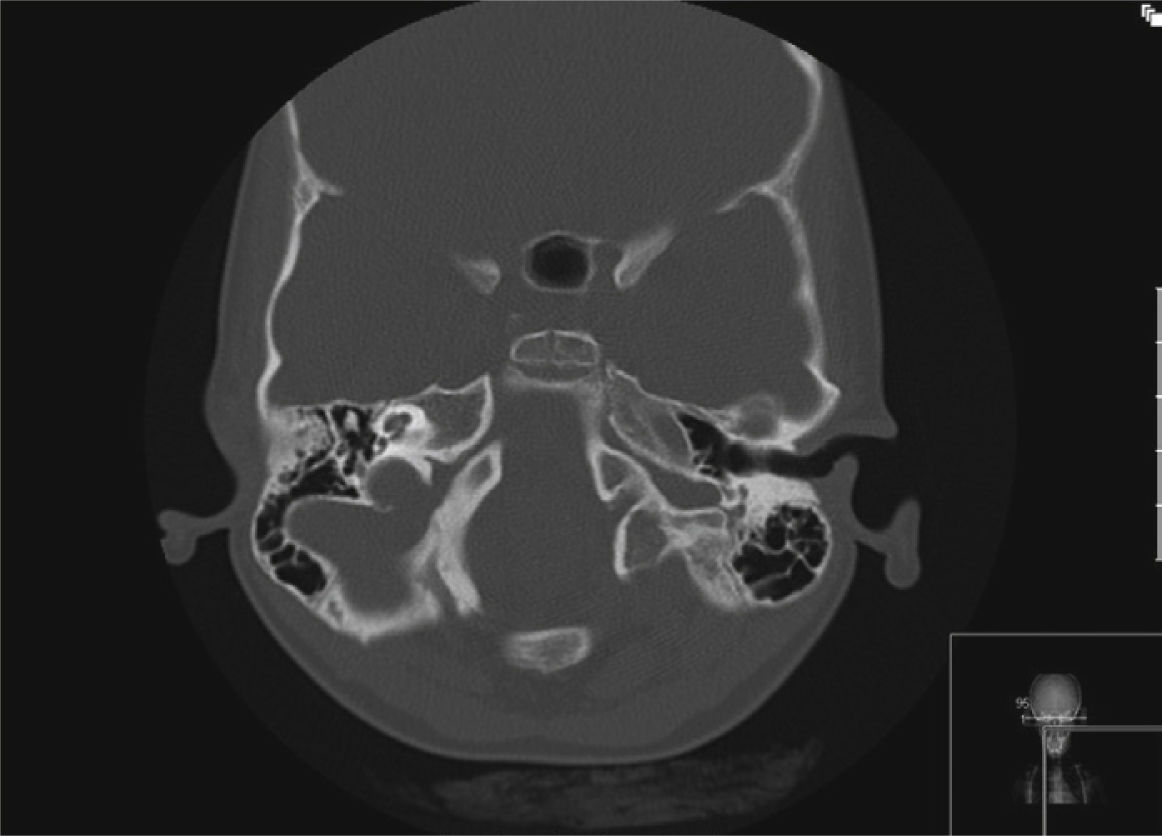
High resolution CT was performed, which revealed absence of stapes and oval window. The malleus and incus were present, but the long apophysis of the incus was in a posterior direction, and the handle of malleus was fixed in the anterior and superior walls of the epitympanum (Fig. 2). Similar alterations in the contralateral ear were observed.
The patient underwent hearing rehabilitation with conventional hearing aids, with poor adjustment. As such, the patient underwent implantation of bilateral BAHA, without surgical complications and with a subsequent hearing gain.
Case 2Female child, age 6, white, with known history of multiple malformations, including tracheal stenosis, cervical aortic arch, and atrial septal defect, and no history of AOM nor deafness in the family. She was referred to an ENT consultation for a screening for deafness in the context of a severe language delay.
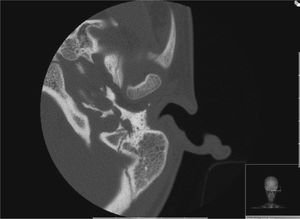
The objective examination of the external ear and the otoscopy showed no alterations. The tympanogram showed normal pressure in the middle ear (type Ad). Audiometry demonstrated a moderate bilateral conduction deafness (Fig. 3).
