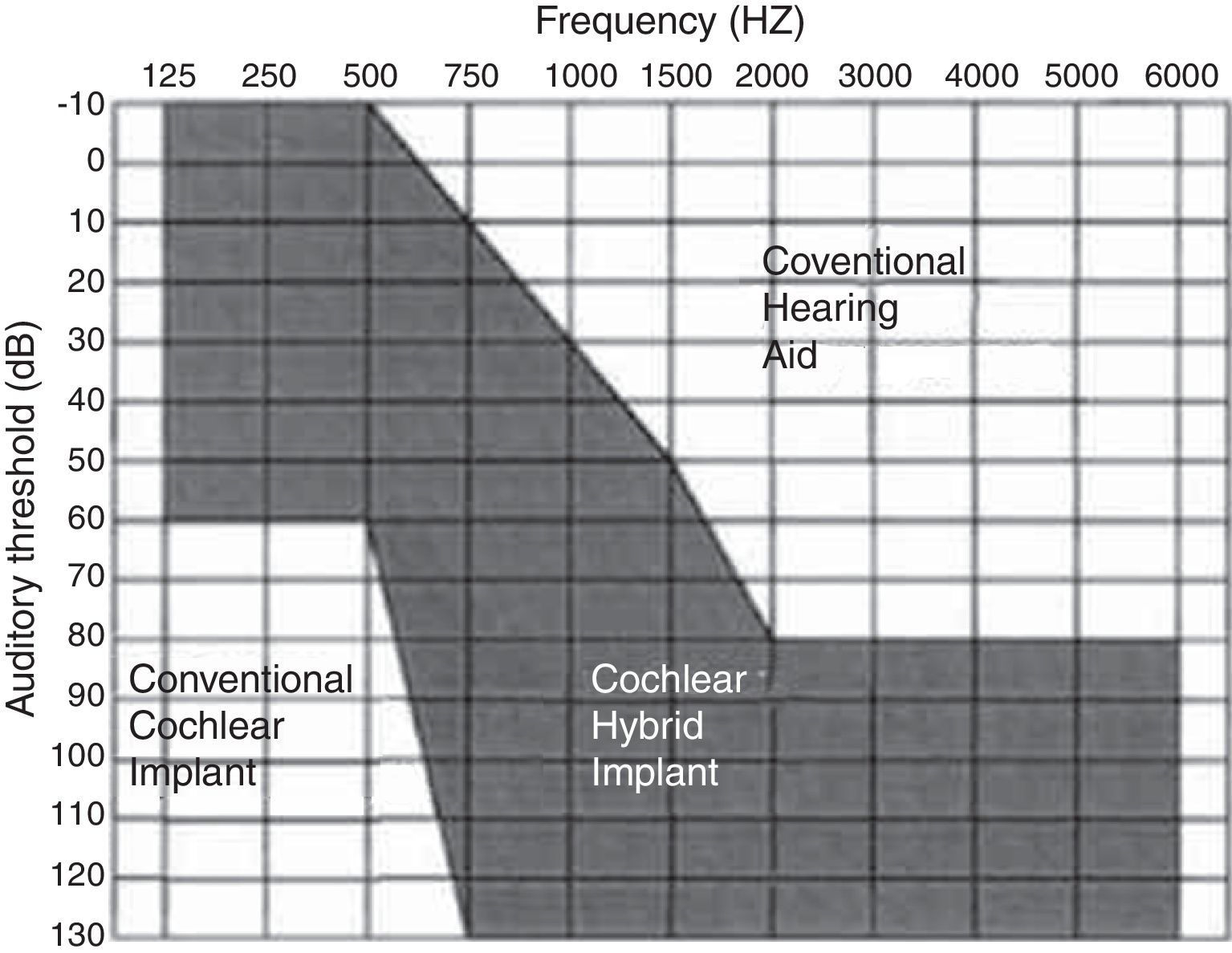
Electroacoustic stimulation is an excellent option for people with residual hearing in the low frequencies, who obtain insufficient benefit with hearing aids. To be effective, the subject's residual hearing should be preserved during cochlear implant surgery.
ObjectivesTo evaluate the hearing preservation in patients that underwent implant placement and to compare the results in accordance with the approach to the inner ear.
Methods19 subjects underwent a soft surgical technique, and the electrode MED-EL FLEX™ EAS, designed to be atraumatic, was used. We evaluated pre- and postoperative tonal audiometric tests with an average of 18.4 months after implantation, to measure the rate of hearing preservation.
