Knowledge of the characteristics related to profound hearing loss is a matter of great importance, as it allows for the etiological and prognostic identification and strategic planning for public health interventions.
ObjectiveTo assess the different etiologies of hearing loss, age at diagnosis of the hearing loss, its relation to language acquisition, and the age at the first consultation in this service for cochlear implant assessment.
MethodsThis was a historical cohort, cross-sectional study, using retrospective analysis of the records of 115 patients with confirmed sensorineural hearing loss, who were followed in a university hospital, based on gender, age of hearing loss, age at the first consultation, language, and hearing loss etiology.
Results and conclusionThe majority of patients assessed for cochlear implants attend the first consultation when they are older than one year (an alarming mean of 3.8 years in the prelingual group) in spite of the early diagnosis of hearing loss. This reflects an already deficient health care system, in terms of referral. The idiopathic cause remains the most frequently identified. Among the known causes, the most prevalent are perinatal causes and meningitis.
O conhecimento das características relacionadas à perda auditiva profunda é de extrema importância já que permite a identificação etiológica e de fatores prognósticos e planejamento estratégico para intervenções de saúde pública.
ObjetivoVerificar as diferentes etiologias da perda auditiva, idade de diagnóstico da perda, relacionada ou não à aquisição de linguagem e idade dos pacientes ao procurar o serviço para a avaliação de implante coclear.
MétodoEstudo de casos, de coorte histórica transversal, com análise retrospectiva de arquivos de 115 pacientes com perda auditiva neurossensorial comprovada acompanhados num hospital universitário, com base em sexo, idade da perda, idade na primeira consulta, linguagem e etiologia da perda.
Resultados e conclusãoos pacientes avaliados para implante coclear chegam à primeira consulta, em sua maioria, com mais de um ano de idade (média preocupante de 3,8 anos no grupo pré-lingual), apesar de o diagnóstico da perda ser precoce, o que reflete um sistema ainda deficiente em termos de referenciamento. A causa idiopática ainda é a mais encontrada. Dentre as etiologias conhecidas, as mais prevalentes são as perinatais e a meningite.
Data from the last census conducted by the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatística – IBGE) in 2010 show that approximately 9.7 million Brazilians have hearing loss, which is severe in approximately 2 million individuals. There are more than 770,000 individuals with hearing loss among the population of Rio de Janeiro state.1
It is known that the prevalence of congenital hearing loss exceeds that of many diseases amenable to screening in childhood, such as phenylketonuria, sickle-cell anemia, congenital hypothyroidism, and congenital adrenal hyperplasia.2,3 A study conducted in 1998, at the beginning of the implementation of universal hearing screening, demonstrated that children with hearing loss who undergo intervention before 6 months of age to 3 years have rates of receptive and expressive language comparable to that of children with normal hearing, and that favorable prognosis in early intervention does not depend on the degree of hearing loss.4
Similarly, individuals with post-lingual hearing loss show progressive language deterioration according to the time of sound deprivation, which determines negative impact on their quality of life and indicates the need for early detection and auditory rehabilitation.
These data indicate the magnitude of hearing loss in the population and show the importance of early detection and referral of these patients for assessment, which allows for proper management and improved quality of life.
In this context, the importance of identifying the etiological cause of hearing loss is emphasized, as the process becomes more targeted toward the intervention and rehabilitation process.
In Rio de Janeiro, cochlear implant surgery by the Brazilian Public Health System (Sistema Único de Saúde – SUS) started in July 2011, and a total of 32 patients had received implants by March 2013.
The objective of this study was to assess the different etiologies of hearing loss, age at diagnosis of hearing loss, relationship to language acquisition (pre- or post-lingual), and age of patient when he/she presented to the service for cochlear implant assessment. With these data, the quality of hearing health care can be inferred, in order to promote the implementation of improvement measures.