High-resolution CT was performed, which demonstrated absence of stapes and oval window, and an anomaly in the course of the facial nerve (Fig. 4).
The patient underwent hearing rehabilitation with conventional bilateral hearing aids, with auditory gain.
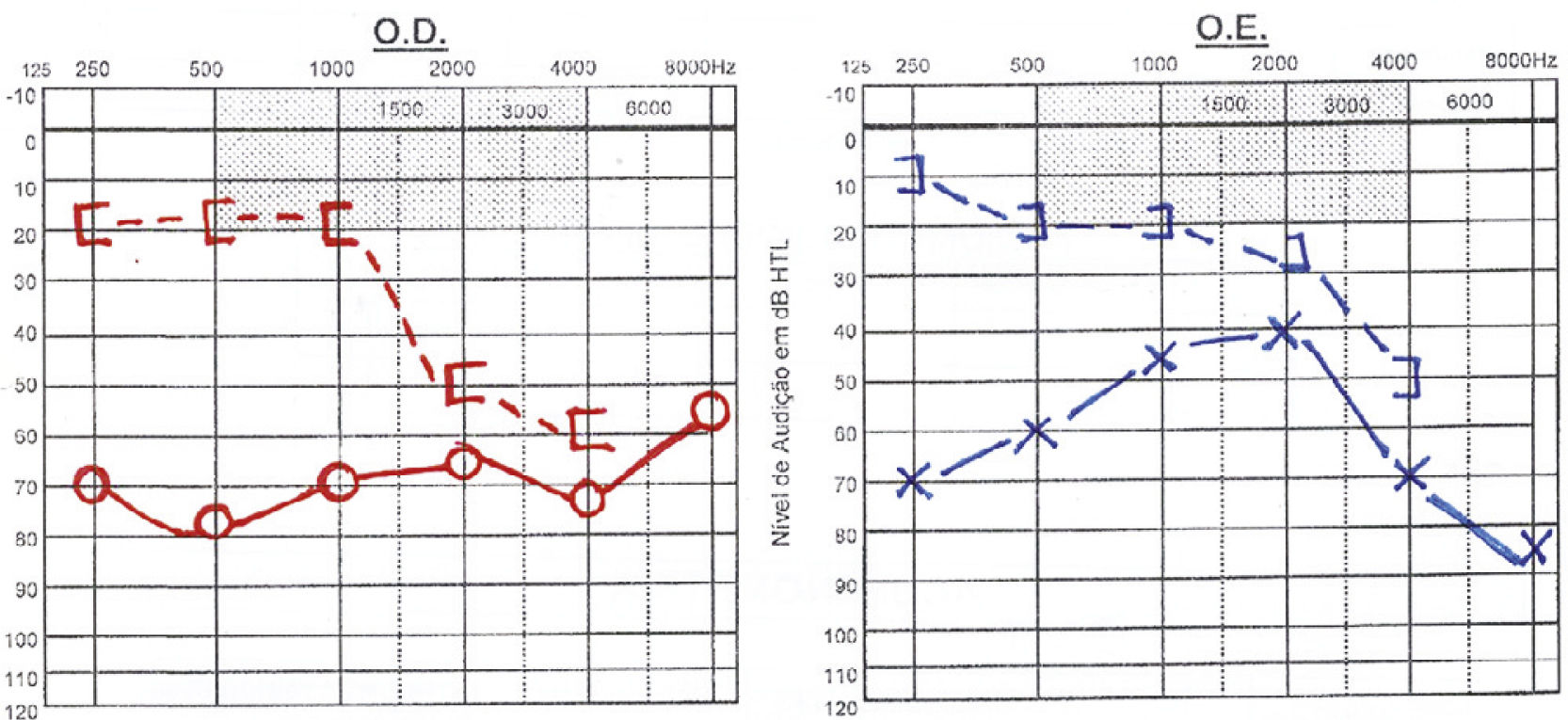
Case 3Male child, age 9, white, without a significant history, referred for an ENT consultation due to hearing loss. He did not have repetition of AOM nor family history of deafness. On physical examination, the outer ear presented no alterations. The audiogram revealed severe conduction hearing loss on the left, with normal hearing on the right and bilateral type B tympanogram (Fig. 5).