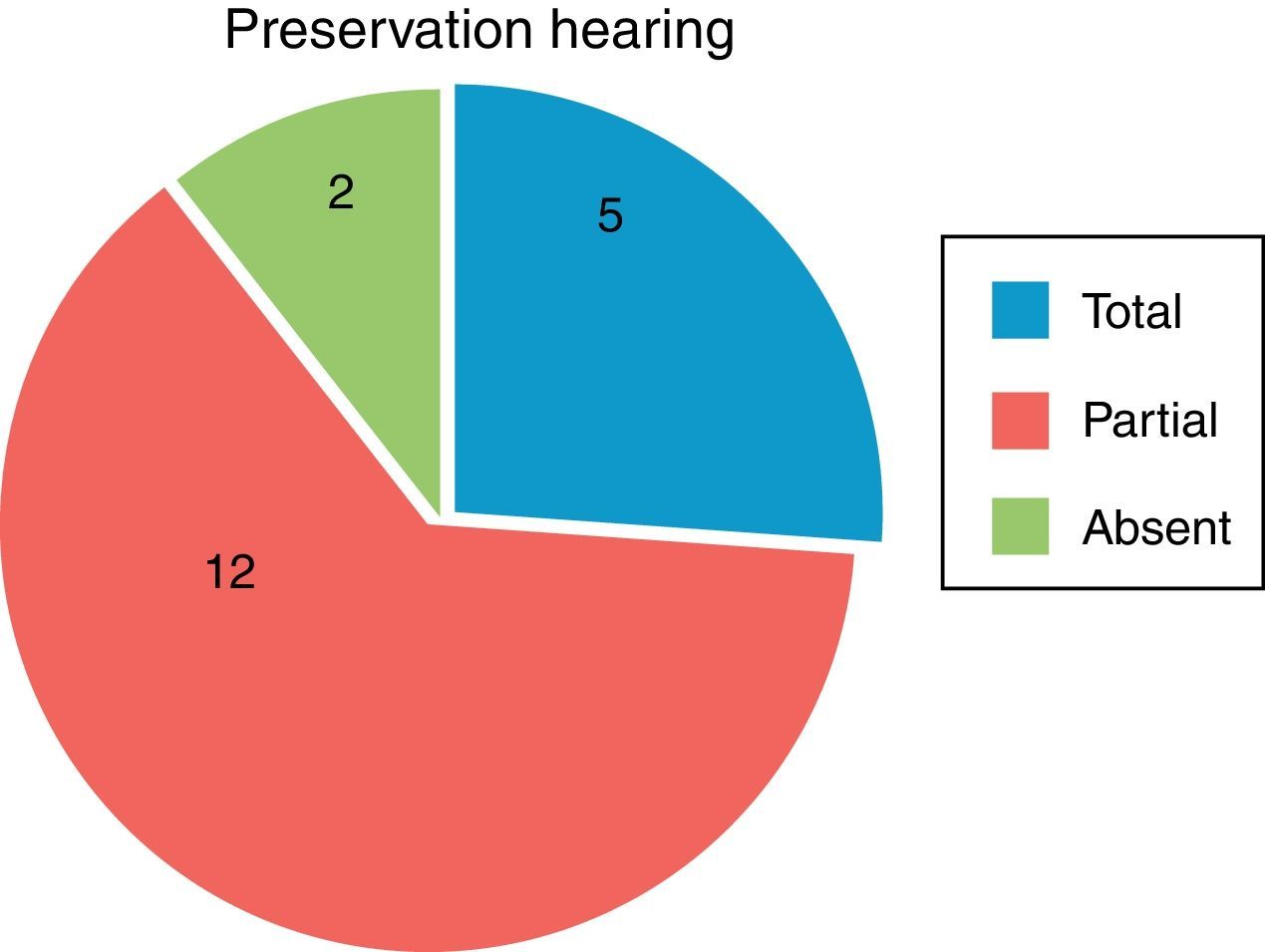
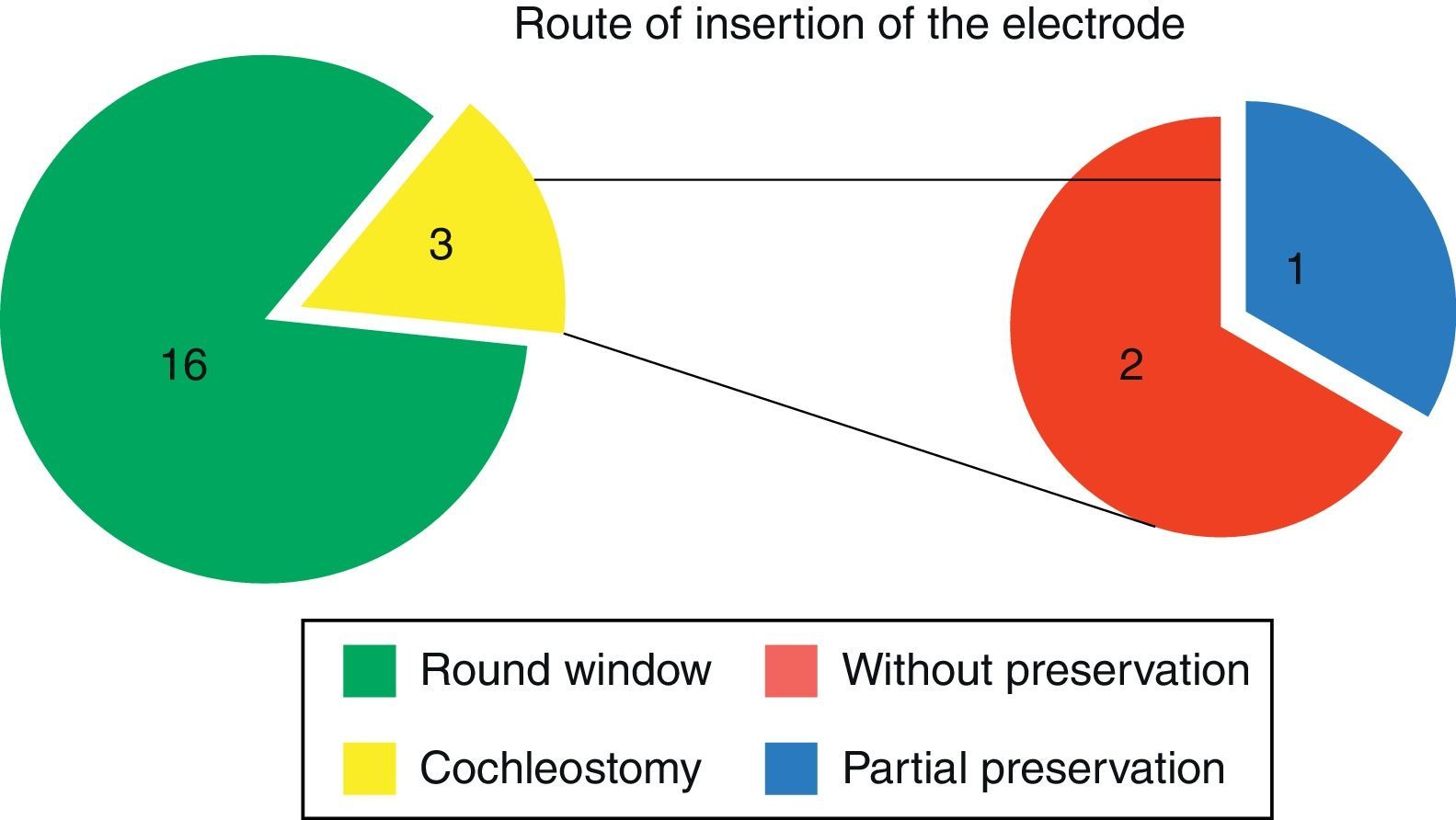
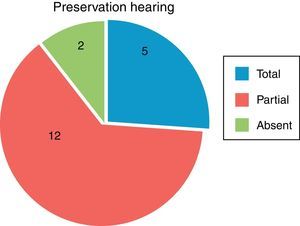
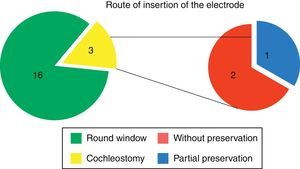
Results17 patients had total or partial preservation of residual hearing; 5 had total hearing preservation and two individuals had no preservation of hearing. The insertion of the electrode occurred through a cochleostomy in 3 patients, and in 2 of these there was no hearing preservation; the other 16 patients experienced electrode insertion through a round window approach. All patients benefited from the cochlear implant, even those who are only using electrical stimulation.