Materials and methodsThis study was approved by the ethics committee of the institution under research protocol number 043/11 – CEP. A retrospective analysis of the records of 115 patients with proven profound sensorineural hearing loss referred for cochlear implant assessment at the otorhinolaryngology outpatient clinic of a university hospital between 2011 and 2013 was performed. The assessed patients were all submitted to tonal and vocal or behavioral audiometry, performed by the same qualified audiologist from this service, including otoacoustic emissions (OAEs) test and brainstem auditory evoked potential (BAEP) test carried out by experts in otolaryngology, computed tomography (CT), and magnetic resonance imaging (MRI) of the mastoids and auditory pathways.
Some patients who did not have a clear etiology for the hearing loss also underwent genetic testing in order to screen blood samples for the 35delG mutation, and were assessed by other specialties, as applicable. All were referred for hearing aid, whose criteria follow the recommendation of the Ministry of Health,5 and speech rehabilitation, in addition to assessments by a psychologist and a social worker. The criteria for cochlear implant indication followed those published by the Brazilian Association of Otolaryngology and Cervical-Facial Surgery.6
Patients who did not meet the criteria, or who had no indication or release by all professionals involved in the use of cochlear implants underwent follow-up at the Hearing Health Outpatient Clinic, which involves otolaryngologists and speech therapists, to maximize hearing gain and/or communication skills.
The data analyzed were gender, age, etiology of hearing loss, age at first consultation, and the type of hearing loss in relation to language acquisition (pre- or post-lingual). These were arranged in charts for statistical purposes.
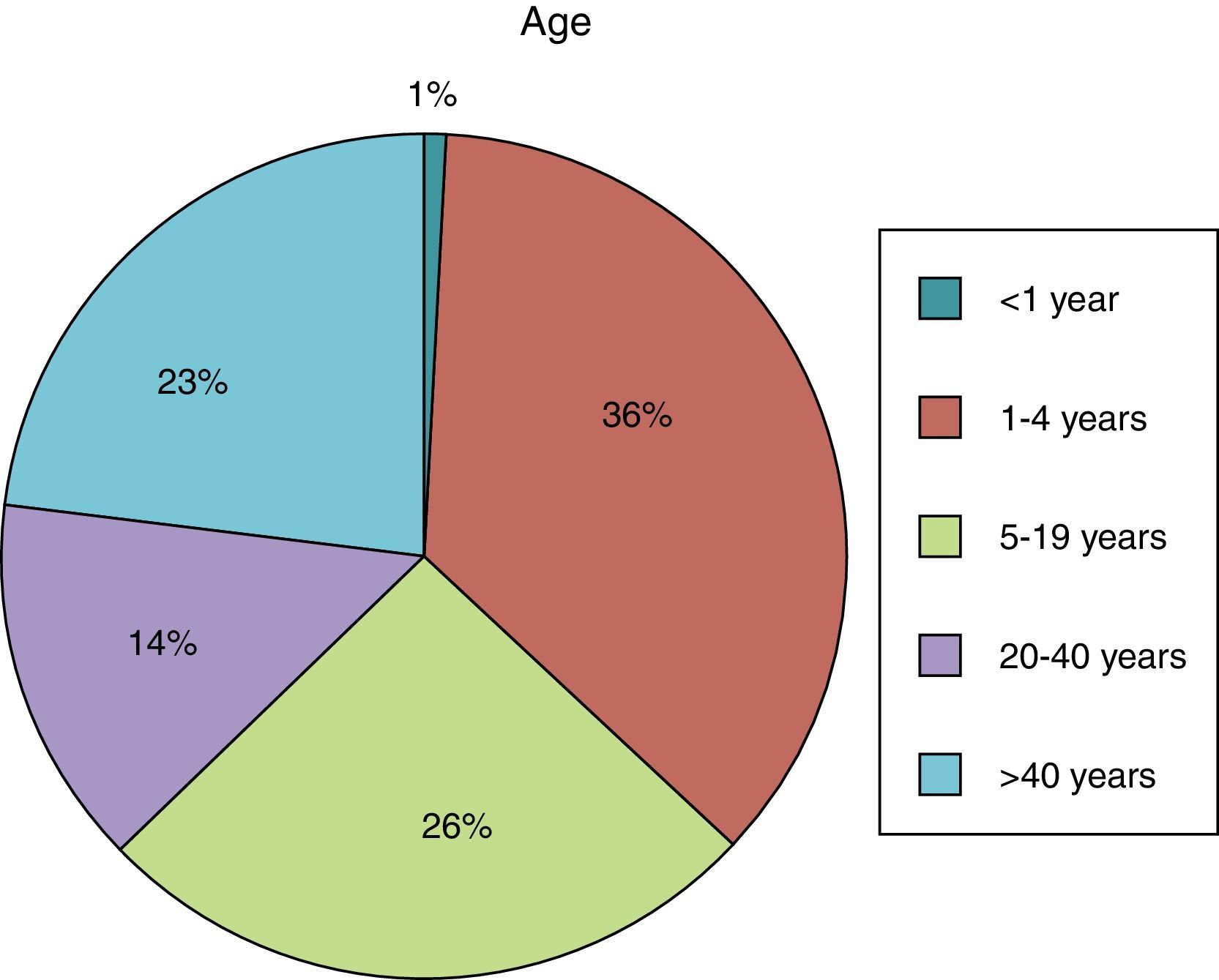
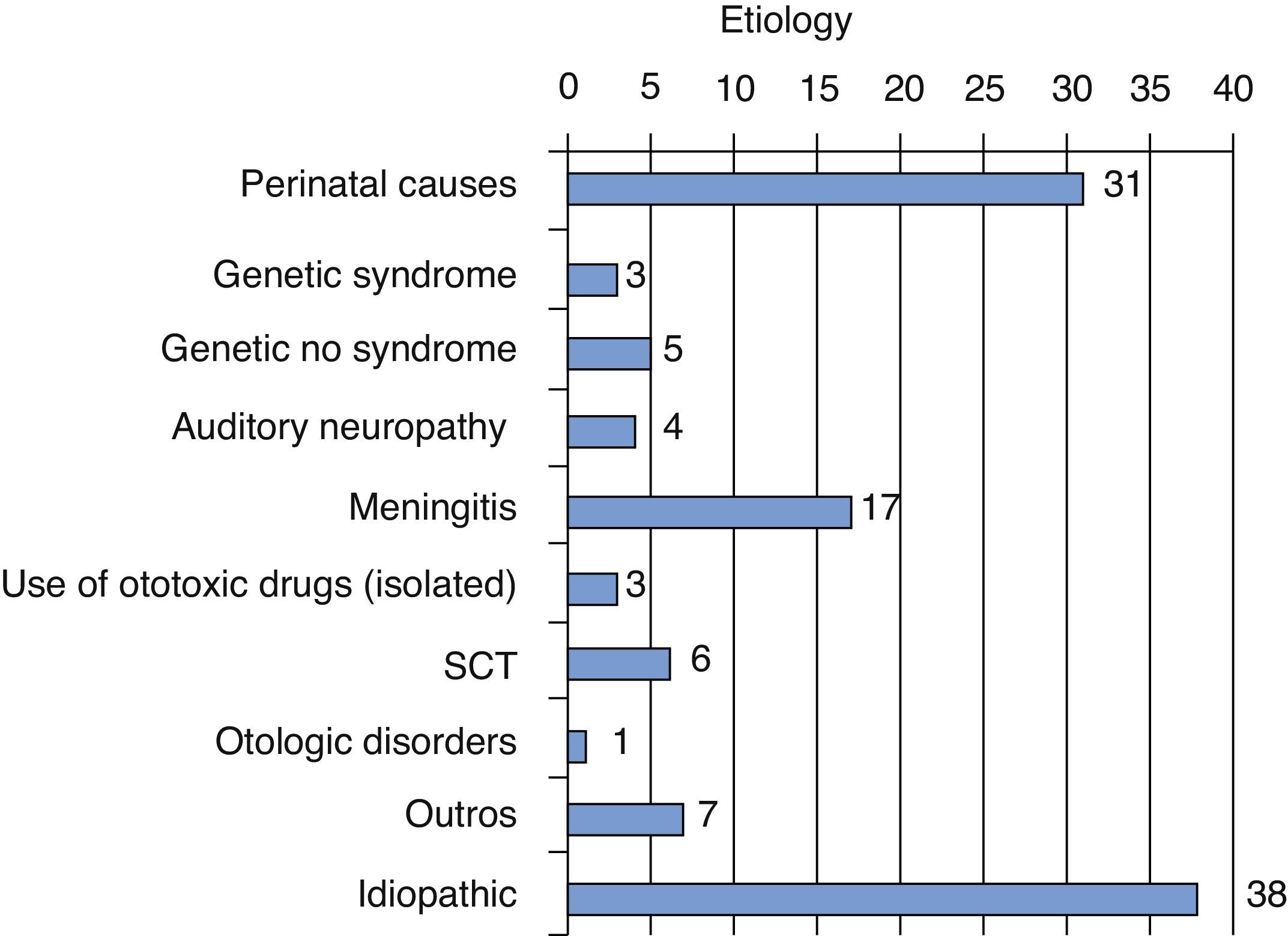