The patient underwent double bilateral myringotomy with transtympanic ventilation tube insertion, without hearing improvement.
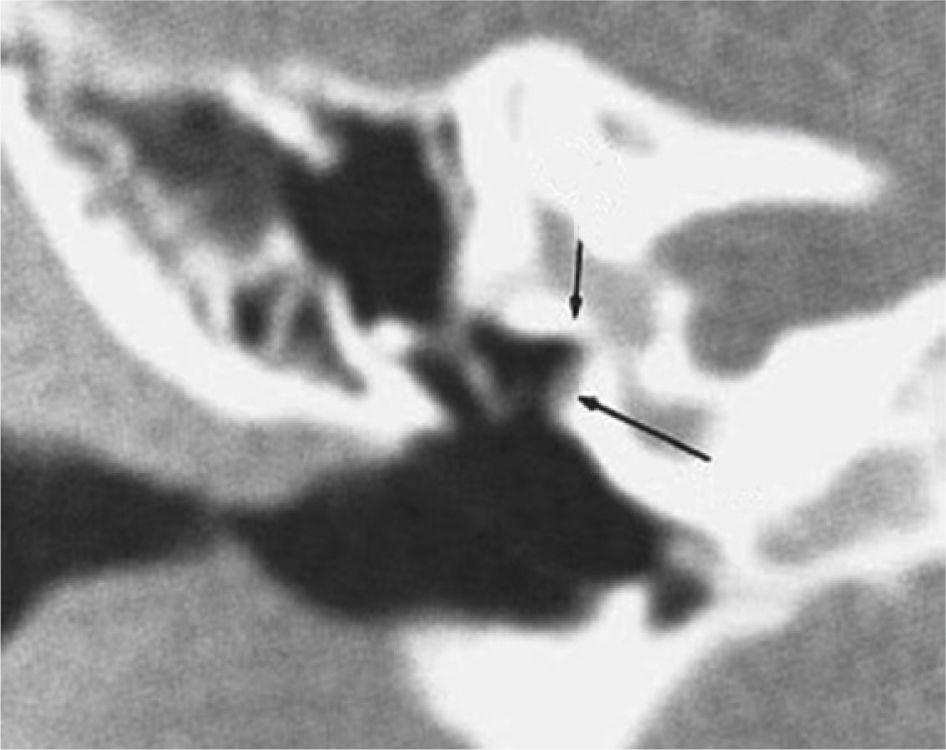
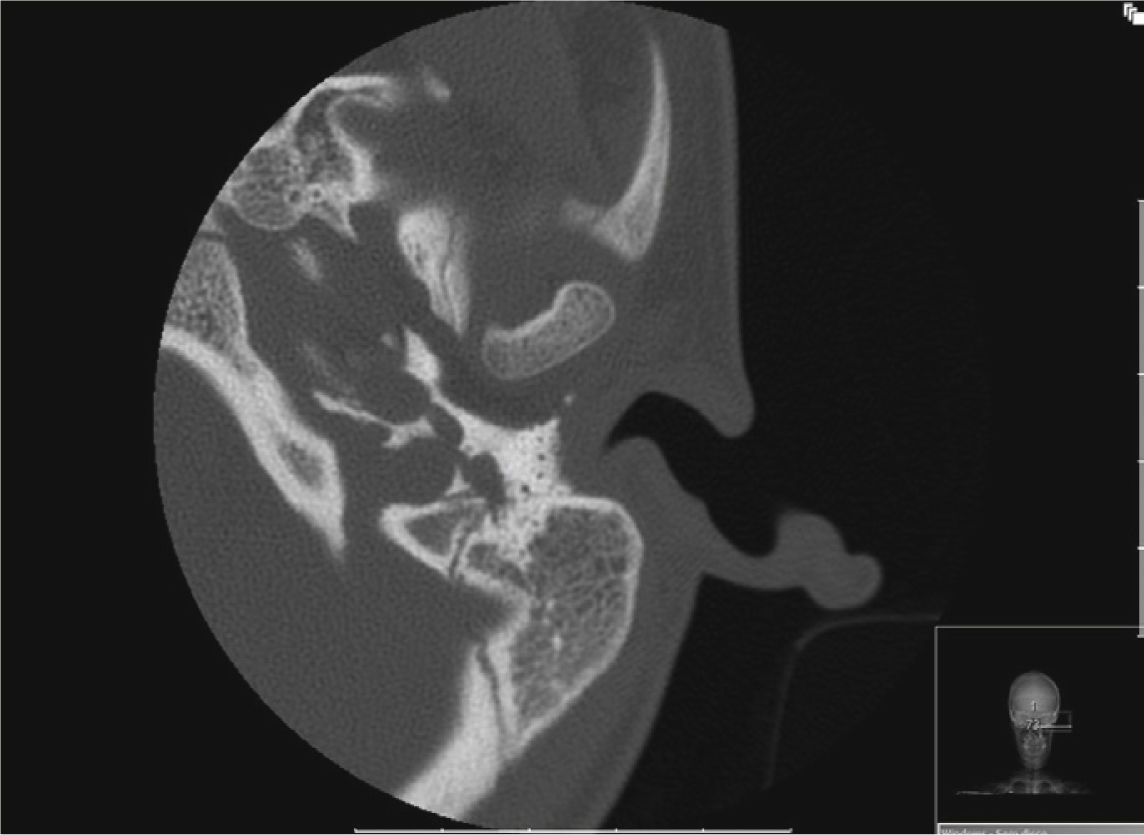
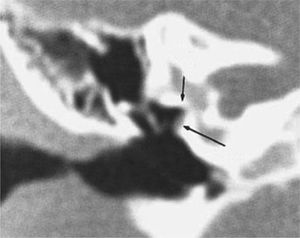
A CT was obtained, which revealed absence of left round window, stapes, and incus lenticular apophysis (Fig. 6). The remaining ossicular chain and incus-malleolar joint were maintained. The oval window was narrowed. Facial nerve canal dehiscence (Fig. 7) and persistent stapedial artery (Fig. 8) were also present. The right ear showed no significant alterations.
It was chosen not to perform auditory rehabilitation, with outpatient surveillance.
Case 4Female child, 8 years old, white, without a significant history, referred for an ENT consultation due to hearing loss. She had no recurrent AOM nor family history of deafness. On otoscopy, the outer ear presented no alterations.
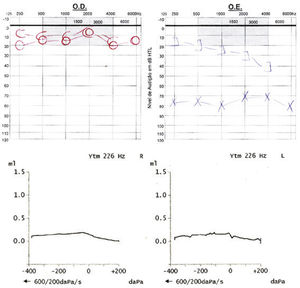
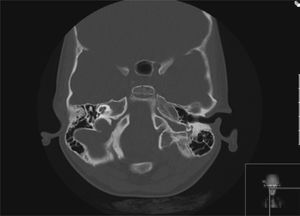
The audiogram revealed slight bilateral conduction hypoacusis (Fig. 9) and bilateral type C tympanogram.
A CT was conducted, which revealed bilateral fusion between the incus body and malleus head, hypoplasia of the oval window, and a high position of the jugular bulb on the right (Fig. 10).
As treatment, hearing rehabilitation with conventional prosthesis was chosen.
Case 5Female child, 12 years old, white, with a history of tonsillectomy at 3 years and bilateral myringotomy with ventilation tubes at 8, 9, 11, and 12 years. Referred for an ENT consultation with long-term hearing loss, without improvement from previous surgeries. She had no history of recurrent AOM nor of deafness in the family.
The objective examination of the external ear and an otoscopy showed no alterations.
The audiogram revealed an existence of conductive hearing loss (moderate to the left and severe to the right) (Fig. 11).
High-resolution CT showed the presence of long and lenticular apophyses of incus, bony blades into the oval window, and left round window hypoplasia (Fig. 12).
The patient underwent hearing rehabilitation with conventional bilateral hearing aids, resulting in auditory gain.
DiscussionAlthough the etiopathogenesis of most malformations of the middle ear is poorly defined, the knowledge of the embryology of this area allows for better understanding.