ConclusionThe hearing preservation occurred in 89.4% of cases. There was no significant difference between the forms of inner ear approach.
A estimulação eletroacústica é uma excelente opção para pessoas com audição residual nas baixas frequências, que obtêm benefício insuficiente com aparelhos auditivos. Para ser eficaz, a audição residual deve ser preservada durante a cirurgia de implante coclear.
ObjetivosAvaliar a preservação auditiva de pacientes implantados e comparar os resultados de acordo com a abordagem da orelha interna.
Método19 indivíduos foram implantados com uma técnica cirúrgica para preservação auditiva, tendo sido utilizado o eletrodo MED-EL FLEX™ EAS, concebido para ser atraumático. Foram avaliados os exames audiométricos tonais no pré e pós-operatório, com uma média de 18,4 meses após o implante para medir a taxa de preservação da audição residual.
Resultados17 pacientes tiveram preservação total ou parcial da audição residual; cinco obtiveram preservação da audição total e dois indivíduos não tiveram preservação da audição. A inserção do eletrodo ocorreu por cocleostomia em 3 pacientes; em 2 destes pacientes não houve preservação da audição. Os outros 16 pacientes foram submetidos à abordagem pela janela redonda. Todos os pacientes foram beneficiados com o implante coclear, mesmo aqueles pacientes que utilizando apenas estimulação elétrica.
ConclusãoA preservação auditiva ocorreu em 89,4% dos casos. Não houve diferença significativa entre as formas de abordagem da orelha interna.
Electroacoustic stimulation is an excellent option for people who have residual hearing at low frequencies, but not at high frequencies, and achieve insufficient benefits with the use of hearing aids. For an electroacoustic stimulation to be most effective, the patient's residual hearing should be preserved during cochlear implant (CI) surgery.
In recent decades, several electrodes were developed and refined in order to cause the least possible damage to the cochlear structures, thereby preserving residual hearing.1–4 However, for the preservation to be successful, in addition to an appropriate electrode, a special surgical technique is essential. After the earliest operations, in which a conventional cochlear implant electrode was partially inserted into the cochlea,5 the so-called “soft surgery” was developed, striving for a less traumatic operation. This surgery aims to preserve hearing, and many advances have occurred since then.6,7
The route for the introduction of the electrode into the cochlea is one facet of the surgical technique that has been especially studied and discussed.
Initially, insertion through the round window was the standard technique for hearing preservation surgery. This technique consists of a minimal incision through the membrane, with no need for drilling the cochlea, thereby reducing acoustic trauma and the possibility of bone fragments entering the scala tympani.8
However, a recently published study showed that the angle of insertion of the electrode is similar for both techniques (through the round window and by cochleostomy), and in both procedures, tissue damage will be minimal if an electrode designed for hearing protection is used.9 In a systematic literature review in 2013 comparing the two approaches, we could not find a single study specifically comparing insertion techniques; the levels of hearing preservation were similar between the two approaches, being slightly higher in patients undergoing insertion through the round window.8
Currently, such data comprise the largest case series of patients who underwent the technique of hearing preservation in cochlear implantation in Latin America. Furthermore, this group of patients has also been benefited with a longer postoperative follow-up.
Considering the importance of a deeper understanding of the factors that contribute to a higher rate of hearing preservation in patients who undergo cochlear implant placement, this study aims to assess the rate of hearing preservation in these subjects, and compare the results and the auditory performance of the patients according to the type of inner ear approach.