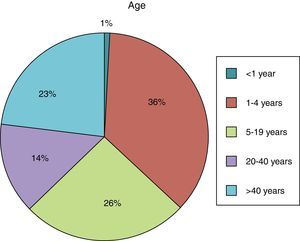
ResultsMost of the patients evaluated were aged 1–4 years, corresponding to 36% of the sample, followed by the age group 5–19 years (Fig. 1), and 53% of the patients were males.
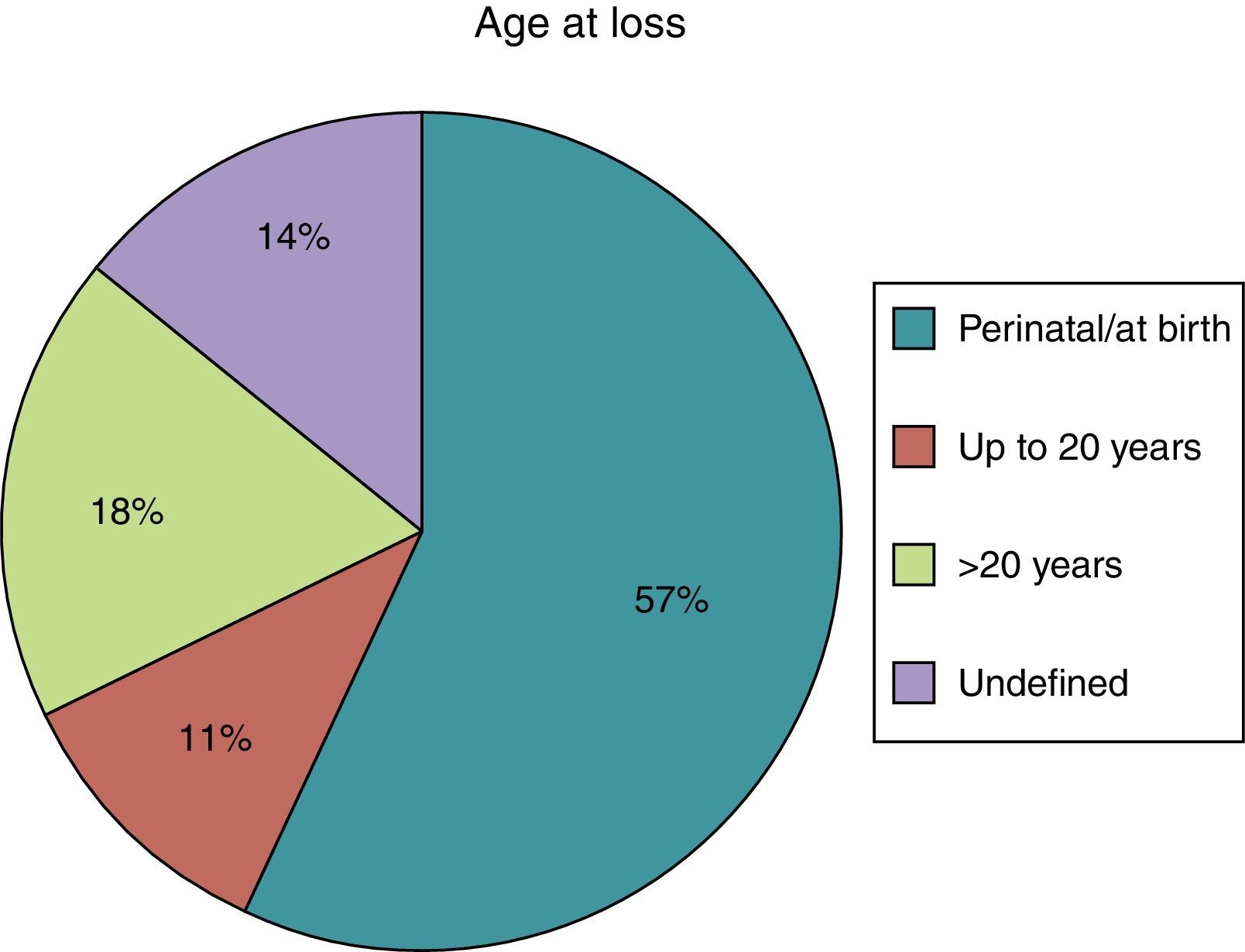
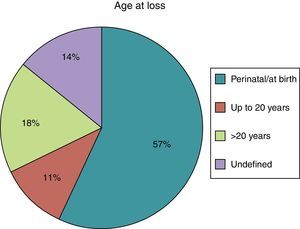
The age at diagnosis of hearing loss was the perinatal period in most cases (57%), whereas in 14% of cases the age at diagnosis of hearing loss was undetermined (Fig. 2).
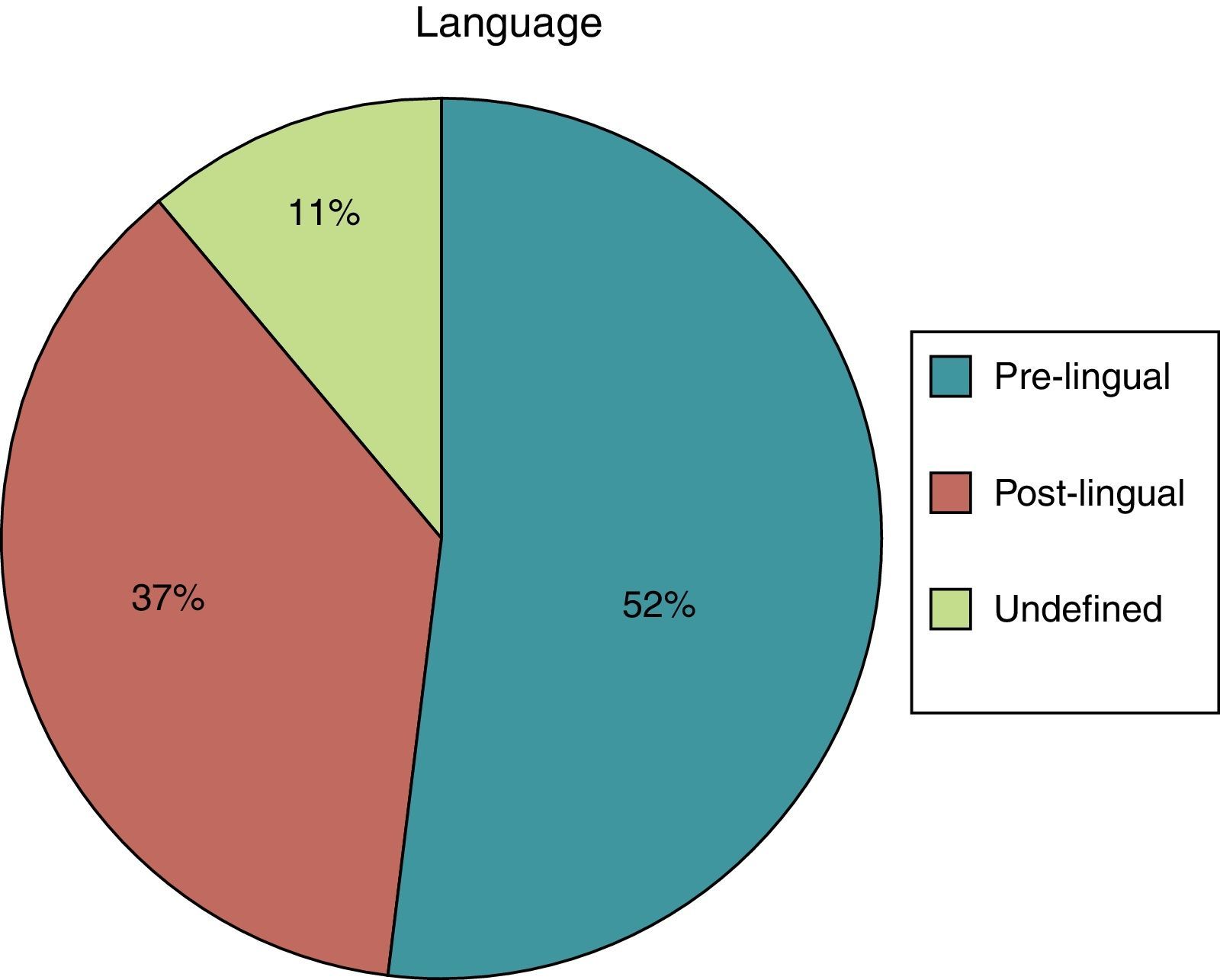
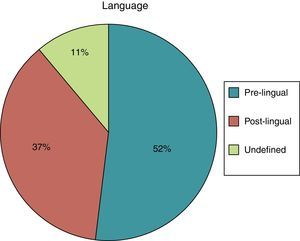
Of the assessed patients, 52% had pre-lingual hearing loss, 37% had post-lingual loss, and 11% had an undefined status (Fig. 3).
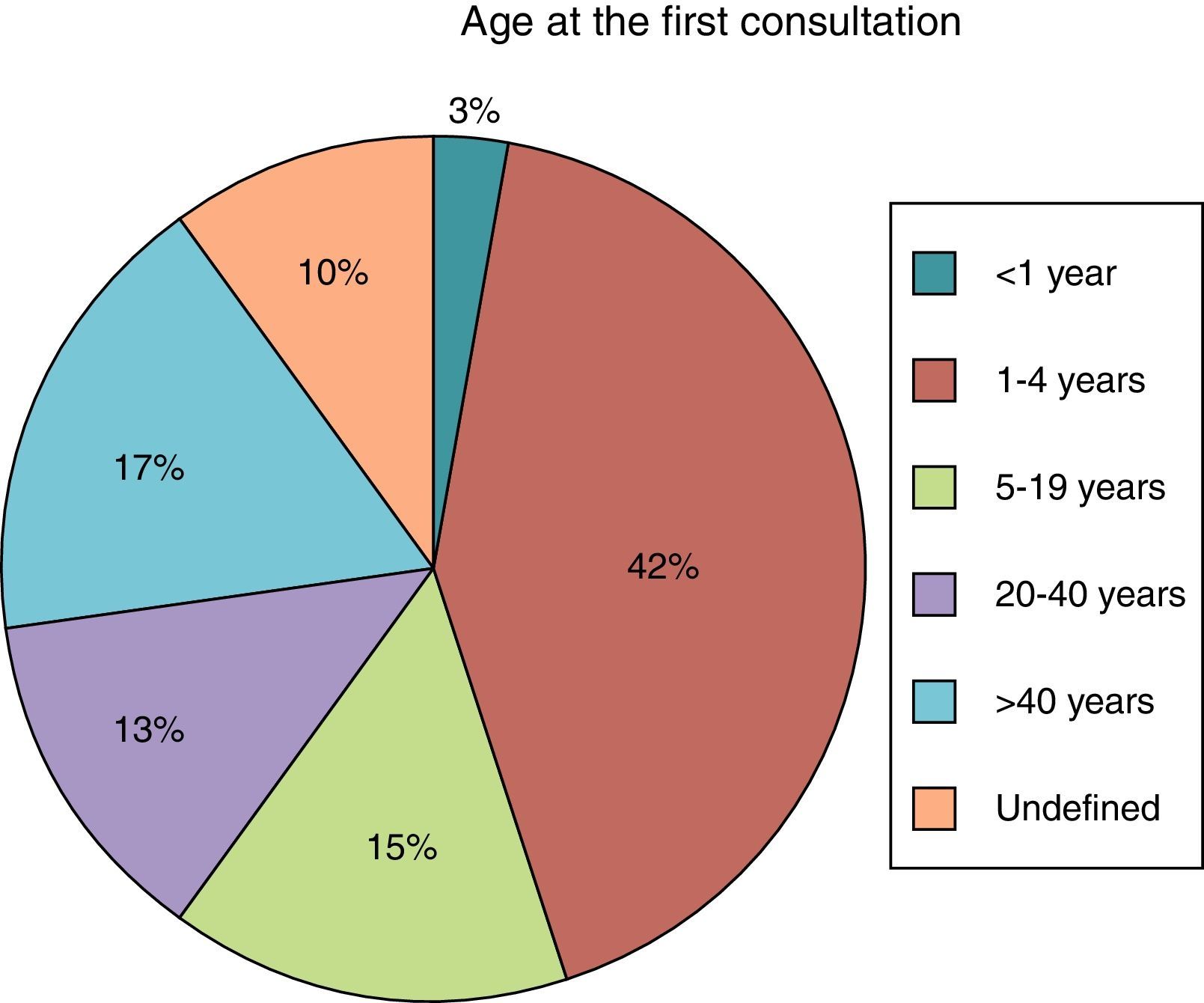
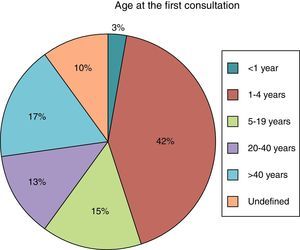
The age at first consultation at the hearing health outpatient clinic was mostly between 1 and 4 years, and only 3% of the patients were younger than 1 year (Fig. 4). In the group of pre-lingual patients, the mean age at the first consultation for hearing health assessment was 3.8 years.