The stapes develops between the fifth and sixth week of embryonic development, with its origins in the second branchial arch (Reichert's cartilage), forming a ring that surrounds the stapedial artery. Between the seventh and ninth week, a depression in the otic capsule emerges, deep to the stapes footplate, in the future site of the oval window.12
The facial nerve, originating from the otic capsule and from cartilage of Reichert, develops in a temporal window identical to the stapes. The failure of fusing the two structures can lead to an anomalous facial nerve. The ossification of the facial canal is completed after the first year of life.13
In turn, the stapedial artery suffers atrophy around the tenth week. If persistent, it has its origin from the internal carotid artery. Generally this persistence does not generate symptoms, but may rarely be associated with a pulsatile tinnitus. This can be observed in the otoscopic exam, although in most cases the artery only is detected on imaging studies or during an exploratory surgery.14,15
The evolutive processes of the stapes, the oval window, and the facial nerve are clearly related, both temporally and spatially, which explains the concomitant abnormalities of these structures.
These deformities in the complex stapes/oval window can range from minor changes in the structure of the stapes to the complete absence of the oval window. In this latter case, there is invariably malformation or absence of the stapes, suggesting that the induction of the oval window may depend on the presence of that ossicle. The stapes fixation, especially at the level of its footplate, is the most frequent congenital anomaly of the middle ear.16
In 1993, Teunissen and Cremers proposed a classification that employs four major classes of minor anomalies of the middle ear. This classification is the most widely used worldwide, since it is based on a large series of cases and reflects the surgical aspects of the malformations.
The clinical cases reported previously correspond to minor defects, since there was never involvement of the external ear. Since there is consistently severe aplasia or dysplasia of the oval or round window, these cases correspond to Teunissen and Cremers class 4, the rarest and the most advanced stage of middle ear malformations. In these stages, an improper development of the stapes and an alteration of the course of the facial nerve are common. The persistence of the stapedial artery and the presence of a gulf in the high jugular, although rare, also occurred in the aforementioned clinical cases.
Other known non-ossicular malformations, although not identified in the studied cases, are congenital perilymphatic fistula and aberrant internal carotid artery.
In Teunissen and Cremers class 4, there is a significant change in the middle ear, which limits the conduction of sound to the inner ear. Surgical treatment, such as vestibulotomy with piston insertion, has a higher risk of facial nerve and inner ear injury, with consequent sensorineural deafness. As such, this option should only be chosen in very selected cases and by experienced surgeons.6,12,17,18 Auditory rehabilitation with conventional or BAHA prosthesis is a good therapeutic option in younger patients, or when reconstructive surgery is contraindicated.6
In contrast, in Teunissen and Cremers classes 1 and 2, it is possible to perform a stapedotomy with good long-term results.19–21 In class 3, tympanoplasty with ossicular chain reconstruction is a good therapeutic option.22,23
Auxiliary diagnostic tests are essential in patients with suspected hearing loss and middle ear malformations. An audiometry should be the first test requested in the functional investigation of these patients. Conversely, a high resolution CT scan is an option with good representation of the bony structures; it is more useful than MRI to demonstrate changes of the external and middle ear and mastoid. Where there is suspicion of congenital conduction deafness, it is recommended to perform a high-resolution CT scan. This examination, in addition to enabling the diagnosis of minor anomalies of the ear, can reveal abnormalities of the facial nerve, with exclusion of inner ear malformations or juvenile otosclerosis.12
ConclusionMiddle ear malformations are a rare cause of conductive hearing loss in children, especially when these conditions are not associated with malformations of the external ear. These anomalies are usually confused with serous otitis, because often there is a history of myringotomy with ventilation tube insertion prior to diagnosis.
Where there is a suspicion of congenital conductive hearing loss, obtaining a high-resolution CT in order to evaluate the bony structures of the middle ear should be considered.
In this condition, there is often a delay in diagnosis and treatment, which could cause delays in language and learning.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Esteves SDS, Silva AP, Coutinho MB, Abrunhosa JM, Sousa CA. Congenital defects of the middle ear - uncommon cause of pediatric hearing loss. Braz J Otorhinolaryngol. 2014;80:251-6.
Institution: Centro Hospitalar do Porto, Department of Otorhynolaryngology and Neck Surgery, Porto, Portugal.