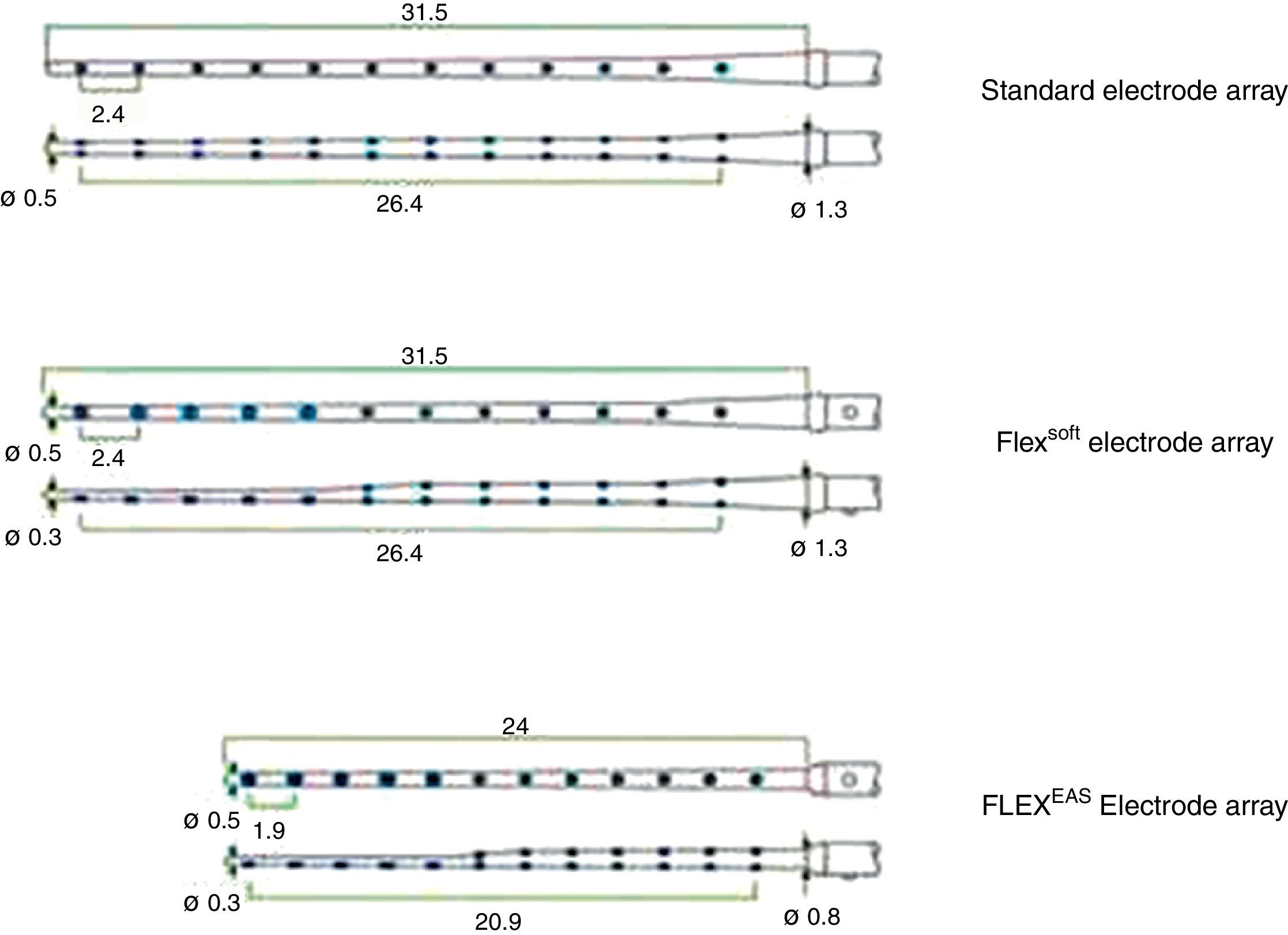
MethodsThis is a retrospective multicenter study of patients who underwent implant placement in the last four years at two specialized care institutions in Latin America; both centers employed the same surgical technique and used the same hearing preservation electrode designed to be atraumatic (MED-EL FLEX™ EAS).10
The surgical technique used was similar in all patients, and has been described in a previous publication.10
The general characteristics (age, gender, medical history) and audiological data (etiology of deafness, duration of deafness, sequential audiometric and speech tests, pre- and postoperative procedures) of patients were analyzed.
Inclusion and exclusion criteriaInclusion criteria were:
- –
Bilateral sensorineural hearing loss with little or no benefit with Personal Sound Amplification Devices (PSADs).
- –
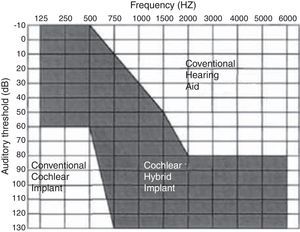
Pure tone thresholds better than 65dB at frequencies of 125, 250 and 500Hz, and worse than 80dB at frequencies above 1000Hz (Fig. 1).
- –
Auditory discrimination with monosyllables below 40% in the best possible sound amplification condition.
- –
A hearing loss, stable for at least the last two years.
Those patients who did not meet the criteria above were excluded from the study.
Implant usedThe implant used in all cases was the MED-EL FLEX™ EAS, with full insertion of the electrode bundle in all cases.
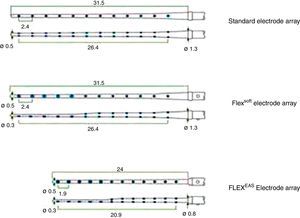
MED-EL FLEX™ EAS electrode has 24mm of overall length, with 0.8mm of diameter at its base and 0.3mm at its apex, with a 0.5-mm length tip. This device is provided with a cochlear coverage of about 1 ½ turn (Fig. 2), giving approximately 21mm of intracochlear stimulation length.
All patients used Sonata™, an internal component, adapted with a Maestro System™ software. Patients who received postoperative electroacoustic stimulation used Duet 2™, a speech processor. The group with purely electrical stimulation in the postoperative differed only in its speech processor; in such cases, OPUS 2™ was used.
Surgical treatment of inner earAt first, the introduction of an electrode through the round window was tried in all patients, but in those whose exposure of the round window niche was poor, a cochleostomy was performed for the insertion of the electrode. In each case, all steps proposed for hearing preservation were followed.10
It is noteworthy that, in cases where the exposure of the round window niche was not adequate via a posterior tympanotomy, a cochleostomy was chosen, without any instrumentation of the cochlear or round window region.
Hearing preservationTo determine the patients’ residual hearing, audiometric tests without electrical stimulation were performed as follows: on the date of activation one month postoperatively; at 3 months postactivation; at 6 months postactivation; and subsequently at every six months through follow-up. Preoperative tests up to two years before the treatment were also entered into the data set. Before the procedure the tests were also repeated on the day of surgery. For statistical analysis, the most recent preoperative examinations (on the date of surgery), as well as the latest postoperative assessment registered in these patients’ medical charts, were used.
The protocol included pure tone audiometry field tests with the implant on and speech tests, with standardization according to the rules of the institution.
“Residual hearing preservation” was defined in three ways:
- •
Total hearing preservation: 0–10dB of hearing loss postoperatively,
- •
Partial hearing preservation: >10dB of hearing loss postoperatively, while maintaining audiometric indices ≤80dB, at least at frequencies between 250 and 1000Hz,
- •
No hearing preservation: no benefit with the use of an EAS, by presenting a postoperative threshold without electrical stimulation >80dB.
This study was approved by the local Ethics and Research Committee.