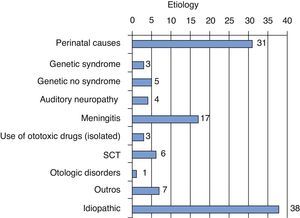
Of the 115 assessed patients, 31 had no defined cause for the hearing loss (33%). The most frequent known causes were of perinatal origin (27%) and meningitis (15%), as shown in Fig. 5.
DiscussionThe present study was conducted in the only public center that performs cochlear implant surgery in the entire state of Rio de Janeiro, Brazil. This center started cochlear implant procedures in July 2011, and by March 2013, 32 patients had received implants.
The assessment of candidates for cochlear implants includes stringent selection criteria, as well as complete patient history, physical examination or even genetic tests, and imaging studies, in addition to assessment by a psychologist, a speech therapist, and a social worker. With all these data, it was possible to analyze the profile of patients with profound sensorineural hearing loss evaluated for cochlear implantation in this outpatient clinic.
Correct selection of patients who will receive cochlear implants is essential to attain success, which requires a multidisciplinary approach, consisting of several stages and involving high costs and technology. Studies on patient selection criteria highlight the importance of standardization.7–10 It is necessary, however, that this assessment is performed efficiently and rapidly so that no time is lost until the surgery, as the period of auditory deprivation influences the performance of patients undergoing cochlear implantation.11–13
It was observed that most patients followed in this outpatient clinic were children between 1 and 4 years. Male gender predominance was also observed in other studies performed at the national level, as was an unknown etiology identified as the most common cause of hearing loss in the evaluated cases.7,14,15 According to Mehra et al.,16 in a review of several studies carried out in the United States from 1966 to 2007, in 56% of cases, the etiology of hearing loss was unknown. Among the known etiologies, genetic causes were the most prevalent. This is the same conclusion of an Australian study carried out in 2003.17
A study carried out in Nicaragua showed preventable causes of hearing loss as an important etiology in non-industrialized countries.18 In agreement with data observed by Pedrett and Moreira,15 perinatal causes, i.e., related to prematurity, neonatal ICU stay, low birth weight, neonatal hypoxia, hyperbilirubinemia, and consanguinity were the most prevalent known etiology in the present sample, without considering the use of ototoxic drugs, which in most cases are associated and are also, by themselves, a risk factor for hearing impairment. In other national studies, maternal rubella was found to be the main known etiology for the assessed hearing impairments;7,14,19 however, in this study, no patients with this etiology were identified.
This fact can be justified by adequate control of maternal rubella, based on vaccination campaigns for rubella implemented in our state, which in 2008 included men and other susceptible groups, and according to data from DATASUL, vaccination coverage remains high.20 However, it may be due to failure in the identification and reporting of individuals with congenital rubella syndrome, causing these cases to be allocated in groups with hearing loss of unknown or perinatal cause. This raises questions regarding the adequacy of epidemiological surveillance policies, and the identification and reporting of suspected or confirmed cases of the disease.
Meningitis was the third most prevalent etiology of hearing loss, which comprised 15% of the present sample. This is also shown in other studies as an important cause of severe/profound hearing loss,14,15,21 and depending on the degree of cochlear ossification, it can create a challenge to the introduction of the implant during surgery.22
Although the age at diagnosis of hearing loss in these patients is most often less than 1 year (57%, in the perinatal period), when they come for the first appointment, they are already between 1 and 4 years, an alarming mean of 3.8 years in the pre-lingual group, which corresponds to 52% of assessed patients. It is known that, ideally, referral to specialized hearing healthcare service should be performed as soon as the hearing loss is detected, in order to prevent social, emotional, and intellectual impairment.
According to Leal,7 the pre- and peri-lingual age range that benefits the most from cochlear implant is 0–3 years. In case of early intervention, these children can develop language and communication skills with a significant impact on their quality of life. A Brazilian study assessed the communicative skills in children undergoing cochlear implant through a translated and culturally adapted questionnaire answered by parents. It was concluded that the cochlear implant had a positive effect on quality of life of patients and their families, and that lexical development is the factor most associated.23 Other studies have shown similar results.11,24
Patients with post-lingual hearing impairment also have important functional outcomes with the implant. A study evaluating post-lingual patients ten years after surgery showed a positive impact; all assessed patients had finished college/university and were employed.25
However, based on the results of this study, the referral of these patients or their access to primary care appears to be deficient, and thus their first consultation at the specialized service will be delayed. This indicates the lack of dynamism of Brazil's public health care system, which has few specialized centers for the assessment of possible candidates for cochlear implants in consideration of the demands of this type of disability, and it raises questions regarding the organization of the referral and counter-referral system for patients treated in hearing healthcare centers.
It should be considered, especially in a context such as that of hearing health, which involves complex and interdisciplinary planning and technology, how the process of referral and monitoring of patients previously identified as having a disability can be made more efficient. This involves improved management and better communication between centers. Currently, computerized systems, used to organize the priority cases, are definitely feasible as a solution to solve the aforementioned problem.
ConclusionPatients with profound sensorineural hearing loss assessed for cochlear implant present for the first consultation at an age greater than 1 year (with a distressing mean of 3.8 years in the pre-lingual group, which corresponds to 52% of assessed patients), even though the loss is diagnosed at birth or in the perinatal period. This reflects an already deficient health care system with respect to prompt referral of these patients to the tertiary service.
Idiopathic etiology of hearing loss was still the most commonly identified, which indicates a limitation in terms of diagnosis. The most frequent known causes were perinatal causes and meningitis.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Barbosa MH, Felix F, Ribeiro MG, Tomita S, Pinheiro C, Baptista MM. Profile of patients assessed for cochlear implants. Braz J Otorhinolaryngol. 2014;80:305–10.