ResultsNineteen patients were included in this study; nine patients underwent operation at institution 1, and 10 patients at Institution 2. Nine patients were female, and ten male ranging in age from 19 to 70 years, with an average of 48 years. All surgeries were uneventful and without complications.
Regarding the etiology of deafness in these patients, the following distribution was found: idiopathic etiology in 11 cases (57.8%), genetic etiology in 3 cases (15.7%; homozygous GJB2), and otosclerosis in two cases (10.5%). In the remaining participants, deafness was caused by trauma, neonatal hypoxia and chronic otitis media.
The mean time for the last postoperative audiometry was 23.6 months after completion of cochlear implant surgery, ranging from 4.5 to 81 months.
Of the 19 patients who underwent implant placement, in 16, the electrode insertion occurred through the round window, and in three cases by cochleostomy because of difficulty in getting adequate exposure of the round window niche. It is noteworthy that, of the three cases in which the insertion occurred through a cochleostomy, deafness had a genetic basis in two cases, and the third case had an idiopathic etiology.
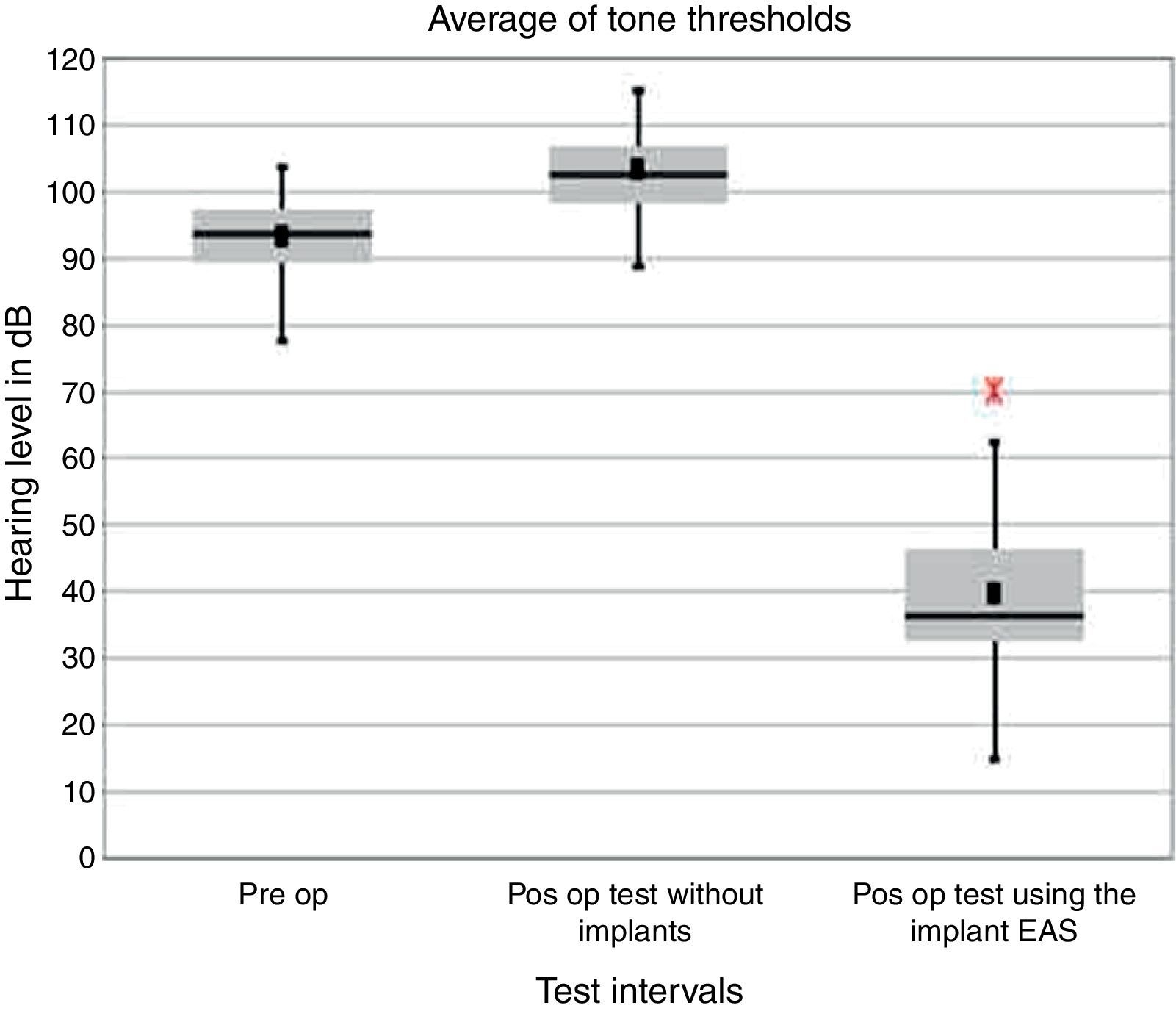
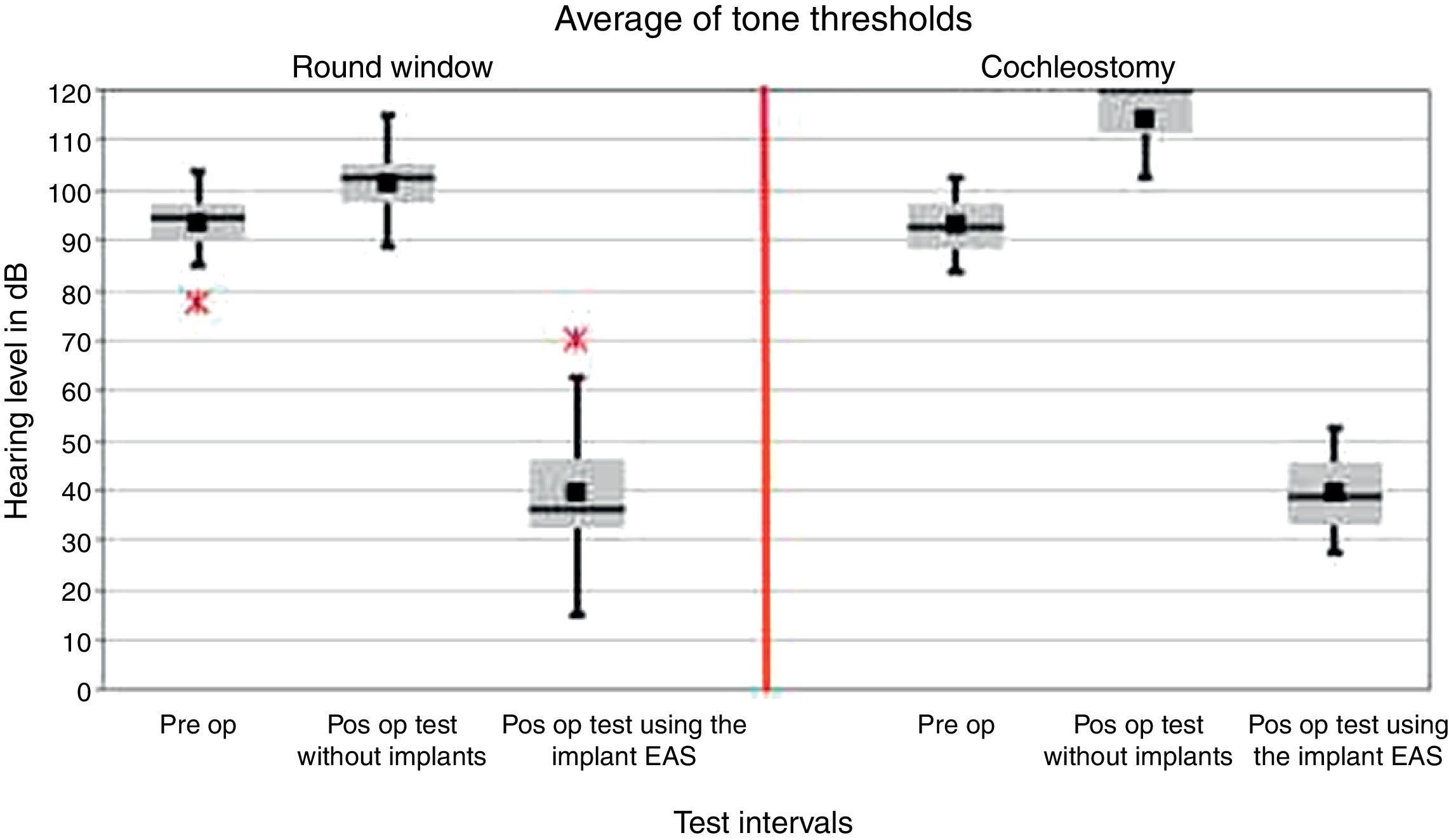
Five patients had complete hearing preservation; in 12 patients preservation was partial. In two patients, there was no hearing preservation (Fig. 3). Of the three patients who underwent cochleostomy, there was no hearing preservation in two cases, with partial hearing preservation in the third case (Fig. 4).
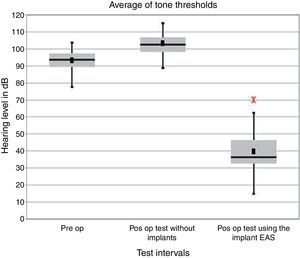
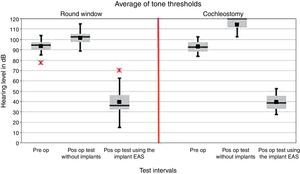
In all patients, the average tonal results of 500Hz, 1kHz, 2kHz, and 3kHz with the activated implant were higher than the preoperative audiometry results (p<0.001) (Fig. 5). The Kolmogorov–Smirnov test was performed prior to data analysis to verify the data distribution. Since our data showed an approximately normal distribution, a paired t test was used to test the difference between ranges of individual tests for the entire group.
Average pure tone audiometric thresholds (500Hz, 1kHz, 2kHz, 3kHz): comparison among preoperative tests, last postoperative test without use of a hearing aid, and last test using the implant (EAS) (hearing level in dB) (n=19). Mean values are shown as vertical black lines, medians as horizontal lines. Red asterisk represents outliers.
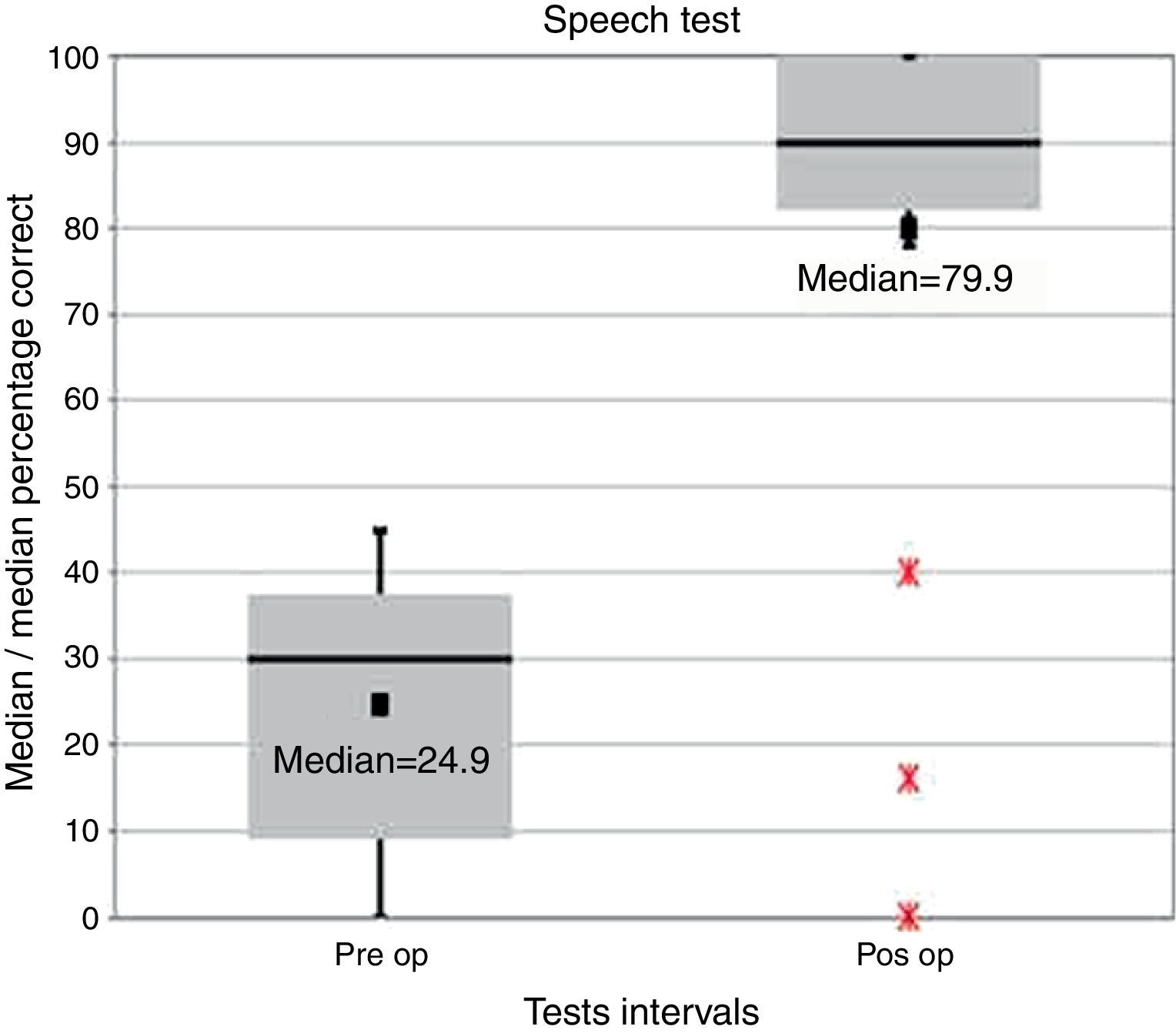
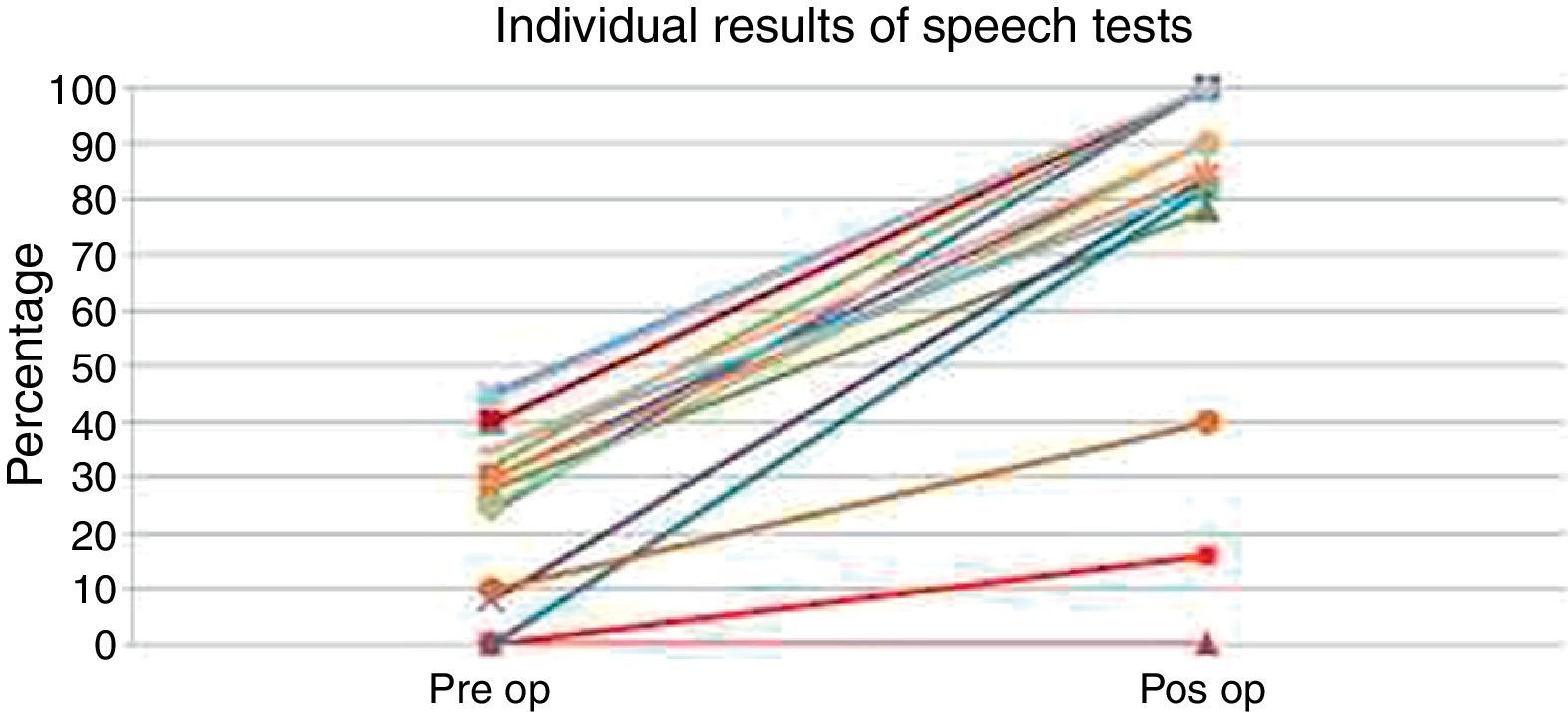
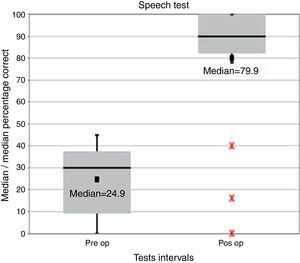
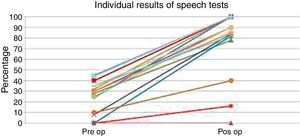
With respect to speech perception tests in silence, we noted benefit for patients from their cochlear implants (Figs. 6 and 7). As the speech perception tests’ distribution was not normal, the Wilcoxon Signed Rank test was used to test the difference between ranges of individual tests. The results showed a significant improvement in speech test performance for the entire group between preoperative versus postoperative tests (p<0.001).
For stratified analyses, the nonparametric Wilcoxon test was used. Individuals treated with the round window approach achieved a significant improvement in postoperative hearing thresholds with the EAS implant activated (p<0.001).
The improvement of postoperative pure tone thresholds in the group of patients with inner ear approach by cochleostomy was not significant (p=0.109) with the EAS implant activated. It is noteworthy that this group is numerically very small (n=3), which may be a bias (Fig. 8).
Average pure tone hearing threshold (500Hz, 1kHz, 2kHz, 3kHz): the graph shows the comparison between preoperative versus postoperative tests, with no use of the cochlear implant (hearing level in dB). The analysis was stratified by inner ear approach (Round window – n=16; Cochleostomy – n=3). Mean values are shown as vertical black lines, medians as horizontal lines. Red asterisk represents outliers.
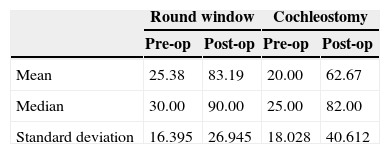
To check if there is a difference between the two inner ear approaches (round window versus cochleostomy) with respect to individual test intervals, Mann–Whitney U test was used. Thus, between the two inner ear approaches no significant difference was found in preoperative (p=0.866) and postoperative (EAS) (p=0.823) tests; however, a tendency to a significant difference in postoperative test with the implant activated (p=0.073) was observed (Table 1).
Regarding speech test results between the two inner ear approaches, participants treated with a round window approach achieved significant improvement in the performance of their speech tests between preoperative and postoperative tests (p=0.001). When comparing preoperative versus postoperative tests, the improvement for those patients treated with cochleostomy approach was not significant (p=0.109).
To determine if there was a difference in speech test performances between the approaches used with respect to individual test intervals, Mann–Whitney U test was utilized. Individuals treated by round window approach achieved higher performance scores on preoperative and postoperative speech tests, but the difference was not significant (preoperative test: p=0.499; postoperative test: p=0.206).
DiscussionElectroacoustic hearing stimulation aims to combine the amplification of a patient's residual hearing by means of conventional hearing aids, with cochlear electrical stimulation by performing a cochlear implant. Although there are still controversies about the real benefits of this combined stimulation, several benefits resulting from combined stimulation are described for patients with residual hearing and whose hearing was preserved, such as a good speech discrimination,11,12 better speech perception in noisy environments,12,13 improved music appreciation,14,15 and a better discrimination of different sound frequencies.16
Some classifications for hearing preservation have been proposed to assess the degree of preservation of residual hearing, and the most commonly employed is that proposed by Skarzynski,17 which was used in this study. Many factors are related to hearing preservation, for instance, the surgeon's experience, the electrode chosen,18 the speed of electrode insertion,19 the use of preoperative corticosteroids20 and the technique used. However, some steps in surgical technique seem to make no difference in the rate of hearing preservation,21 but, there is still controversy with respect to different routes for insertion of the electrode into the cochlea.8,22
Generally, hearing preservation occurs in 70–100% of implant technique patients.23 Only two of those patients who underwent implant placement lost all hearing; our overall hearing preservation rate was 89.4%. Only three of our patients underwent implant placement through a cochleostomy, because of difficulty to expose the round window; 66.7% of these patients did not realize hearing preservation, whereas in all cases of insertion through the round window the patients obtained complete or partial hearing preservation.
This was the first study assessing the hearing preservation of patients that underwent implant placement at the institutions of the authors. We believe that, with more experience with this surgical technique, we will be able to report higher rates of preservation of residual hearing. A more comprehensive monitoring and other types of speech tests are essential for a better evaluation of the results.
The improvement in postoperative pure tone thresholds in subjects treated with the cochleostomy approach to the inner ear was not significant (p=0.109) with an EAS-activated implant. This group had a small number (n=3) of patients, and this could represent a bias (Fig. 8).
In all 19 operated patients, independent of hearing preservation, the pure tone thresholds with an activated implant improved significantly; therefore, all patients have benefited from cochlear implants. A recent study involving patients with residual hearing who underwent implant placement also showed that all patients obtained better hearing outcomes and quality of life.24,25
This study has some bias, especially because of its methodological (retrospective) design. We also should mention a selection bias, since the cochleostomy group was formed as a result of an impossibility of accessing the inner ear through the round window. Thus, an asymmetry between the groups resulted, which could compromise the analysis.
Despite the limitations described, we consider the number of participants in the study as substantial, since they represent the largest number of cases in Latin America with the longest follow-up of these select patients. The reporting of these results will helps us achieve a greater understanding and comprehension of hearing preservation in cochlear-implanted patients.
ConclusionThe hearing preservation rate in patients with residual hearing submitted to a cochlear implant of MED-EL FLEX™ EAS was 89.4% (27% of overall preservation and 63% of partial preservation), with a tendency to a better preservation with the insertion of the electrode through the round window.
Regardless of hearing preservation, pure tone thresholds and speech tests improved in those patients with implant, either with electroacoustic stimulation or exclusively with electrical stimulation.
Conflicts of interestThe authors declare no conflicts of interest.
We thank all the patients and their families, the Unicom cochlear implant group (audiologists, social workers, nurse staff, psychologists, speech therapists and all staff), our Department (ENT, Head and Neck Surgery Department), and everyone at MED-EL team who helped us.
Please cite this article as: Guimarães AC, de Carvalho GM, Duarte AS, Bianchini WA, Sarasty AB, di Gregorio MF, et al. Hearing preservation and cochlear implants according to inner ear approach: multicentric evaluation. Braz J Otorhinolaryngol. 2015;81:190–6.
Institution: Universidade Estadual de (UNICAMP), Campinas, SP, Brazil; and Universidade Católica de Córdoba, Argentina.